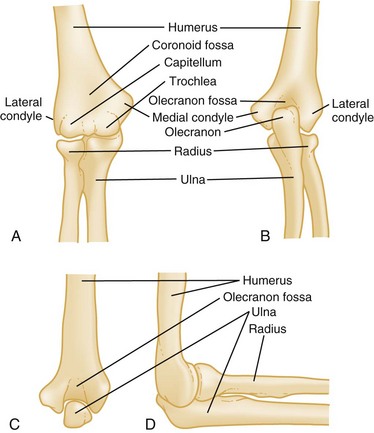
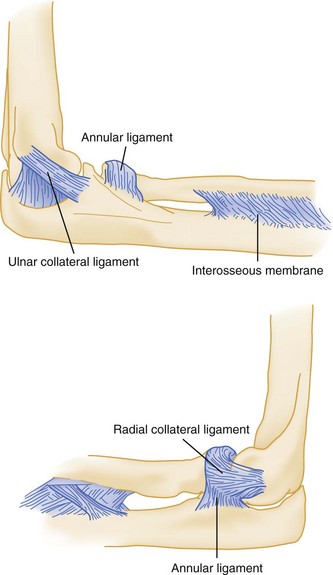
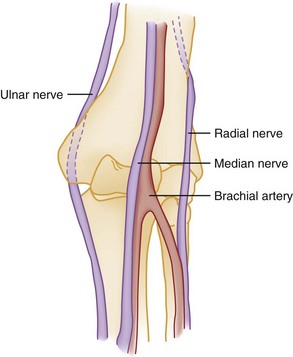
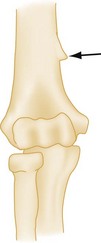
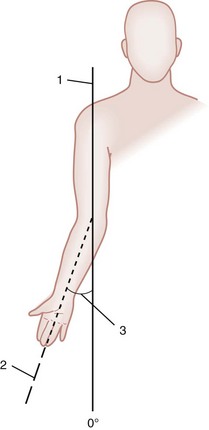
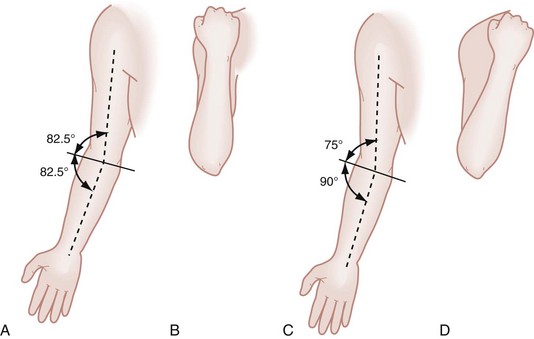
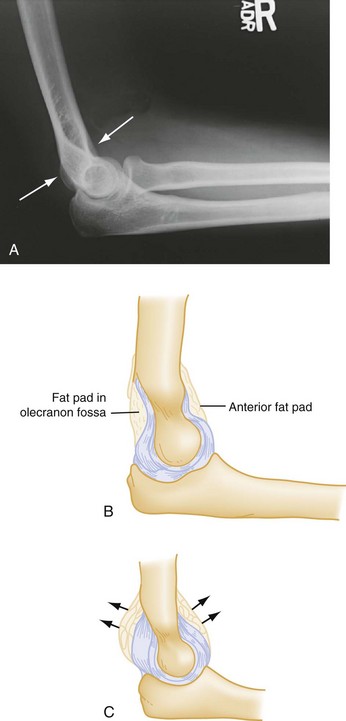
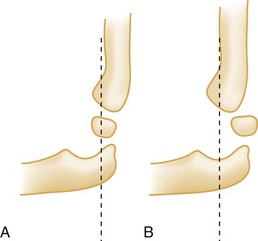
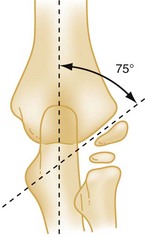
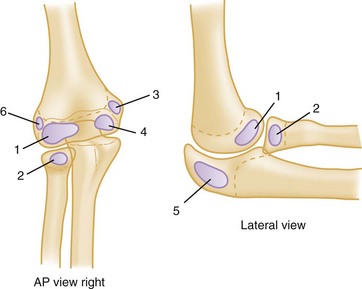
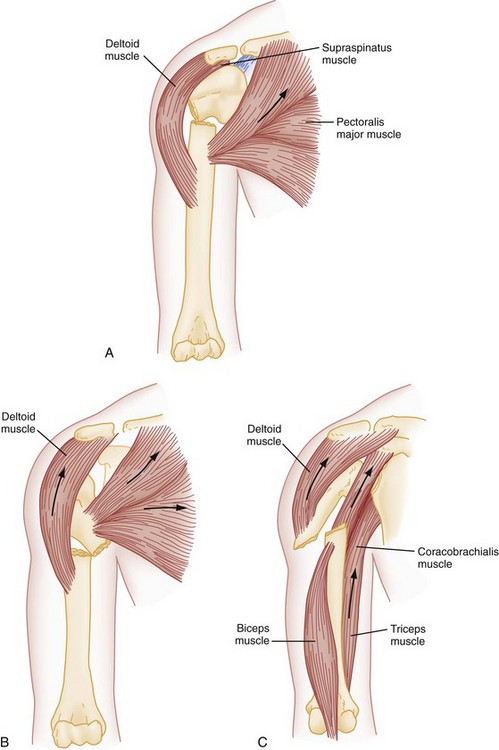
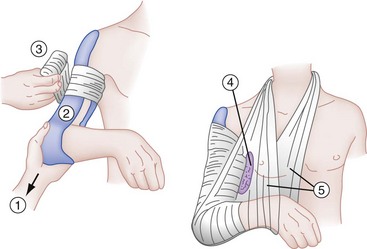
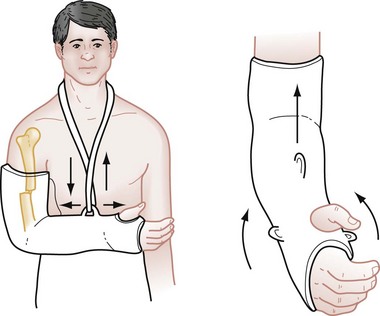
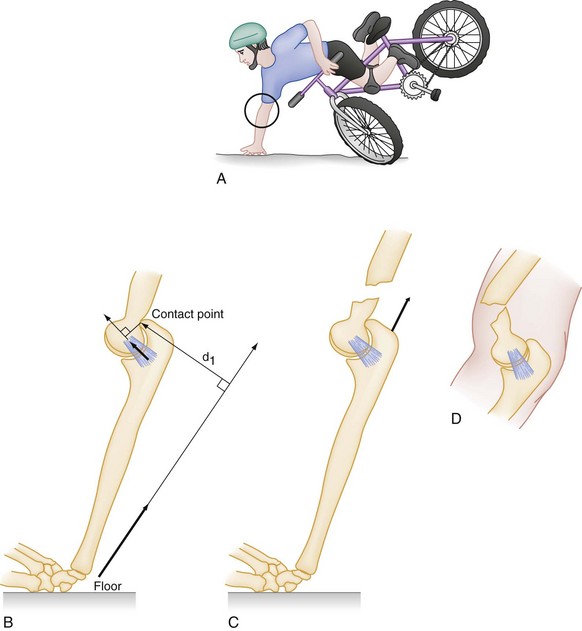
Chapter 52 The bony anatomy of the distal humerus and elbow is diagrammed in Figure 52-1. The distal end of the humerus tapers into two columns of bone, the medial and lateral condyles. Between the condyles, the bone thins, and the recess created is the coronoid fossa. The more proximal nonarticular portions of the condyles are the epicondyles. Just proximal to the epicondyles, the supracondylar ridges run up each side of the humerus. Collectively, these areas serve as points of origin for the muscles of the forearm. The wrist flexors originate from the medial epicondyle, and the wrist extensors originate from the lateral epicondyle. Fractures of the distal humerus often result in fragment displacement because of the pull of these strong forearm muscles on attachment sites. Four ligamentous structures are important in evaluating elbow injuries (Fig. 52-2). The radial head is held in place by the annular ligament and the adjacent radial collateral ligament. Rotation of the radial head within the confines of the fibrous annular ligament permits pronation and supination. In addition, the ulnar collateral ligament and anterior capsule add stability to the joint. Fracture or dislocation of the joint may severely damage the ligamentous structures. The neurovascular structures of this area are shown in Figure 52-3. The brachial artery, which is the continuation of the axillary artery, travels with the median nerve in the anterior compartment of the upper arm. It enters the antecubital fossa and bifurcates into the radial and ulnar arteries. One important anatomic variation is the presence of a supracondylar process (in approximately 2.5% of cases) just proximal to the medial epicondyle (Fig. 52-4). When the supracondylar process is present, the median nerve and brachial artery must traverse behind this process, then forward between a fibrous band connecting the process to the epicondyle. Median nerve symptoms may develop if this process is fractured or if an injury causes swelling in the vicinity of the supracondylar process. One special aspect of the elbow examination is the determination of the carrying angle, the normal outward angulation of the extended forearm at the elbow. This angle allows the long axes of the humerus and forearm to become superimposed when the elbow is flexed (Fig. 52-5). This angle varies from 5 to 20 degrees in adults, with men having less angulation than women. Measurement of the carrying angle is helpful in assessing subtle supracondylar fractures in children. As shown in Figure 52-6, lines drawn parallel to the shafts of the humerus and ulna intersect to form an angle with a mean measurement in children of 13 degrees, although this angle varies widely.1 A difference in carrying angles of greater than 12 degrees (from one side to the other for a particular individual) is associated with fractures. However, the carrying angle is used primarily for assessing the adequacy of reduction or the results of fracture healing rather than for acute diagnosis, because it is difficult for children to fully extend the arm during the initial evaluation for this measurement to be obtained. Many fractures in the elbow region are obvious on plain film, with cortical disruption, angulation, or displacement of fragments. Minor fractures can be subtle and may be missed. Special attention to the contour of the radial head and the fat pads reduces the risk of missing fractures. The normal cortex of the radius is smooth and has a gentle continuous concave sweep. If consistent with history and physical findings, any disruption of this smooth arc is considered evidence of fracture. Abnormalities within the soft tissues on elbow films are particularly important and may be the only radiographic sign of a fracture. Normally, fat surrounding the proximal elbow joint is hidden in the concavity of the olecranon and coronoid fossae. The normal elbow has only a narrow strip of lucency anteriorly (the anterior fat pad), and a posterior fat pad is not visible on radiographs. Injuries that produce intra-articular hemorrhage cause distention of the synovium and displace the fat out of the fossa, making the posterior fat pad visible on lateral radiographic views. The anterior fat pad also is altered by this swelling, becoming more prominent and taking the shape of a spinnaker sail from a boat: “sail sign” (Fig. 52-7). In the setting of trauma, more than 95% of patients with the “posterior fat pad” sign have intra-articular skeletal injury. These soft tissue findings occur even with subtle fractures, and when they are present in the setting of trauma, an occult fracture is considered to be present even when not visible on radiographs. In adults, a radial head fracture is implied, whereas in children a supracondylar fracture is the more likely underlying injury. In the absence of trauma, the presence of a fat pad suggests other causes of effusion (e.g., gout, infection, bursitis). The fat pad signs may be absent in fractures where the injury is severe enough to rupture the capsule. The anterior humeral line is a line drawn on a lateral radiograph along the anterior surface of the humerus through the elbow. Normally, this line transects the middle third of the capitellum (Fig. 52-8). With an extension supracondylar fracture, this line either transects the anterior third of the capitellum or passes entirely anterior to it. The abnormal relationship between the anterior-humeral line and capitellum may be the only evidence of a minimally displaced supracondylar fracture and is a presumptive finding of a fracture. Another diagnostic aid in evaluating radiographs of possible supracondylar fractures in children is the determination of Baumann’s angle. As shown in Figure 52-9, the intersection of a line drawn on the anteroposterior film through the midshaft of the humerus and the growth plate of the capitellum defines an angle of approximately 75 degrees. In normal children, Baumann’s angle is the same in both elbows, and it has been suggested that a comparison between the injured and uninjured sides be used to assess the accuracy of reduction. An increase in Baumann’s angle indicates medial tilting of the distal fragment. Alteration in Baumann’s angle is thought to predict the final carrying angle when the fracture heals, although there is controversy regarding its reliability.2 Radiographic evaluation of the elbow in children is difficult because of the presence of multiple ossification centers (Fig. 52-10). Table 52-1 lists the typical age of first appearance and fusion of ossification centers, which gives rise to the CRITOE acronym: Table 52-1 Ossification Centers of the Elbow: CRITOE Injuries in the region of the shaft of the humerus and about the elbow fall into several categories (Box 52-1). Emergency department (ED) management varies with location and type of fracture or dislocation. Supracondylar fractures of the humerus in children are usually described according to the Gartland classification (Box 52-2). Fractures of the humeral shaft commonly result from a direct blow to the arm, such as occurs during a fall or motor vehicle collision. Severe twisting of the arm or a fall on an outstretched hand can also produce this type of fracture. Fractures produced by violent muscle contraction, such as occurs when a javelin or baseball is thrown, also are reported.3 Motion of the humerus is controlled by several muscle groups, which also influence the fracture pattern of the humeral shaft. If the fracture is located proximal to the attachment of the pectoralis major, the proximal fragment of the humerus abducts and rotates internally owing to the action of the rotator cuff, whereas the distal fragment is displaced medially by the pectoralis major (Fig. 52-11A). If the fracture occurs below the pectoralis major insertion but above the deltoid insertion, the distal fragment is displaced laterally by the deltoid muscle, and the proximal fragment is displaced medially by the pull of the pectoralis major, latissimus dorsi, and teres major muscles (Fig. 52-11B). In fractures occurring distal to the deltoid insertion, the proximal fragment is abducted by the deltoid, and the distal fragment is proximally displaced (Fig. 52-11C). The shaft of the humerus most commonly fractures in the middle third in a transverse fashion (Fig. 52-12). Radiographic findings are confirmatory. Studies routinely should include the shoulder and elbow joints. The humerus is a common site for benign tumors, unicameral cysts, and primary bone malignancies. The humeral shaft also is a common site for metastatic disease. Thinning of the cortex and abnormal osteoblastic or osteoclastic activity are evidence of a pathologic fracture (see Fig. 52-12). These fractures do not heal without concomitant treatment of the underlying pathologic condition. Closed fractures that are isolated injuries are treated conservatively with a high degree of success. Elaborate attempts at fracture reduction and external immobilization are unnecessary and sometimes detrimental to healing. Humeral shaft fractures remain surrounded by a richly vascularized envelope of muscle so that fracture reduction is accomplished most easily with the aid of gravity and muscle balance. Fractures that are nondisplaced or minimally displaced are immobilized by adding a coaptation, or “sugar-tong,” splint, to the sling and swathe (Fig. 52-13). This is accomplished by first padding the extremity, then carrying a long plaster splint from the lateral side of the shoulder, down the lateral aspect of the upper arm, around the elbow with the elbow flexed, and then up the inner aspect of the arm to the axilla. The sugar tong is wrapped in an elastic bandage, and a sling is used to support the arm in 90 degrees or less of flexion. The weight of the splint aided by gravity applies traction while it immobilizes the fracture. Some authorities use the coaptation splint for only the first 10 to 14 days of treatment, followed by a functional brace. If the fracture is grossly displaced or comminuted, the hanging cast technique sometimes is used. This technique is especially effective with spiral fractures. The cast is lightweight, applied at least 1 inch proximal to the fracture site, and extends to the distal palmar crease of the hand. The elbow is flexed 90 degrees, and the wrist is placed in the neutral position. The sling is attached through a loop at the wrist. Angulation is corrected by placing the plaster loop on the dorsal aspect of the cast (to reduce lateral angulation) or on the volar side of the cast (to reduce medial angulation). Anterior or posterior angulation is corrected by altering the length of the sling apparatus (Fig. 52-14). Care is taken not to make the cast too heavy because this would distract fracture fragments. The hanging cast has the disadvantage of requiring gravity for traction and requires that the patient remain upright at all times, including during sleep, a situation that many patients find intolerable. Neurovascular examination should be repeated and documented after the application of any splint or cast, because loss of nerve function from entrapment of the nerve between fragments can occur after these interventions. The use of open reduction and internal fixation (Fig. 52-15) has been more frequent recently and is necessary in certain circumstances, including open fractures, presence of multiple injuries that preclude mobilization, bilateral fractures, poor reduction, poor patient compliance, failure of closed treatment, and fractures through pathologic bone.4,5 Isolated radial nerve palsy usually is assumed to be a neurapraxia and is managed nonoperatively. Exploration and internal fixation are indicated, however, if the radial nerve palsy develops after manipulation because this is highly suggestive of nerve entrapment.4 Figure 52-15 Midshaft humerus fracture: A, before and B, after open reduction and internal fixation. Distal humerus fractures that occur proximal to the epicondyles are called supracondylar fractures. This type of fracture is almost exclusively an injury of the immature skeleton, with a peak incidence in children 5 to 10 years old6 This injury rarely occurs after age 15 and accounts for approximately one half of all elbow fractures and one third of pediatric limb fractures. In children, the tensile strength of the collateral ligaments and joint capsule of the elbow is greater than that of bone. In adults, the reverse is true, and a posterior elbow dislocation is sustained instead. Supracondylar fractures are classified as either extension or flexion fractures, depending on the mechanism of injury and the displacement of the distal fragment. Of these injuries, 98% are of the extension type. Extension Supracondylar Fractures: Pathophysiology.: Extension supracondylar fractures occur as a consequence of a fall on the outstretched arm when the elbow is either fully extended or hyperextended (e.g., a fall off the “monkey bars”). The elbow is likely to be in the latter position at the time of the fall because ligamentous laxity, with hyperextension of the joints, is a normal phenomenon in younger children. With the forearm acting as a lever,7 the ground reaction produces a moment of force at the elbow (Fig. 52-16). Ultimately the distal humerus fails anteriorly in the supracondylar area. The strong action of the triceps tends to pull and displace the distal fragment in a posterior and proximal direction. There may be anterior angulation of the sharp distal end of the proximal fragment into the antecubital fossa, endangering the brachial artery and median nerve (Fig. 52-17). In most cases, however, the brachialis muscle protects the anterior neurovascular structures from injury.
Humerus and Elbow
Perspective
Anatomy
Clinical Features
Physical Examination
Radiographic Findings
OSSIFICATION CENTERS
AGE OF APPEARANCE
Capitellum
1-2
Radial head
4-5
Internal (medial) epicondyle
4-5
Trochlea
8-10
Olecranon
8-9
External (lateral) epicondyle
10-11
Fractures
Fractures of the Shaft of the Humerus
Clinical Features
Management

Fractures of the Distal Humerus

Full access? Get Clinical Tree


Humerus and Elbow
Only gold members can continue reading. Log In or Register to continue