163 Hyperglycemic Comas
Diabetic ketoacidosis (DKA) and hyperosmolar nonketotic hyperglycemia syndrome (HNHS) are life-threatening syndromes caused by metabolic derangement associated with diabetes mellitus, both insulin dependent (type 1) and non–insulin dependent (type 2). Although a distinction is made in the definitions of the two syndromes, there is much commonality between them, with up to 30% of presentations having features of both syndromes. DKA is approximately three times as common as HNHS in patients presenting with hyperglycemic syndromes.1 Although the metabolic derangement seen in DKA and HNHS is extreme, the death rate associated with these syndromes is low with appropriate and meticulous therapy. Surveys of patients presenting with hyperglycemic syndromes have found an overall mortality rate of less than 5% associated with DKA and 15% associated with HNHS.1,2 Most deaths are not caused by the metabolic derangement but occur as a result of coexisting disease (e.g., myocardial infarction), sepsis (particularly pneumonia), or less frequently, the management methods employed.2
 Hyperglycemic Syndromes
Hyperglycemic Syndromes
Diabetic Ketoacidosis
DKA has an incidence of approximately 8.6% in diabetics2 and occurs in a younger age group (mean age, 33 years) compared with DKA-HNHS (44 years) or HNHS (69 years).1 Precipitating factors associated with the development of DKA include3–5:
Laboratory tests supporting the diagnosis of DKA commonly reveal the following:
Hyperosmolar Nonketotic Hyperglycemia Syndrome
Laboratory test results are similar to those listed for DKA but differ somewhat in degree, in that:
Metabolic Derangements in Hyperglycemic Syndromes
The main metabolic derangements that result in morbidity and must be urgently addressed in the management of both DKA and HNHS are severe dehydration, insulin deficit, electrolyte depletion, and metabolic acidosis. These are discussed in detail in Chapters 12 and 18.
Severe dehydration is estimated to be a water deficit in the range of 100 to 200 mL/kg.4 Although there is no consensus on the ideal approach to fluid management in these patients, prompt restoration of the circulation with isotonic fluid (e.g., normal saline or preferably compound sodium lactate solution), followed by more moderate replacement of the water deficit using hypotonic fluid, are the underlying principles.
Figure 163-1 shows serial measurements taken from a typical patient with DKA on presentation and during his treatment in the ICU.
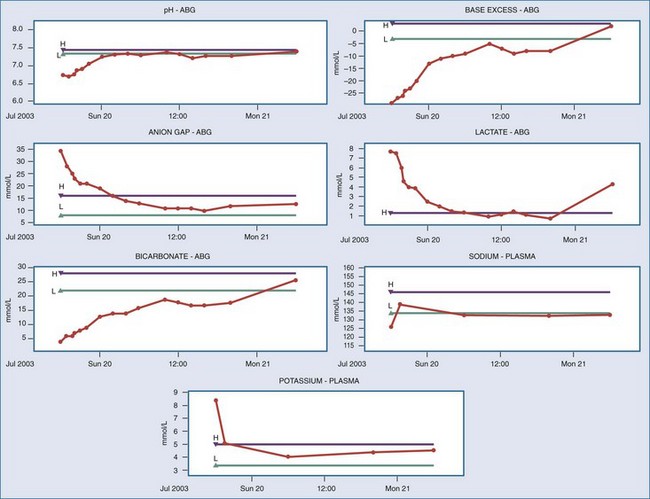
Figure 163-1 Trends in metabolic parameters monitored during treatment of diabetic ketoacidosis. ABG, arterial blood gases.

Full access? Get Clinical Tree




