Indications for Upper Extremity Blocks
Jacques E. Chelly
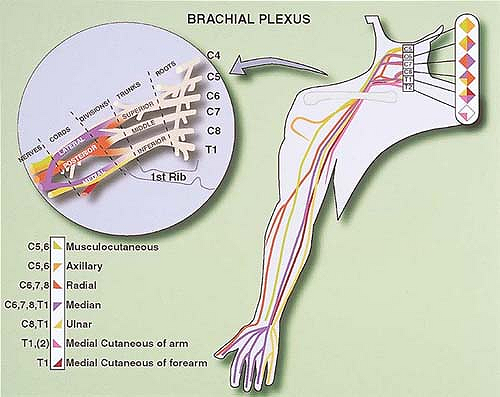
Regional anesthesia of the upper extremity is most frequently based on either a block of the brachial plexus (interscalene, supraclavicular, and classical infraclavicular) or a block of terminal nerves (median, ulnar, radial, and musculocutaneous nerves) at either the axilla (axillary block) or proximal part of the humerus (high-humeral approach). The choice of the approach often depends on the patient’s condition, the surgical indication, and the anesthesiologist’s experience. In this regard, it is important to recognize that for surgeries at the wrist and fingers scheduled for less than 30 minutes, a more distal approach either at the elbow or the wrist may satisfy all surgical requirements and allow for specific blocking of the nerve(s) implicated as well as for a preferential sensory block (at the wrist), preserving the motor function and allowing the patient to move his or her fingers at the request of the surgeon (release of trigger fingers). This “hyperselective” approach to regional anesthesia has been proven to be safe and effective and to facilitate rapid patient discharge after ambulatory surgery. For example, a short procedure on the fifth finger can be performed using a block of the ulnar nerve at the wrist. This technique is very quick to perform, satisfies all surgical requirements, provides effective postoperative analgesia, and allows the preservation of motor function not only of the thumb, index finger, and middle finger, but also of the fourth and fifth fingers. This chapter focuses on providing some rationales for choosing the most appropriate strategy for anesthesia and postoperative analgesia in patients undergoing upper extremity surgery.
Anatomic Considerations
A good knowledge and understanding of upper extremity innervation is essential to define the minimum anesthetic and analgesic requirements for a given indication, even if a more global approach is chosen because of other considerations (i.e., the anesthesiologist’s experience and the length of surgery), and even if ultimately the surgeon determines the technique. For example, a median, ulnar, and lateral cutaneous nerve block at the wrist represents the minimum requirement for anesthesia for carpal tunnel release, even if an axillary block is often performed.
Table 5-1. Most Common Anastomoses Between the Brachial Plexus Nerves | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Three factors need to be recognized when considering the role of anatomy in performing a peripheral block of the upper extremity: the level at which the nerves branch, anastomosis between nerves, and global innervation.
Level at Which the Nerves Branch
Each nerve of the brachial plexus divides into a sensory branch and a motor branch below the axilla, with a number of collaterals. For example, the radial nerve divides into a sensory and motor branch above the elbow crease, with the sensory branch running more superficially. The median and ulnar nerve divide into a sensory and motor branch above the wrist, whereas the musculocutaneous nerve supplies a motor branch to the biceps muscle and remains sensory thereafter. Consequently, a radial nerve block performed in the axilla results in a sensory and motor block of the posterolateral aspect of the forearm. In contrast, when the radial nerve is blocked at the elbow and below, the nerve has already divided into motor and sensory branches. Therefore, it is important to block the radial nerve 2 to 3 cm above the elbow crease, especially when using a nerve stimulation technique. The same is true when blocking the median nerve at the wrist: The motor and sensory fibers are distinctly separated. In addition, at the wrist, the median and ulnar nerves provide collateral sensory fibers to the anterior and medial aspects of the wrist, respectively, which originate above the wrist. Consequently, blocking these nerves at the level of the wrist crease produces only incomplete blocks. Wrist blocks need to be performed at least 4 cm above the wrist crease.
Anastomosis Between Nerves of the Brachial Plexus
Anastomosis between the nerves constituting the brachial plexus is frequent and may explain, at least in part, individual variations after a nerve block. To increase the reliability of the block, it is necessary to take this factor into consideration, especially when considering the use of specific distal blocks (see Table 5-1, which lists the most frequent nerve anastomoses).
Global Innervation
Although in most representations of the upper extremity innervation is based on superficial distribution, it is important to recognize that the muscular and bone innervation is not strictly superimposed (Fig. 5-1). The only location at which a single nerve innervates all structures is the lateral edge of the hand and the fifth finger, both of which are innervated by the ulnar nerve. There are some significant differences between the superficial, muscular, and skeletal innervations. These differences must be taken into account in determining the most appropriate block(s) for a specific surgical procedure. Thus, the surgical exploration of a second interdigital wound requires radial and median blocks, whereas an ulnar block is also necessary if interosseous muscle exploration is indicated.
Extent of Upper Extremity Blocks
Upper extremity nerve conduction can be interrupted at the level of the brachial plexus or the individual nerves. Approaches to the brachial plexus include the interscalene, subclavicular,
infraclavicular, and axillary blocks. Other blocks of the upper extremity are high humeral, elbow, wrist, and digital blocks. Each injection site is associated with a defined probability of achieving a complete block for a given nerve. The orientation of the plexus vis-à-vis the injection site is an important factor to take into consideration. Although experience is an important determinant of success, the extent of the sensory and motor blocks also depends on the site at which the block is performed. To maximize the correlation between the block resulting from the use of a given approach and the surgical requirements, it is important to choose an approach with the highest probability of producing a complete block in the surgical territory. This can only be achieved by gaining experience in the different approaches. Finally, when using peripheral nerve blocks as the main anesthesia technique, it is also important to account for all surgical requirements, such as the prevention of tourniquet pain, especially if the tourniquet is placed at the level of the arm and the surgery lasts more than 30 minutes.
infraclavicular, and axillary blocks. Other blocks of the upper extremity are high humeral, elbow, wrist, and digital blocks. Each injection site is associated with a defined probability of achieving a complete block for a given nerve. The orientation of the plexus vis-à-vis the injection site is an important factor to take into consideration. Although experience is an important determinant of success, the extent of the sensory and motor blocks also depends on the site at which the block is performed. To maximize the correlation between the block resulting from the use of a given approach and the surgical requirements, it is important to choose an approach with the highest probability of producing a complete block in the surgical territory. This can only be achieved by gaining experience in the different approaches. Finally, when using peripheral nerve blocks as the main anesthesia technique, it is also important to account for all surgical requirements, such as the prevention of tourniquet pain, especially if the tourniquet is placed at the level of the arm and the surgery lasts more than 30 minutes.
Brachial Plexus Blocks
Interscalene Block
With an interscalene block, the brachial plexus is approached at the level of the trunks or roots. The anatomy of the plexus relative to the site of injection with this approach explains why the upper (C5-6) and middle (C7) trunks are preferentially blocked. The lower trunk (C8-T1), which is more posterior, is often blocked incompletely. Consequently, the shoulder and the lateral aspect of the upper arm represent the territory with the highest probability of block. In addition, the proximity of the phrenic nerve, the large volume of local anesthetic usually injected (40 to 50 mL), and the diffusion of the local anesthetic solution toward the cervical region explain why the phrenic nerve, which runs anterior, is also almost always blocked and why the sensory block may extend up to C2 (Fig. 5-2).

Full access? Get Clinical Tree