Indications for Peripheral Nerve Blocks
Jeff Gadsden
Introduction
During the past 20 years, increasing knowledge in functional regional anesthesia anatomy, coupled with new technologies for locating peripheral nerves, has resulted in expansion of regional anesthesia techniques. This phenomenon served to provide the clinician with a wide variety of techniques from which to choose. Nevertheless, many nerve block techniques are quite similar and result in a similar, if not exact, distribution of anesthesia. The proper choice of the nerve block for a particular surgical procedure and/or patient, however, is far more important than deliberation on the minutia of various technical techniques. In this chapter, a rational selection of the nerve block techniques is approached in three sections. In the first section, indications for common nerve blocks are listed with a short summary of the advantages and disadvantages of each technique selected. In the second section, specific protocols for intraoperative anesthesia and postoperative analgesia for the common surgical procedures are suggested as practiced by anesthesiologists affiliated with the St. Luke’s and Roosevelt Hospitals in New York. This cookbook approach was chosen to allow clinicians to duplicate the results that we have found, via trial and error, to work best in our own practice. The last section is a more comprehensive compendium of published medical literature on the indications for peripheral nerve blocks.
Section I: Advantages and Disadvantages of Specific Nerve Blocks
Upper Limb Blocks
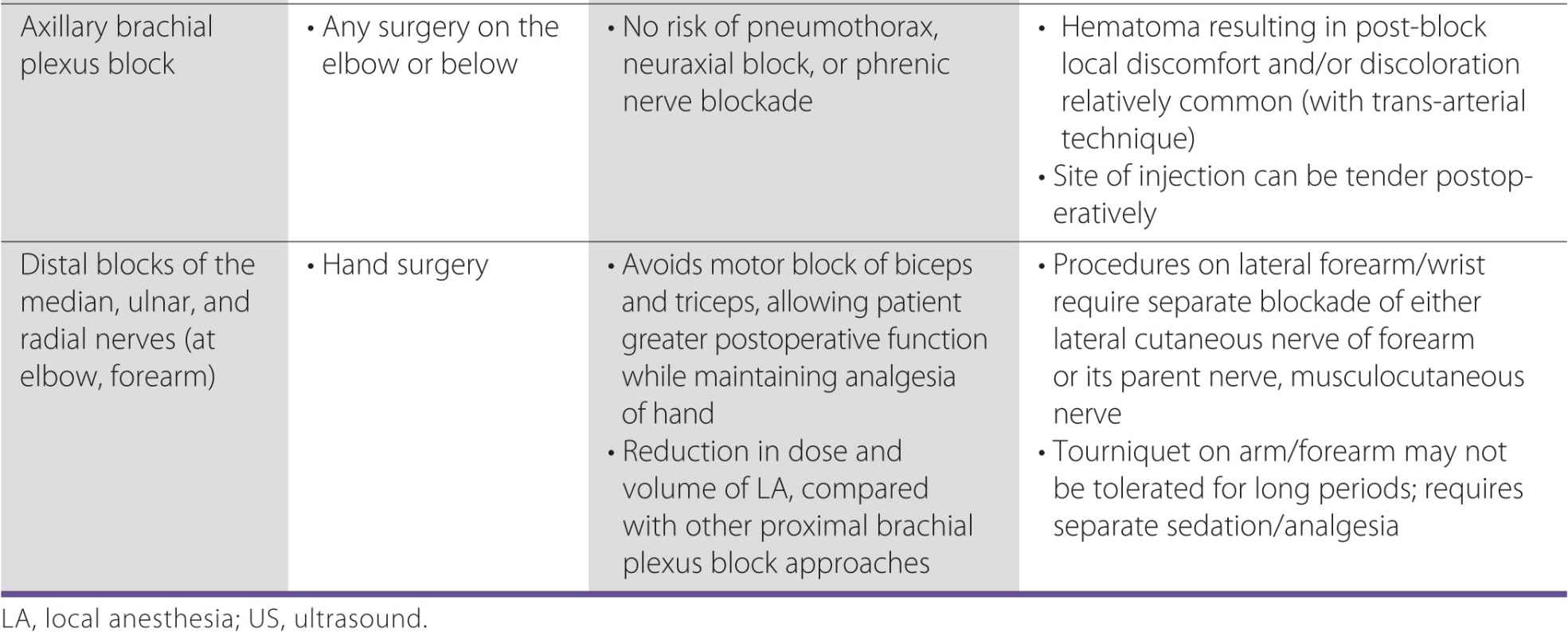
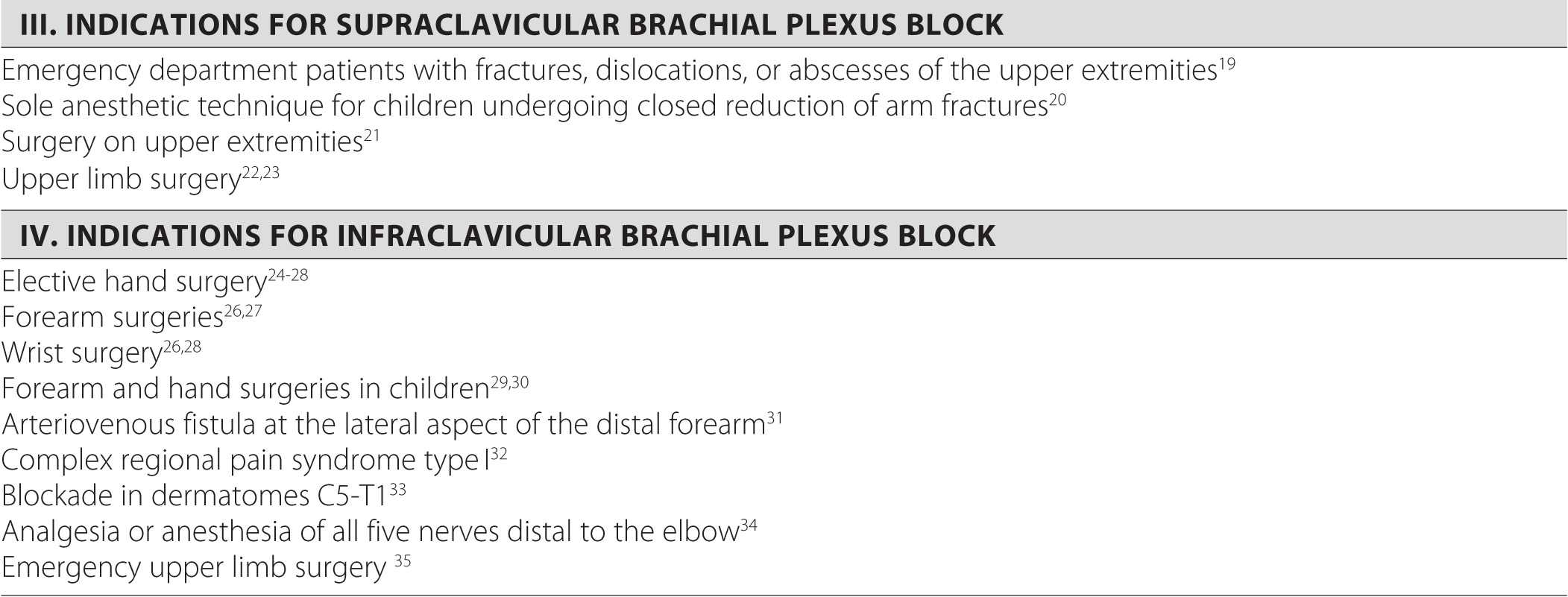
With the advent of ultrasound guidance for nerve blocks, the choice of which brachial plexus block to perform has become less relevant because the block can be extended by needle repositioning into the desired area. For example, the interscalene approach was not recommended in the past for procedures on the hand or elbow because it was believed that local anesthetic would not sufficiently cover the inferior trunk of the brachial plexus. However, this barrier can be overcome with the use of a low-interscalene approach or by using sonographic guidance to target all three trunks. Multiple injections at different levels of the brachial plexus through a single-needle insertion site can make the interscalene brachial plexus applicable for most upper limb procedures. Regardless, the common approaches to brachial plexus block are sufficiently different in their anesthetic coverage to deserve knowledgeable consideration when making a decision about which block to use. In addition to the anesthetic coverage, the block selection should also take into consideration other factors, such as patient comfort, preexisting respiratory dysfunction, and practitioner experience. Table 6-1 lists common nerve block procedures and their indications.
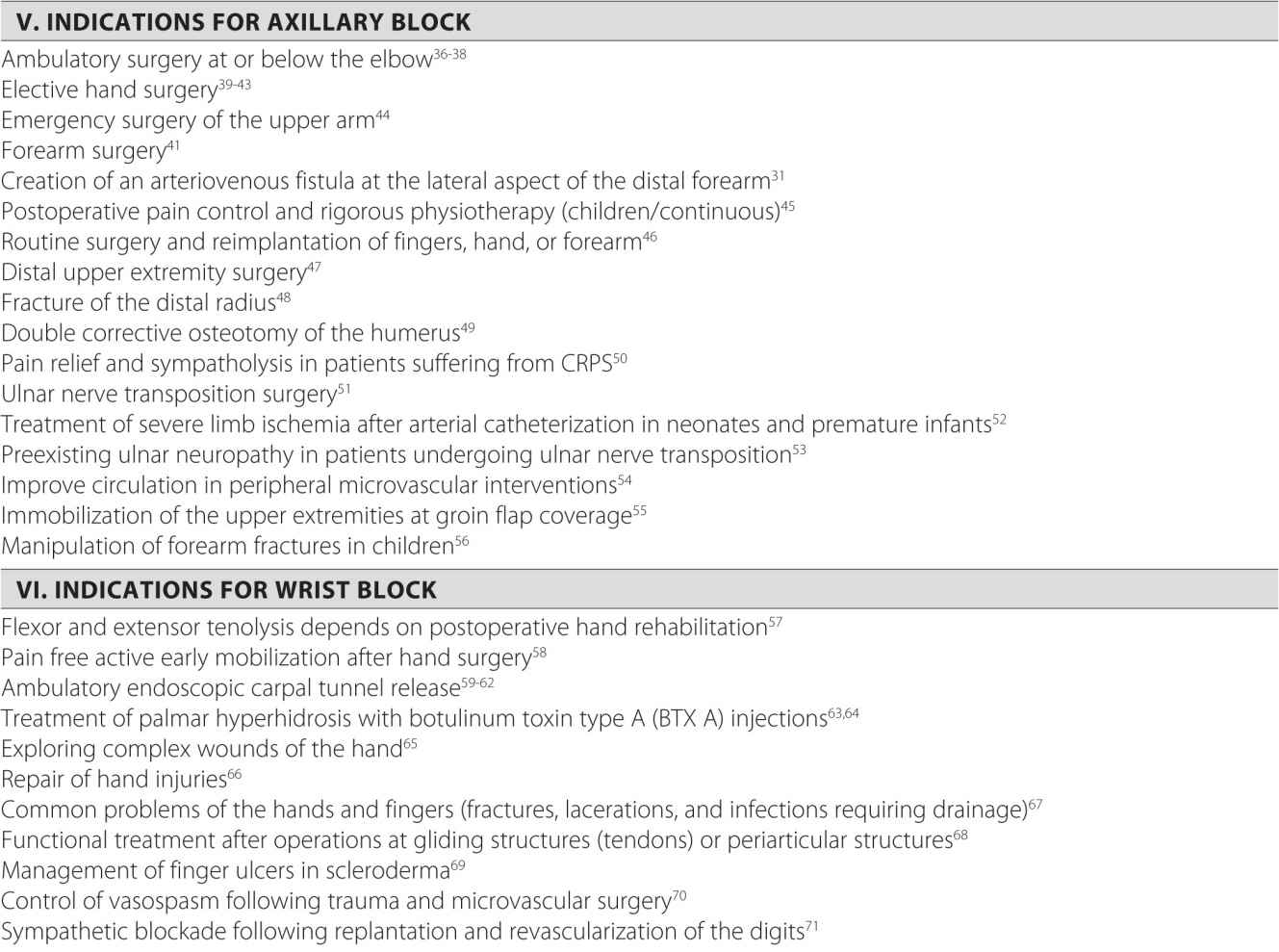
TABLE 6-1 Common Upper Limb Blocks
Lower Limb Blocks
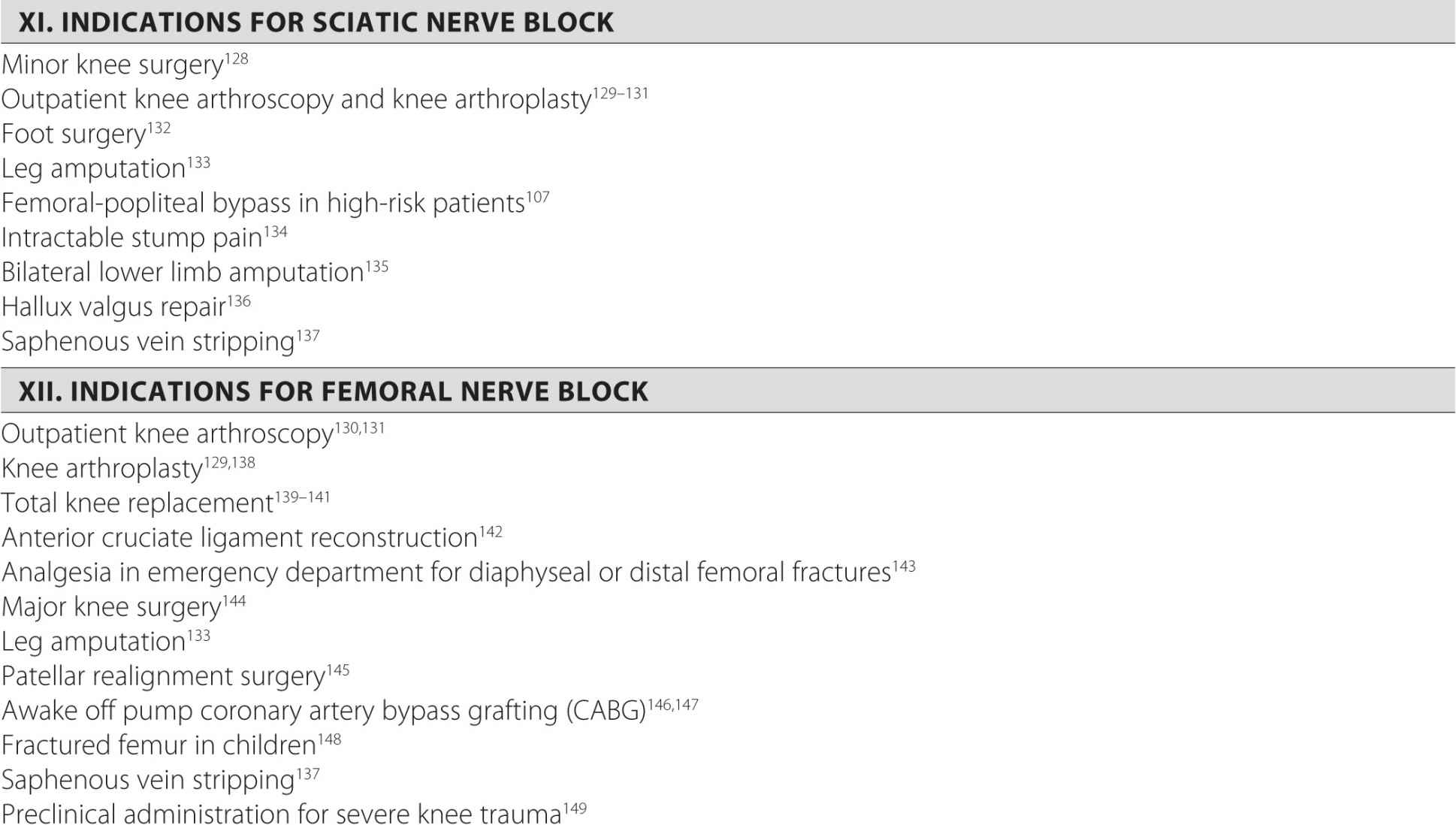
Achieving quality anesthesia or analgesia of the lower limb is more challenging than with an upper extremity. This is because its innervation stems from two major plexuses, the lumbar and the sacral. The lumbar plexus is formed by the roots of L1-L4 and gives rise to the femoral, obturator, and lateral femoral cutaneous nerves, among others. The sacral plexus originates from L4-S3, and its principal branch is the sciatic nerve. Most of the indications for lower limb blockade involve joint surgery on either the hip or the knee. Because both joints are supplied by elements of each plexus, complete anesthesia often requires at least two nerve blocks. Consequently, many clinicians choose to perform just one block for the purpose of analgesia. Table 6-2 lists some common lower limb blocks and their advantages and disadvantages.
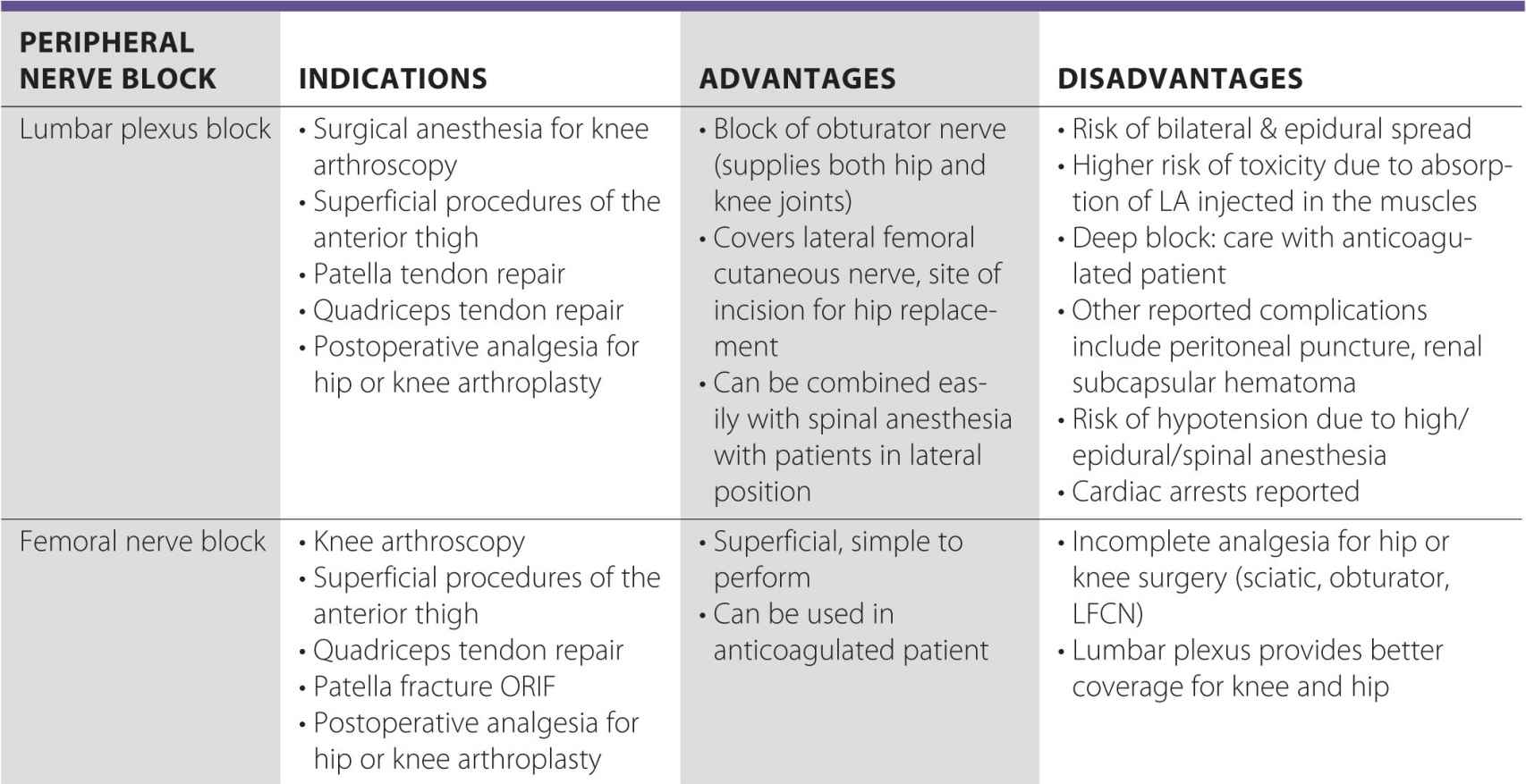
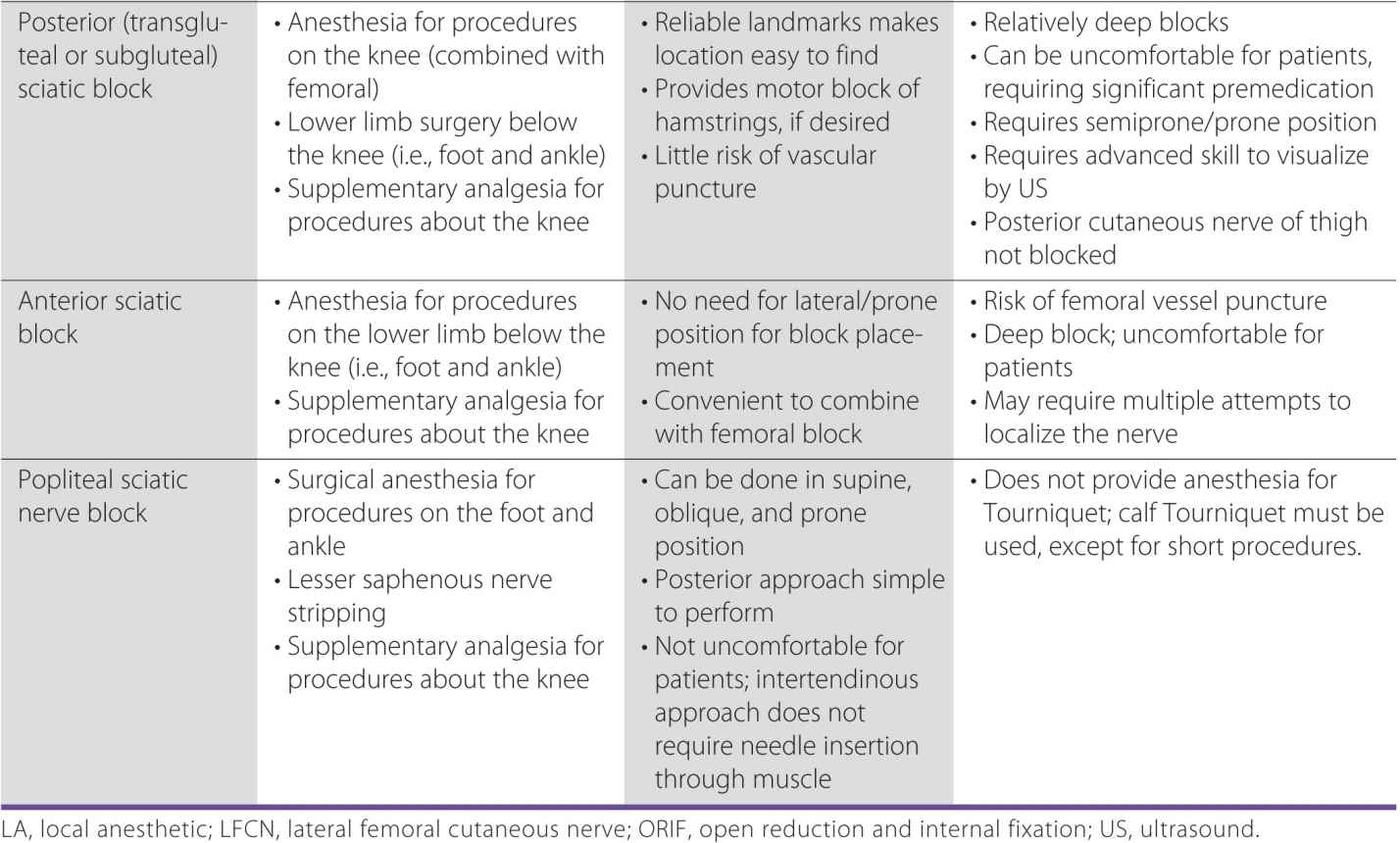
TABLE 6-2 Common Lower Limb Blocks
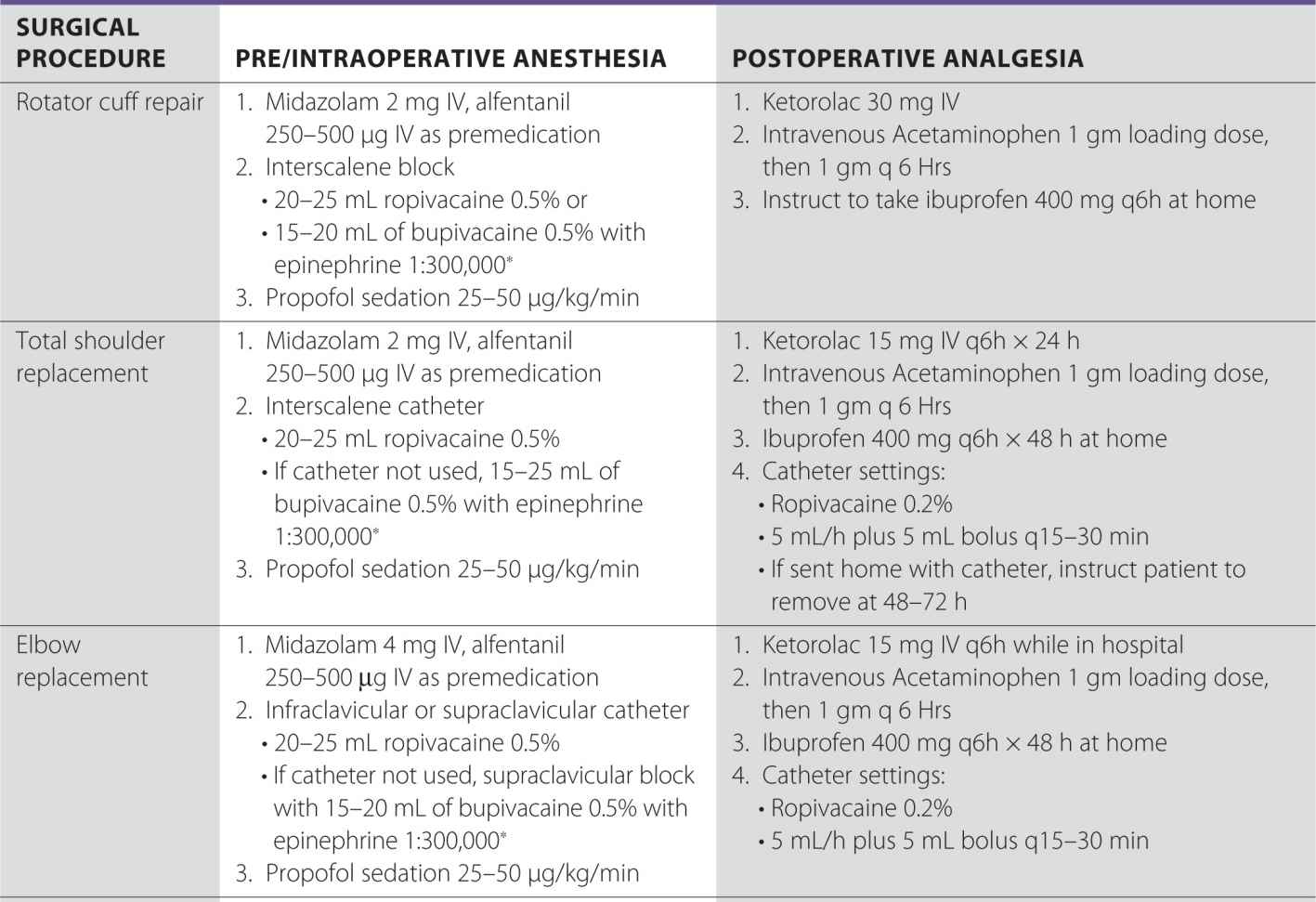
Section II: Protocols
A variety of different methods are available to provide intraoperative and postoperative analgesia for surgery on the extremity. Any anesthetic or analgesic plan is based on patient and surgical factors as well as practical considerations such as the practitioner’s skill level, availability of a block room, availability of skilled assistants, and departmental and hospital policies. The protocols for most common major orthopedic procedures outlined in this section were refined through trial and error and are the actual methods used in our daily practice.
The choice of the block combination for postoperative pain is based on several factors. The orthopedic surgeons at St. Luke’s-Roosevelt Hospital prefer a regimen of twice-daily dosing of low molecular weight heparin (LMWH) for thromboprophylaxis, which makes the use of an indwelling epidural catheter for postoperative pain impractical or unsuitable. Similarly, although we recognize there is some controversy regarding the use of lumbar plexus catheters in the same setting, by and large, we treat them as neuraxial catheters and remove them before the first dose of LMWH. Other perineural catheters are routinely placed and maintained even in patients who are treated with anticoagulants.
In recent years, we have made an effort to minimize the use of parenteral opioids for postoperative pain if possible. In particular, patients admitted to the ward with a perineural catheter and intravenous patient-controlled opioid analgesia can find it confusing to have two buttons to press, and therefore they do not use the catheter effectively, leading to inadequate analgesia. For this reason, we strive to make use of a multimodal regimen instead, consisting of acetaminophen, a nonsteroidal anti-inflammatory drug, and an oral opioid.
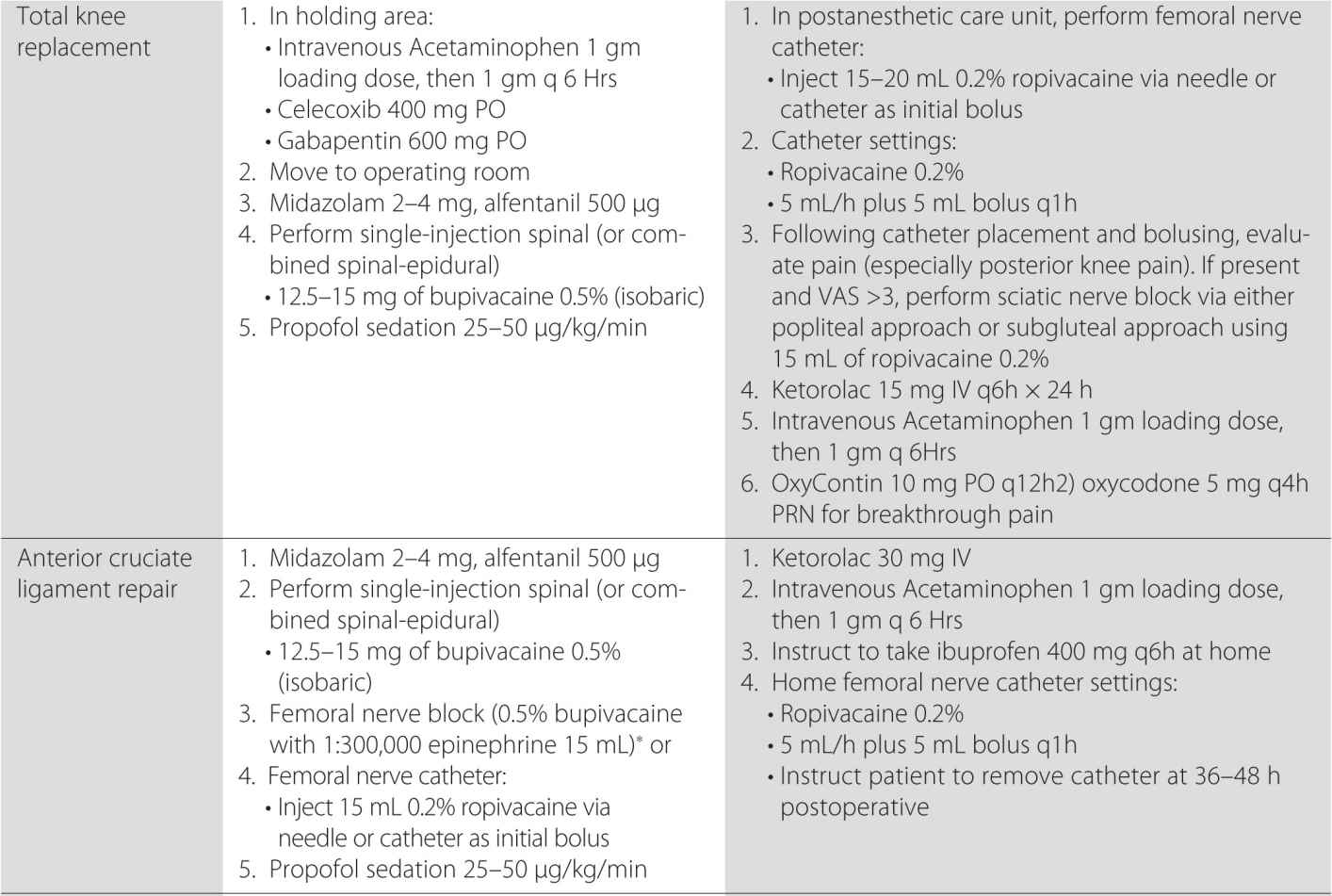
For lower limb surgery, such as total knee replacement, clinicians often debate whether the sciatic nerve and/or obturator blocks should be routinely used in addition to the femoral (or lumbar plexus) block. We do not routinely do this but rather assess the patient after the femoral/lumbar plexus blockade is performed. In our practice, in the majority of patients, postoperative pain is adequately managed (visual analog scale [VAS] ≤3) by continuous femoral nerve block alone. A small proportion of patients (about 20%) may require a sciatic nerve block for adequate pain control. Although often debated and taught in various regional courses, the usefulness of the obturator block in our practice is questionable at best. Consequently, we do not use obturator blocks in patients having knee arthroplasty.
The timing of block placement is institution dependent, and it relies on the presence of various factors, such as availability of the designated block personnel, operating room flow, ancillary staff, and a separate block area. Single-injection nerve blocks for surgery are performed either in the holding area or operating room immediately prior to the surgical procedure. Catheters for upper limb surgery are usually placed in a similar manner if the technique is used for surgical anesthesia as well. In contrast, most of our lower limb nerve blocks or catheters are placed in the postanesthesia care unit before the resolution of the neuraxial block. Although the practice of performing blocks in anesthetized patients (in this case in the presence of spinal anesthesia), we believe that when modern monitoring is used (combination of ultrasound, nerve stimulation, and injection pressure monitoring), it is irrelevant whether the blocks are performed in anesthetized or nonanesthetized patients.
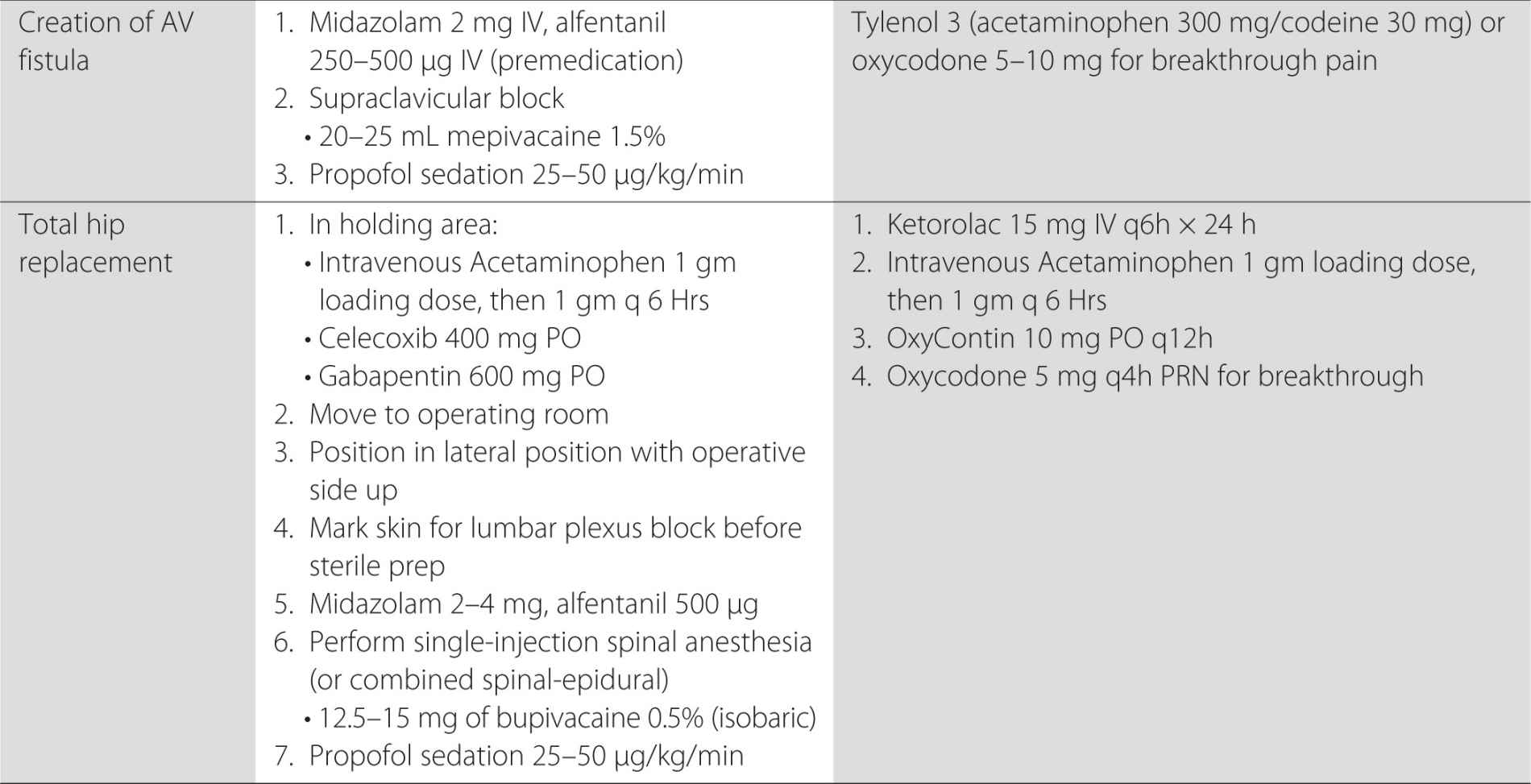
Finally, we do not routinely combine general anesthesia with regional anesthesia, although this is a widely used practice elsewhere. Our regional anesthetics are often used as the primary anesthesia modality, rather then solely for the purpose of postoperative analgesia. Instead of general anesthesia, we typically use sedation with propofol and/or intravenous midazolam titrated to light sleep and spontaneous breathing with supplemental oxygen via a facemask. Table 6-3 lists some common surgical procedures, peripheral nerve blocks that are suitable for anesthesia and analgesia, as well as other common analgesic options.
TABLE 6-3 Common Surgical Procedures and Analgesic Options
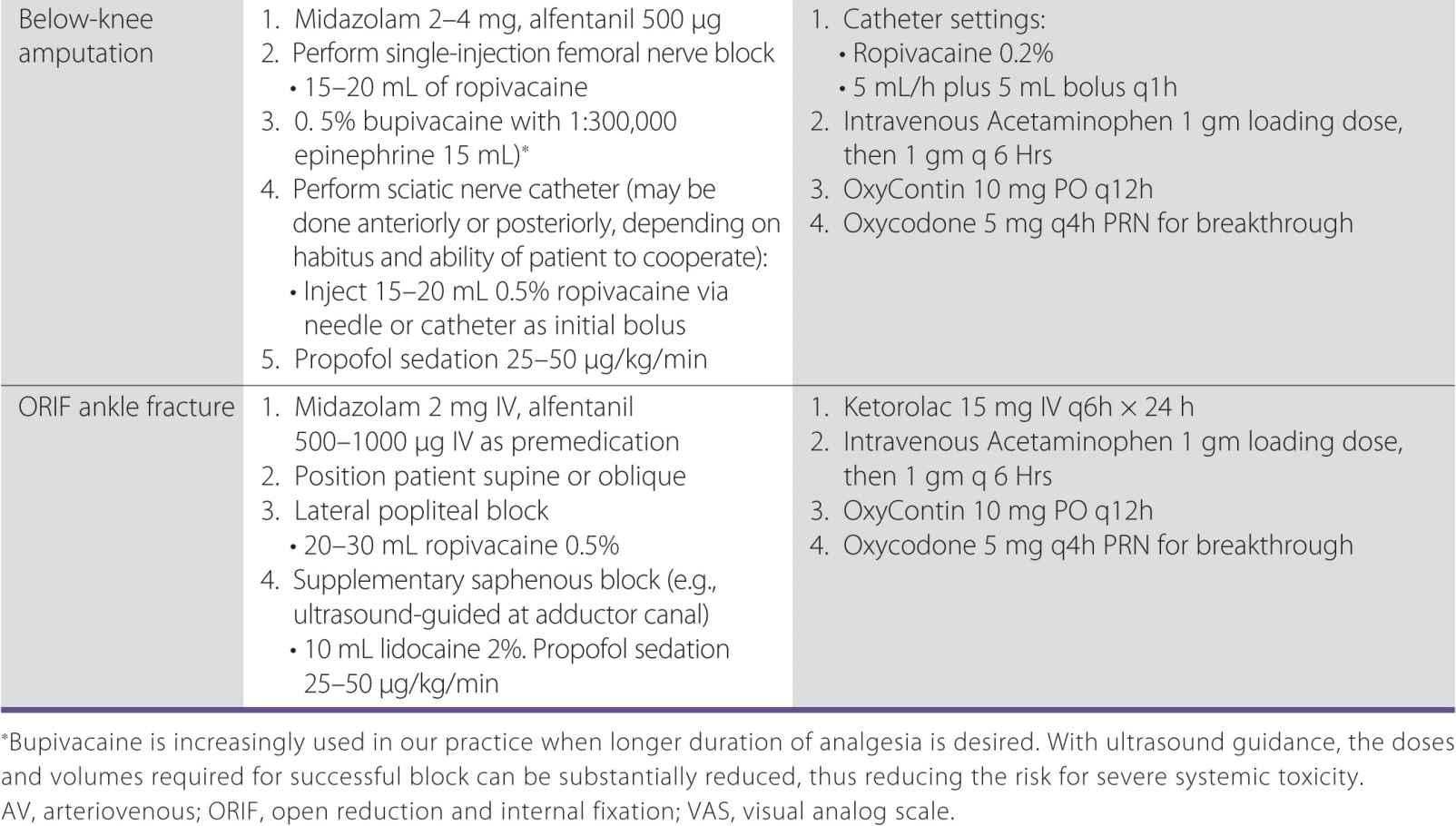
Section III: Compendium of the Literature
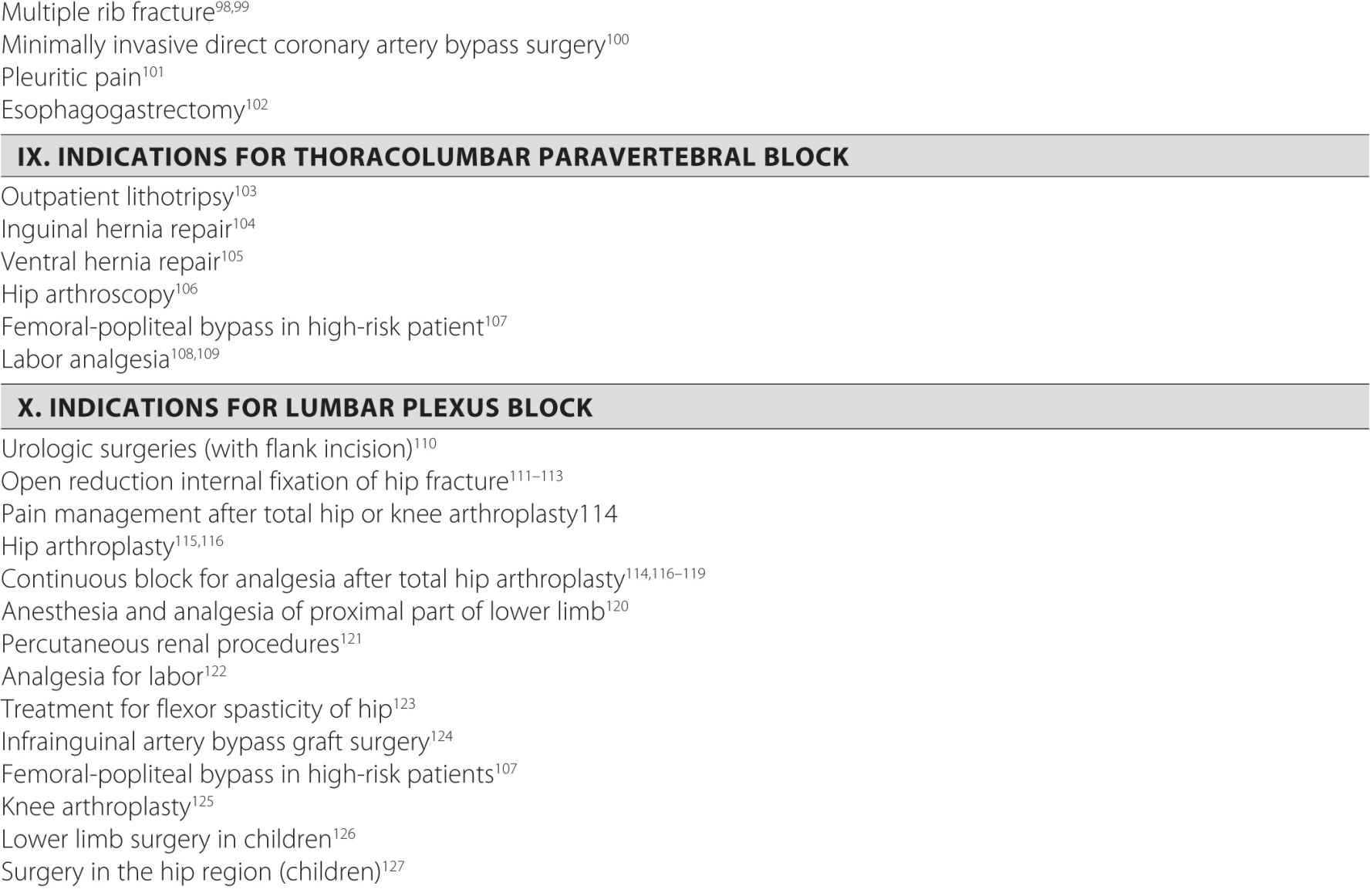
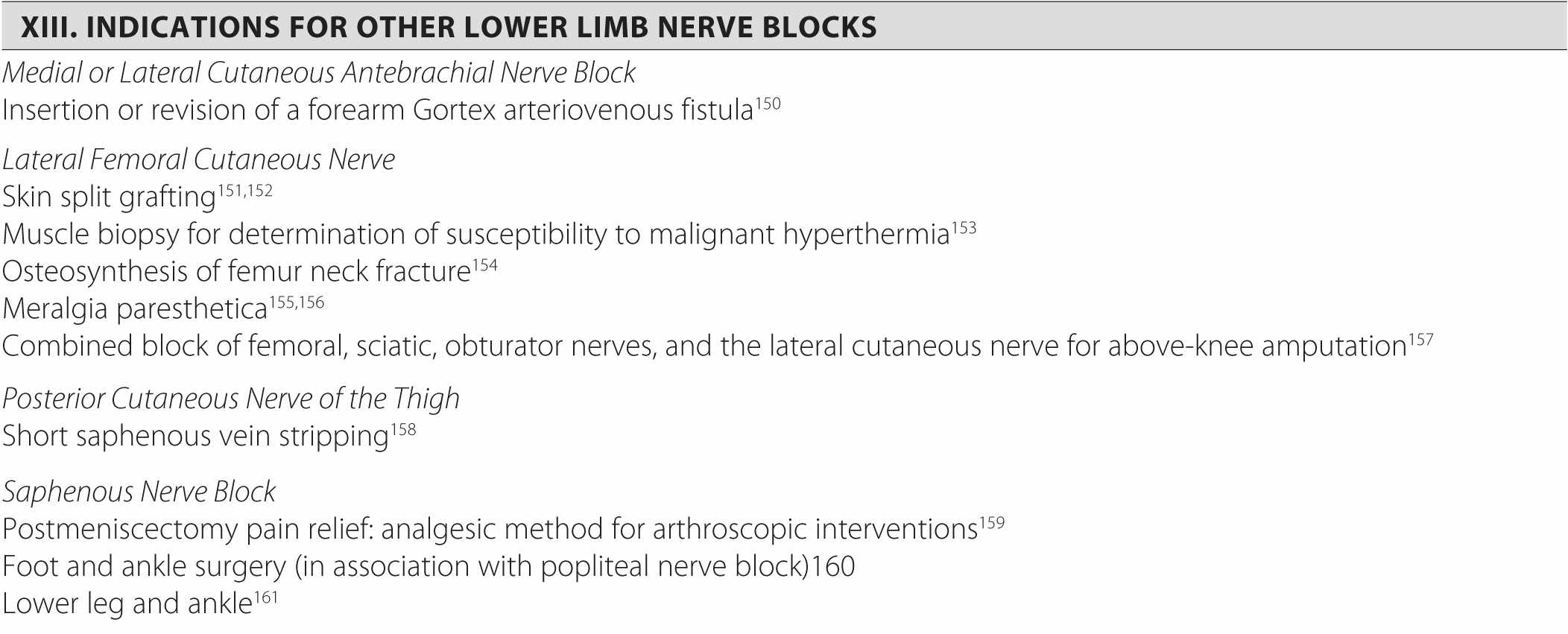
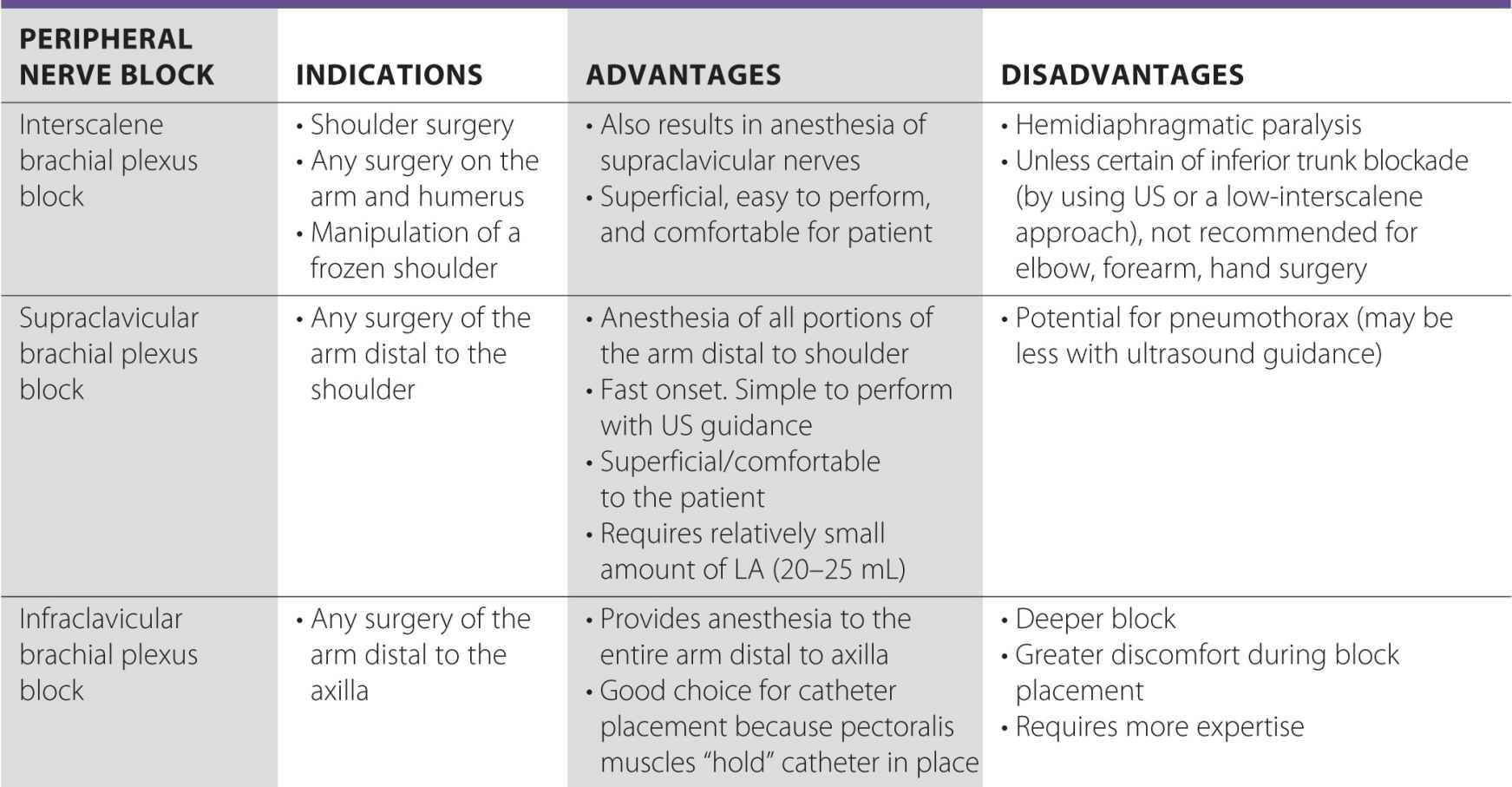
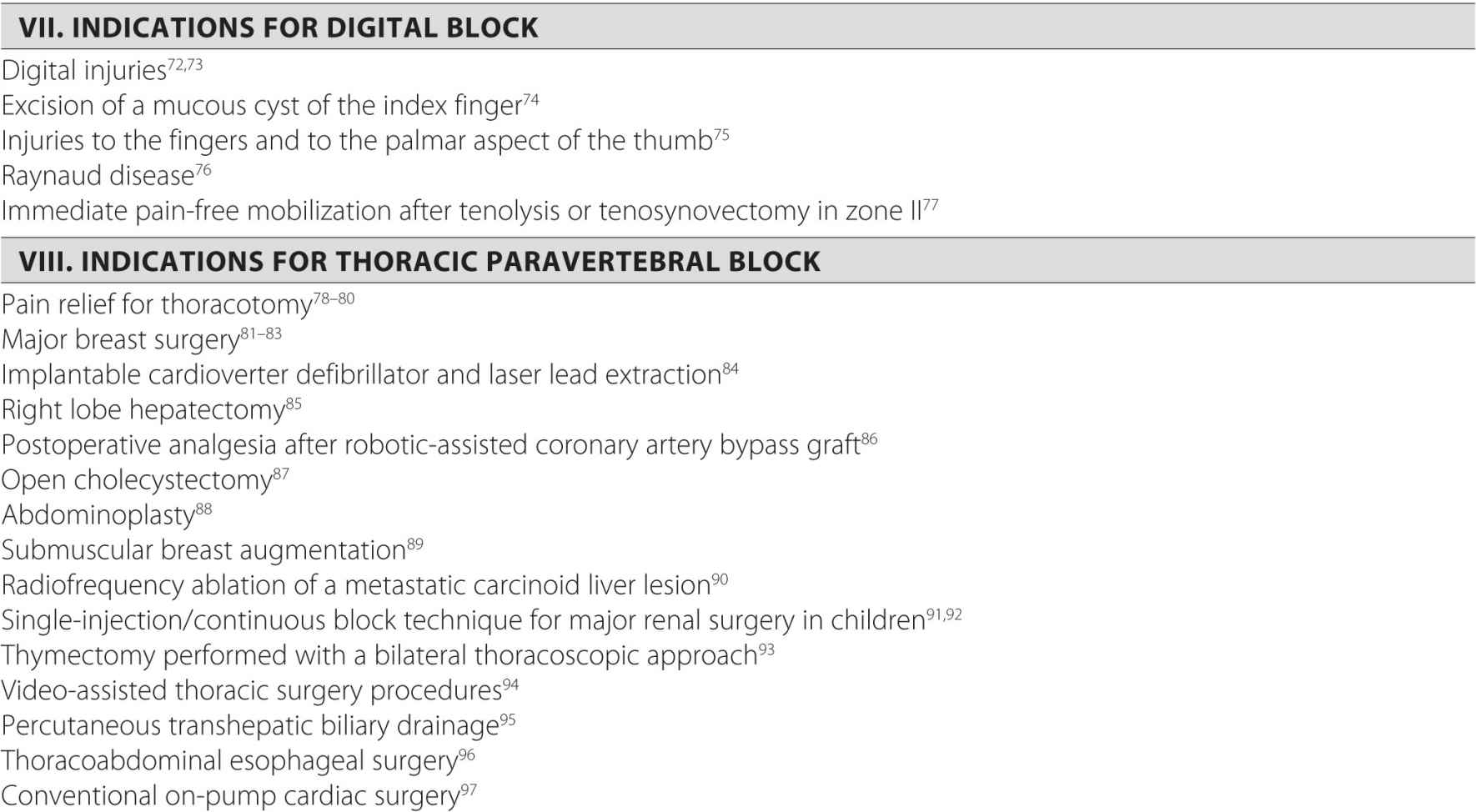
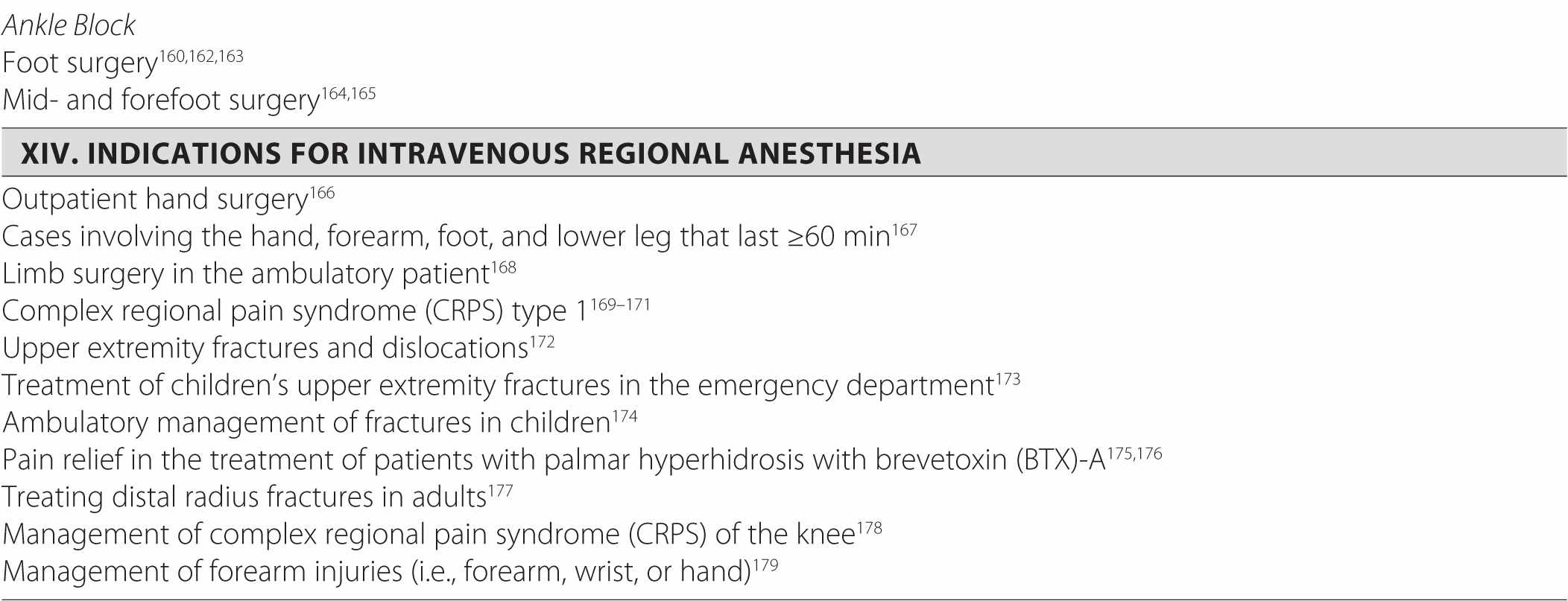
The previous two sections described some of the most common indications for peripheral nerve blocks in our practice. However, the usefulness of peripheral nerve blocks is much greater than the few common ones discussed here. For the sake of completeness, the compendium of indications for peripheral nerve blocks reported in medical literature is listed in the accompanying chart. Readers should use their own discretion when determining whether any indications would fit the realm of their own clinical practice.
REFERENCES
1. Suresh S, Templeton L. Superficial cervical plexus block for vocal cord surgery in an awake pediatric patient. Anesth Analg. 2004;98:1656-1657.
2. Goldberg ME, Schwartzman RJ, Domsky R, Sabia M, Torjman MC. Deep cervical plexus block for the treatment of cervicogenic headache. Pain Physician. 2008;11:849-854.
3. Stoneham MD, Knighton JD. Regional anaesthesia for carotid endarterectomy. Br J Anaesth. 1999;82:910-919.
4. Naja ZM, Al-Tannir MA, Zeidan A, et al. Bilateral guided cervical block for Zenker diverticulum excision in a patient with ankylosing spondylitis. J Anesth. 2009;23:143-146.
5. Ling KU, Hasan MS, Ha KO, Wang CY. Superficial cervical plexus block combined with auriculotemporal nerve block for drainage of dental abscess in adults with difficult airways. Anaesth Intensive Care. 2009;37:124-126.
6. Shteif M, Lesmes D, Hartman G, Ruffino S, Laster Z. The use of the superficial cervical plexus block in the drainage of submandibular and submental abscesses—an alternative for general anesthesia. J Oral Maxillofac Surg. 2008;66:2642-2645.
7. Pintaric TS, Hocevar M, Jereb S, Casati A, Jankovic VN. A prospective, randomized comparison between combined (deep and superficial) and superficial cervical plexus block with levobupivacaine for minimally invasive parathyroidectomy. Anesth Analg. 2007;105:1160-1163; table of contents.
8. Jones HG, Stoneham MD. Continuous cervical plexus block for carotid body tumour excision in a patient with Eisenmenger’s syndrome. Anaesthesia. 2006;61:1214-1218.
9. Choi DS, Atchabahian A, Brown AR. Cervical plexus block provides postoperative analgesia after clavicle surgery. Anesth Analg. 2005;100:1542-1543.
10. Aunac S, Carlier M, Singelyn F, De Kock M. The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg. 2002;95:746-750.
11. Nadig M, Ekatodramis G, Borgeat A. Continuous brachial plexus block at the cervical level using a posterior approach in the management of neuropathic cancer pain. Reg Anesth Pain Med. 2002;27:446; author reply 446-447.
12. Christiansen TG, Nielsen R. Reduction of shoulder dislocations under interscalene brachial blockade. Arch Orthop Trauma Surg. 1988;107:176-177.
13. Roubal PJ, Dobritt D, Placzek JD. Glenohumeral gliding manipulation following interscalene brachial plexus block in patients with adhesive capsulitis. J Orthop Sports Phys Ther. 1996;24:66-77.
14. Barak M, Iaroshevski D, Poppa E, Ben-Nun A, Katz Y. Low-volume interscalene brachial plexus block for post-thoracotomy shoulder pain. J Cardiothorac Vasc Anesth. 2007;21:554-557.
15. Casati A, Borghi B, Fanelli G, et al. Interscalene brachial plexus anesthesia and analgesia for open shoulder surgery: a randomized, double-blinded comparison between levobupivacaine and ropivacaine. Anesth Analg. 2003;96:253-259.
16. Faryniarz D, Morelli C, Coleman S, et al. Interscalene block anesthesia at an ambulatory surgery center performing predominantly regional anesthesia: a prospective study of one hundred thirty-three patients undergoing shoulder surgery. J Shoulder Elbow Surg. 2006;15:686-690.
17. Hingorani AP, Ascher E, Gupta P, et al. Regional anesthesia: preferred technique for venodilatation in the creation of upper extremity arteriovenous fistulae. Vascular. 2006;14:23-26.
18. Hadzic A, Williams BA, Karaca PE, et al. For outpatient rotator cuff surgery, nerve block anesthesia provides superior same-day recovery over general anesthesia. Anesthesiology. 2005;102:1001-1007.
19. Stone MB, Price DD, Wang R. Ultrasound-guided supraclavicular block for the treatment of upper extremity fractures, dislocations, and abscesses in the ED. Am J Emerg Med. 2007;25:472-475.
20. Harmon D, Frizelle HP. Supraclavicular block for day-case anaesthesia at altitude. Anaesthesia. 2001;56:197.
21. Ortells-Polo MA, Garcia-Guiral M, Garcia-Amigueti FJ, Carral-Olondris JN, Garcia-Godino T, Aguiar-Mojarro JA. Brachial plexus anesthesia: results of a modified perivascular supraclavicular technique [in Spanish]. Rev Esp Anestesiol Reanim. 1996;43:94-98.
22. Rigal MC, Esteve E, Alran R, Pech C. Brachial plexus block anesthesia in the upper limb surgery [author’s translation]. Anesth Analg (Paris). 1979;36:231-234.
23. Thompson AM, Newman RJ, Semple JC. Brachial plexus anaesthesia for upper limb surgery: a review of eight years’ experience. J Hand Surg Br. 1988;13:195-198.

Full access? Get Clinical Tree