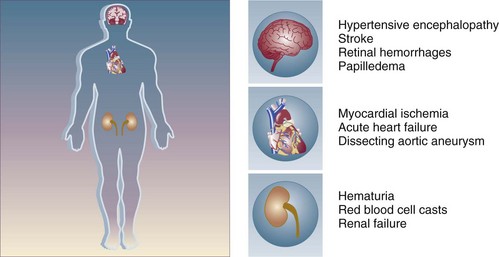
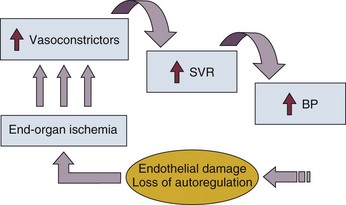
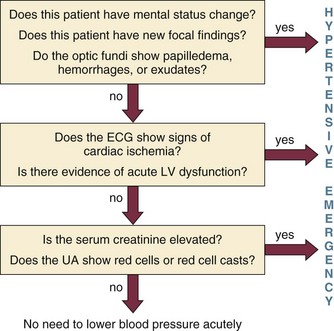
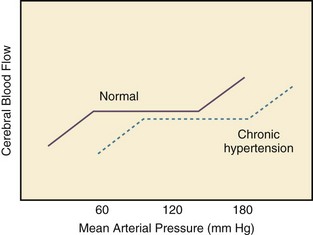
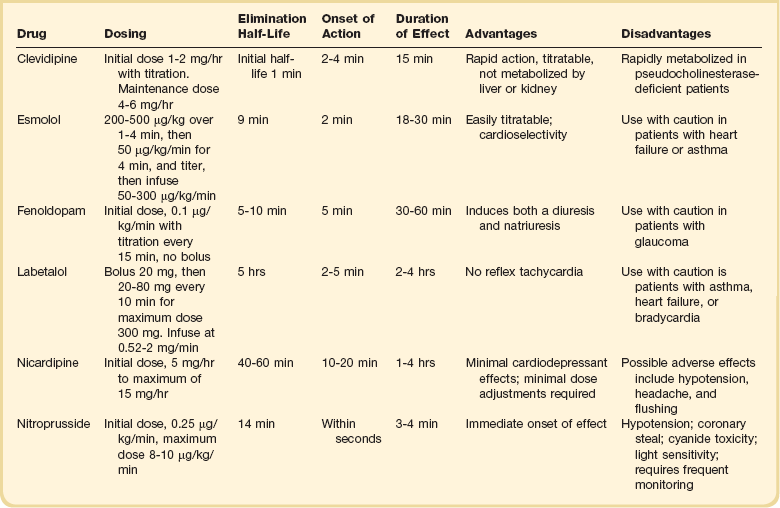
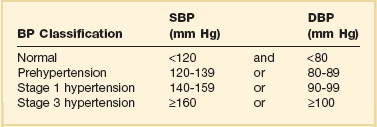
34 Hypertension is a common clinical disorder. Estimates indicate that almost 30% of the U.S. adult population suffers from elevated blood pressure.1 Furthermore, one third of these patients are unaware of their diagnosis, and of those who are diagnosed and treated, only 34% have adequate control of their blood pressure.2 Severe elevations in blood pressure, hypertensive crises, will occur in about 1% of patients with chronic hypertension.1,3 Hypertensive crises constitute a clinical problem that the intensivist will encounter in the hospital setting. Unfortunately, a paucity of clinical studies evaluating optimal therapeutic strategies and a lack of consideration for key pathophysiologic aspects have led to common misunderstandings and pitfalls in the management of patients with hypertensive crises. According to the seventh report of the Joint National Committee (JNC) on Detection, Evaluation, and Treatment of High Blood Pressure, hypertension is classified into three stages: prehypertension, stage 1, and stage 2 (Table 34.1).3 The terms malignant hypertension and accelerated hypertension have been abandoned. These terms were utilized to describe severe elevations in blood pressure associated with advanced retinopathy (Keith-Wagener-Barker stages 3 and 4). Prognosis of these clinical entities has improved dramatically with the advent of effective drugs for hypertension. In addition, studies have demonstrated that retinopathy as measured by the Keith-Wagener-Barker classification does not correlate with severity of hypertension or outcomes.4 Table 34.1 Classification of Hypertension (Joint National Committee [JNC] 7) BP, blood pressure; SBP, systolic blood pressure; DPB, diastolic blood pressure. A hypertensive emergency is a severe elevation in blood pressure associated with the presence of acute end-organ damage. Hypertensive emergencies require immediate control of blood pressure, within 1 to 2 hours, to prevent further organ damage. This will usually require the use of intravenous medications and invasive monitoring (arterial line) in a high-dependency unit such as the intensive care unit. The principal systems susceptible to acute end-organ damage from severe elevations in blood pressure include the central nervous, cardiovascular, and renal systems (Fig. 34.1). Several clinical situations are associated with hypertensive emergencies (Box 34.1). The absolute level of blood pressure and the time course of this elevation will determine the development of a hypertensive emergency. However, acute end-organ damage can occur at different blood pressure values in different patients. Therefore, it is more useful to define hypertensive emergencies with the presence of acute end-organ damage as opposed to specified numbers of systolic or diastolic blood pressure. In addition to initiating immediate therapeutic interventions, patients with a hypertensive emergency may require further diagnostic evaluation to determine the cause of their elevated blood pressure. Depending on the population studied, 20% to 50% of patients presenting with a hypertensive emergency will have a secondary cause of hypertension identified.5 The underlying pathophysiology of hypertensive crises is still not fully understood. The transition of mild hypertension or normotension to a hypertensive crisis is usually caused by an event that leads to an abrupt increase in blood pressure. Situations associated with this event may include cessation of hypertensive medications with potential rebound effects, consumption of illicit drugs, and severe pain, as well as several clinical syndromes. Blood pressure is determined by the product of cardiac output and systemic vascular resistance (BP = CO × SVR). In most hypertensive crises, the initial rise in blood pressure is secondary to increased systemic vascular resistance. The rise in systemic vascular resistance is believed to be caused by humoral vasoconstrictors.6 With the increase in blood pressure, mechanical stress on the arteriolar wall leads to endothelial damage and fibrinoid necrosis of the arterioles.6,7 Vascular damage leads to loss of autoregulatory mechanisms, ischemia, and acute end-organ damage, which prompts further release of vasoconstrictors and initiates a vicious cycle (Fig. 34.2).6,7 1. Should the blood pressure be lowered acutely? 2. How much should the blood pressure be lowered? 3. Which medication should be used to lower the blood pressure? To answer this question, the clinician must determine if there is evidence of acute end-organ damage. In patients with hypertensive emergencies (the presence of acute end-organ damage), the blood pressure should be lowered acutely to a safe target to prevent further end-organ damage. An organized approach in the evaluation of the patient is necessary. A focused history should determine a previous diagnosis of hypertension, medication history, use of illicit drugs or over-the-counter agents with potential hypertensive effects, and the presence of symptoms consistent with neurologic, visual, cardiac, or renal dysfunction. Physical examination should confirm vital signs. It is important to measure blood pressure adequately and in both upper extremities. Pulses should also be checked in all extremities, as inequalities in blood pressure or pulses can exist with aortic dissection. In addition, a thorough neurologic and cardiopulmonary examination should evaluate possible signs of end-organ failure such as altered mentation, new focal neurologic deficits, or cardiogenic pulmonary edema. A funduscopic examination of the eyes should be done to look for signs of acute papillary edema or new retinal hemorrhages. A set of simple diagnostic tests can complete the evaluation for acute end-organ damage. An electrocardiogram to rule out active ischemia and a chest x-ray to assess for pulmonary edema or signs of aortic pathology can help the clinician to evaluate the cardiopulmonary system. Abnormalities in blood urea nitrogen (BUN), creatinine, and the urinalysis (red blood cell [RBC] casts) suggest renal involvement. Additional tests may be indicated based on the individual characteristics of each case. An algorithm to establish the presence of acute end-organ damage at the bedside when evaluating patients is presented in Figure 34.3. Different organs have the ability to autoregulate and maintain a constant blood flow through a range of mean arterial pressures (MAPs). Under normal conditions cerebral autoregulation will keep blood flow constant between MAPs of 60 to 150 mm Hg.8 When the MAP drops, cerebral arteries will dilate, and if the MAP rises, they will constrict to maintain constant blood flow to the brain. Drops in the MAP below the lower limit of autoregulation will lead to hypoperfusion resulting in brain ischemia. Rises in the MAP above the higher limit of autoregulation will lead to acute end-organ damage from hypertension (hypertensive emergency). In the case of the brain, this may result in hypertensive encephalopathy. With chronic hypertension, compensatory functional and structural changes will occur in the vasculature.9,10 These changes will shift the autoregulatory curve to the right.11 The autoregulatory curve for cerebral blood flow in healthy individuals and in patients with chronic hypertension is shown in Figure 34.4. Hence, patients with chronic hypertension will have a higher tolerance to elevated blood pressures, as their autoregulatory curve is shifted to the right. This explains why many patients present with severely elevated blood pressure and no evidence of acute end-organ damage. However, rapid reductions of blood pressure to “normal” levels can fall below the lower autoregulatory capacity of the circulation in a chronically hypertensive patient. This phenomenon explains the hypoperfusion of vital organs and the development of renal failure or cerebral ischemia often seen when blood pressure is lowered too far or too fast.12 Based on these principles, most experts would recommend that for most hypertensive emergencies the goal should be to lower MAP by 15% to 25% over a period of several minutes to hours, depending on the clinical situation.13 Reduction of blood pressure to normal levels may be warranted in special situations such as those involving patients with aortic dissection or previously normotensive patients with a postoperative hypertensive emergency. The ideal medication to treat a hypertensive emergency should have a rapid onset of action, high potency, immediate reversibility, no tachyphylaxis, and minimal or no adverse effects. Although there is no perfect medication, several agents with some of these characteristics are summarized in Table 34.2. There are a limited number of studies comparing agents in terms of clinical outcomes. With no clear outcome data the selection of a particular agent is based on the clinical scenario, pharmacologic characteristics of the drug, and availability. We will further discuss parenteral agents that are useful in treating hypertensive emergencies (in alphabetical order). Clevidipine is relatively new agent approved for use in treating severe hypertension during surgery. It is an ultra-short-acting calcium-channel antagonist. Clevidipine has vasoselective properties with a rapid onset of action and a very short half-life (<1 minute).14 Clevidipine is metabolized by red blood cell esterases; therefore, its use is not affected in patients with renal and or hepatic failure. Clevidipine reduces blood pressure by a direct and selective effect on arterioles. It does not produce reflex tachycardia, and its effect on reducing afterload is often associated with increased cardiac output. Clevidipine is administered intravenously as a continuous drip. The initial dose is usually 1 to 2 mg/hour with adjustments as needed to obtain the desired response in blood pressure. The maintenance dose is usually 4 to 6 mg/hour; however, higher doses may be required in certain clinical situations. Small studies have compared clevidipine to nitroprusside for the treatment of severe hypertension in anesthetized patients undergoing surgery.15,16 These studies showed that clevidipine had similar effects on blood pressure control with less effect on cardiac filling and heart rate. Although clevidipine has not been studied extensively in other clinical situations, its characteristics make it an attractive option for the treatment of hypertensive emergencies outside of the operating room. More recently it seems to have received increased attention in neurologic hypertensive emergencies.17,18 Esmolol is an ultra-short-acting cardioselective, beta-adrenergic agent that can be administered intravenously for the treatment of hypertensive emergencies.19 Esmolol has a rapid onset of action (within 2 minutes), a short elimination half-life (approximately 9 minutes), and a rapid offset of action (within 15 to 30 minutes after stopping infusion).20 Esmolol is rapidly metabolized by red blood cells and is not dependent on renal or hepatic function.20 These properties enable easy titration of the drug and make it attractive in situations of a hypertensive emergency associated with intense adrenergic responses or tachycardia. This agent is available for intravenous (IV) use, both as a bolus and as a continuous infusion. The usual dose is 0.5 mg/kg as a loading dose, followed by a maintenance infusion of 25 to 300 µg/kg/min titrated to the patient’s individual response.20 Esmolol has been found to be effective in controlling postoperative hypertension and tachycardia in several clinical studies.21–23 Esmolol has also been utilized successfully to treat hypertensive emergencies under other various clinical situations.24,25
Hypertensive Crises
Introduction
Definitions
Pathophysiology
Approach to Management
Should the Blood Pressure Be Lowered Acutely?
How Much Should the Blood Pressure Be Lowered?
Which Medication Should Be Used to Lower the Blood Pressure?
Clevidipine
Esmolol

Full access? Get Clinical Tree


Hypertensive Crises