140 Influenza
Influenza is a zoonosis indigenous to waterfowl, with periodic introduction of the virus into humans and other mammals. The consequences of host species transfer from birds to humans can be devastating, with substantial mortality rates and rapid transmission by the respiratory route with global pandemic potential. The fate of influenza virus infection in human populations depends upon the viral virulence properties, immunologic differences from previous influenza outbreaks, fitness of the virus for replication and dissemination within humans, and status of the host immune defenses.1
In the winter months, severe disease in individual patients is usually limited to those with vulnerabilities in host defenses, including the very young, the very old, and individuals with immunodeficiency or underlying cardiopulmonary disease. The annual incidence rate varies each season depending upon the degree of antigenic “drift” (point mutations in coding regions of genes for major surface antigens) from one year to the next. However, influenza pandemics can occur following an antigenic “shift” (i.e., whole-scale reassortment of the influenza virus genome, with the expression of entirely new antigenic components), and these novel influenza hybrid viruses circulate throughout the entire susceptible global population. This set of events occurred in 2009 with the novel swine influenza virus strain where everyone, including healthy young people, became susceptible to this novel influenza infection and its complications.2
Even in a typical year between pandemics, influenza viruses account for the deaths of hundreds of thousands of people worldwide and exact billions of dollars from society in terms of morbidity and lost productivity. Recent estimates from the United States indicate that at least 610,660 life-years are lost, with 3.1 million hospital days, 31.4 million outpatient visits, and $10.4 billion in direct medical costs annually from influenza alone. The staggering amount expended for influenza care is $16.3 billion in projected lost earnings and an estimated total cost burden (including lost-life years) amounting to $87.1 billion.3 The total costs to society during a pandemic year such as 2009 are even higher and likely incalculable. The costs of intensive care services required for managing the most severely ill influenza victims alone are enormous.2
 Pathogenicity of Influenza Viruses
Pathogenicity of Influenza Viruses
Influenza virus is a single-stranded RNA virus of the family Orthomyxoviridae It affects birds and mammals and includes three genuses: influenza virus A, B, and C, based upon their matrix proteins.1,4 Influenza A virus is typically the most virulent, has pandemic potential, and leads to the most severe disease. Based upon the antibody response to two major antigenic proteins on the outside of virus, hemagglutinin (HA) and neuraminidase (NA), influenza A is subdivided into different serotypes including: H1N1 (responsible for Spanish flu in 1918, in addition to the 2009 flu pandemic); H2N2 (Asian flu of 1957); H3N2 (Hong Kong flu of 1968); H5N1 (the avian flu, often sited as the most recent pandemic threat), and a number of others currently less relevant to humans (H7N7, H1N2, H9N2, H7N2, H7N3, H10N7). The two other forms of influenza include B (which almost exclusively infects humans but is less common) and C (affecting humans, dogs, and pigs), which only rarely cause severe illness and epidemics in humans.5
A notable characteristic of influenza virus is the genomic structure consisting of eight separate single-strand segments, each encoding a single major protein to complete the synthesis of the mature virus. The RNA-based genome provides a high background mutation rate and gives the virus genetic plasticity. The multiple genome segments provide the substrate for reassortment of large sequences of RNA and permit hybrid viruses to form in hosts infected simultaneously by more than one virus strain. These events lead to whole-scale recombination of entirely novel hybrid viruses with new antigenic constituents (antigenic shift). As an example, the novel swine-origin influenza A/Mexico City/4/2009 (H1N1) outbreak strain was a quadruple-reassorted virus derived from gene segments originating from ducks, Eurasian swine, North American swine, and human-adapted influenza virus.6
Avian-adapted viruses can occasionally be transmitted to mammals, causing outbreaks in animals or giving rise to disease in human pandemics. The pig is an important “mixing vessel” host in shuttling avian influenza viruses to humans, as they can carry both avian and human influenza viruses.1 Porcine mucous membranes express a mixture of sialic acid–coated glycopeptides linked in a favorable conformation to bind both avian and human-adapted viruses. This is vitally important in the biology of influenza viruses, as the initial event in influenza infection is interaction of the hemagglutinin receptor to binding sites on host epithelial tissues. Avian species express α2,3-linked sialic acid–galactose disaccharides on their epithelial surfaces, and avian-adapted influenza preferentially binds to this linkage pattern. Human upper respiratory airways primarily express α2,6-linked sialyl-galactose surface receptors, and seasonal influenza strains in humans bind readily only to α2,6 linkages. Pigs, in contrast, normally express both α2,3- and α2,6-linked disaccharides on their mucous membranes, facilitating the opportunity for dual infections with avian- and human-adapted viruses.1,6,7
The lower airways and alveolar pneumocytes of humans actually express α2,3-linked sialylated glycopeptides, and viruses that bind efficiently to α2,3 linkages can cause severe pneumonia if deposited into the distal airways. Most seasonal influenza strains bind preferentially to α2,6-linked disaccharide hemagglutinin (HA) binding sites found in human upper airways. This usually leads to high transmission frequency by the airborne droplet nuclei deposited upon the upper airways, but a low risk of primary influenza pneumonia.8 The avian strain of H5N1 preferentially binds to α2,3 linkages and therefore is poorly transmissible from person to person, but it has the potential to cause severe pneumonia if delivered to the lower airways. Poultry workers in Asia in close proximity to infected livestock can occasionally receive enough viruses deposited into the distal airways to cause severe influenza pneumonia with a high mortality rate (60% to 70%).9,10
One of the explanations for the severity of the 1918 pandemic of H1N1 influenza was its HA that could bind with high affinity to both α2,6- and 2,3-linked sialyl-galactose moieties.11,12 The result of this unusual HA binding affinity was a highly transmissible virus with the capacity to replicate and cause severe disease in the lower airways. Disturbingly, the hemagglutinin of the 2009 outbreak strain of novel swine origin also bound with high affinity to both α2,6 and α2,3 linkages. Fortunately, influenza A Mexico City 4/2009 (H1N1) virus lacked the full complement of other known virulence factors of the influenza virus (Table 140-1), resulting an overall low case-fatality rate (<0.1 %). A further mitigating factor against mortality in older populations during the 2009 outbreak was the presence of already-existing memory cells with B-cell and T-cell epitope recognition sites in humans born before the early 1950s, induced by H1N1 viruses circulating in the first half of the 20th century.13
TABLE 140-1 Pathogenicity Traits and Virulence Factors of Influenza Viruses
| Viral Trait | Mechanism of Virulence | Comments |
|---|---|---|
| Epitope variations on HA and NA | Immune escape from recognition by pre-existing antibodies within the population from previous virus exposure | Antigenic drift (point mutations) leads to epidemics; antigenic shift (reassorted viral genomes) leads to pandemics |
| Cleavability of HA | HA undergoes proteolysis by host-derived proteases before receptor binding | Readily cleaved HA is associated with avid binding and disease severity |
| Binding preference of HA | α2,3-linked sialic acid receptor in alveoli and α2,6 linkage in upper airways | Viruses that bind to the α2,3 linkage or both α2,3 and α2,6 are more virulent |
| HA : NA ratio | NA cleaves sialic acid on glycopeptides on epithelium (binding site for HA) | Optimal ratio of NA and HA activity needed for high replication and release |
| NS-1 | This nonstructural protein inhibits host-derived interferons. | Mutation or truncated variants are associated with loss of virulence. |
| PB1-F2 | This peptide targets virus trafficking to mitochondria and induces apoptosis. | Mutations or truncated forms of PB1-F2 associated with loss of virulence |
| NA inhibitor resistance | H274Y mutation blocks NA inhibitor binding site and oseltamivir activity | Commonly seen mutation is seasonal H1N1 but rare in the 2009 outbreak strain |
| M2 inhibitor resistance | S31N mutation blocks activity of amantidine | Now commonplace in both H3N2 and H1N1 |
| PB2 temperature range | Polymerase activity at lower (mammals) and higher (avian) temperature | Broad Pol temperature range aids transfer from bird to human hosts |
H274Y, histidine substitution for tyrosine at amino acid at position 274; HA, hemagglutinin; M, matrix protein; NA, neuraminidase; NS-1, nonstructural protein; PB, polymerase basic; Pol, polymerase; S31N, serine substitution for asparagine at amino position 31.
 Clinical Manifestations and Complications of Influenza
Clinical Manifestations and Complications of Influenza
Classical seasonal influenza in adults is typified by a 4- to 5-day period of sudden-onset fever, chills, upper respiratory tract symptoms, headache, muscle pain, and weakness. Rhinitis is relatively uncommon and diarrhea is more common with influenza than with most rhinovirus upper respiratory tract infections. Severe complications and death can occur, especially in infants, the elderly, and individuals with chronic medical conditions. Among the most severe complications are primary influenza pneumonia and secondary bacterial infection leading to respiratory failure.14,15 Influenza can also cause central nervous system, cardiac, skeletal muscle, kidney, and hepatic complications.5,15 Underlying pulmonary disease is a frequent risk factor, occurring in 18% of patients, most commonly asthma (7%), followed by neurologic disease (12%), hematologic or oncologic (9.9%), and cardiac conditions (4.6%).16 However, approximately half of those hospitalized (rates ranging from 1-5/1000) for influenza are otherwise healthy.14–16
In the absence of a pandemic, 11% to 19% of patients hospitalized with laboratory-confirmed influenza require treatment in the intensive care unit (ICU).15 The mean duration of mechanical ventilation is approximately 5 days; the sickest patients require treatment with advanced techniques for the treatment of hypoxemia, such as high-frequency oscillatory ventilation (HFOV), extracorporeal membrane oxygenation (ECMO), prone positioning, and nitric oxide. These patients have an attendant increase in length of stay, duration of ventilation, and mortality.14,16,17
An estimated 50 to 100 million people died during the 1918 pandemic. Death followed from aggressive secondary bronchopneumonia, influenza-related lung disease with associated hypoxemia, and cardiac collapse.18,19 During the 1918 pandemic, there was unexplained excess influenza mortality in persons 20 to 40 years of age. This mortality increase may have been due to limited native immunity and/or a vigorous immune response directed against the virus in healthy young persons.18 Today the high mortality rate observed in the 1918 pandemic would almost certainly be reduced because of the availability of ICUs, vaccines, antibacterial agents, and antiviral medications. However, the cost would be a dramatic increase in critical care admissions and length of stay, assuming that this surge capacity is available. Long-stay ICU patients have significantly higher critical care and hospital mortality rates compared to short-stay patients, occupy a disproportionate number of critical care bed-days,4 and consume even greater resources.8 Sophisticated ICU care is often unavailable in developing countries today, and the case-fatality rates in these countries will probably be regrettably similar to the 1918 pandemic.20
 Influenza A 2009 H1N1-Related Epidemiology and Clinical Manifestations
Influenza A 2009 H1N1-Related Epidemiology and Clinical Manifestations
Since March 2009, influenza A 2009 H1N1 has spread from Mexico to virtually all countries of the world. By September 27, 2009, there were over 340,000 cases with 4100 deaths worldwide.7,21 The World Health Organization issued the first phase 6 pandemic alert of the century, anticipating substantial influenza transmission and related disease. Over the period of June to September 2009, there were dramatic spikes in H1N1-related disease in Australia, New Zealand, and South America that breached the capacity for ICU care in some regions. In Australian provinces, approximately 5% of the population developed H1N1-related illness, 0.3% of infected patients were hospitalized, and 20% of hospitalized patients required ICU care.22 In the Northern Hemisphere, an early and severe influenza outbreak occurred that was blunted in part by widespread deployment of an effective inactivated monovalent influenza vaccine program.23
The events that transpired in Canada were illustrative of the influenza situation in much of the Northern Hemisphere in 2009. Among 168 critically ill Canadian patients with influenza A 2009 H1N1, the mean age has been 32 years, with a possible predilection for more severe disease in women (67% of patients).24 Pregnant women in particular suffered from a disproportionate high level of influenza disease severity.25,26 Nosocomial transmission was the mechanism of acquisition in approximately 10% of patients. Hospital-acquired transmission to healthcare workers occurred early in the outbreak, but healthcare-related infection occurred at a low incidence rate once the pandemic was recognized and appropriate infection-control safeguards were instituted. One or more comorbidities were observed in nearly all patients, most commonly chronic lung disease such as asthma, chronic obstructive pulmonary disease, bronchopulmonary dysplasia (41%), obesity (33%, mean body mass index of 34.6 kg/m2), hypertension (24%), history of smoking (23%), and diabetes (21%). Similar clinical findings and predisposing illnesses were reported in other regions of the world during the 2009 outbreak.21,22,27,28 Serious comorbid illness was observed in only 30% of patients. Notably, aboriginal Canadians have thus far been over-represented (26% of patients). A summary of clinical risk factors and comorbidities associated with severe influenza complications is found in Table 140-2.
TABLE 140-2 Prognostic Indicators and Risk Factors for Severe Influenza Complications
| Risk Factors and Comorbidities | Comments |
|---|---|
| Age <5 years | Children < 2 years and those with chronic cardiopulmonary disease at greatest risk |
| Age >65 years | Poor vaccine response, poor host response to influenza infection |
| Chronic cardiopulmonary diseases | COPD, asthma, congestive heart failure |
| Metabolic disease and chronic liver disease | Diabetes mellitus and cirrhosis increase the risk of influenza complications. |
| Chronic neurologic illness | Neurocognitive and neuromuscular diseases associated with increased complications |
| Pregnancy | Particularly women in the third trimester |
| Obesity | BMI >35 kg/m2 increased the risk of influenza complications in the 2009 outbreak. |
| Hemoglobinopathy | Sickle cell disease patients at increased risk |
| Immunosuppression | Glucocorticoids, chemotherapy, HIV transplant recipients at increased risk |
| Children receiving salicylates | Increased risk of Reye syndrome |
| Aboriginal populations, poverty, poor access to healthcare services | Delayed treatment associated with increased risk of influenza complications |
| Secondary bacterial pneumonia | Bacterial pneumonia associated with longer ICU and hospital stays with more nosocomial complications and a greater mortality rate |
The typical clinical syndrome requiring ICU care among all age groups appeared to be a diffuse bilateral four-quadrant pneumonitis that was often rapidly progressive. This process accounted for over 80% of ICU admissions in Canada and elsewhere and often necessitated advanced ventilatory/oxygenation modalities including HFOV, inhaled nitric oxide, and/or ECMO therapy.24,29,30
Over 80% of patients with H1N1-related acute lung injury (ALI) received mechanical ventilation; very few patients were successfully managed with noninvasive ventilation strategies alone. Oxygenation support included high concentrations of inspired oxygen (mean admission PaO2/FIO2 147 mmHg), positive end-expiratory pressure (PEEP), frequent use of HFOV (12%), nitric oxide (14%), neuromuscular blockade (30%), prone ventilation (5%), and occasionally ECMO (7%). Medical therapies included neuraminidase inhibitors (90.5%), antibacterial agents (98.8%), and, despite uncertain efficacy, corticosteroids (50.6%).24
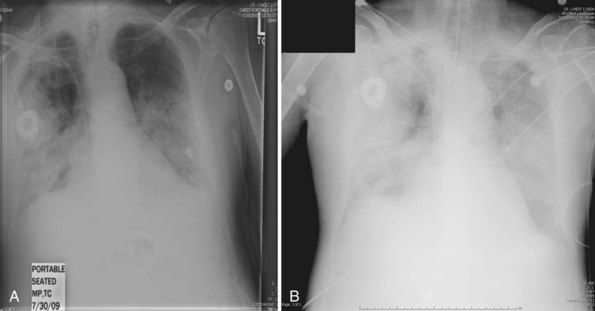
Secondary bacterial pneumonia following ICU admission was found in 24% of cases, most commonly due to S. aureus and S. pneumoniae. The frequency of secondary bacterial infection was difficult to accurately determine owing to the widespread use of empirical antibacterial therapy in influenza patients with rapidly progressive respiratory failure. Overall mortality among critically ill patients at 90 days was 17.3% (similar to that reported from Australia).22 The median duration of ventilation was 12 days. The most common cause of death was severe acute respiratory distress syndrome (ARDS) and hypoxemia, complications thereof, secondary infection, sepsis, or multiorgan dysfunction syndrome. Characteristic radiographic changes of severe primary influenza pneumonia are shown in Figure 140-1, A and B.
< div class='tao-gold-member'>

Full access? Get Clinical Tree