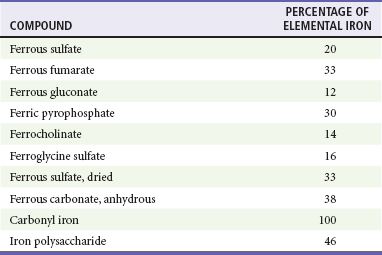
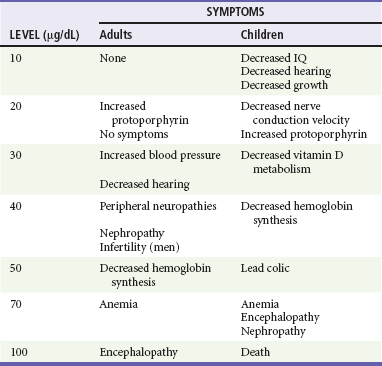
Chapter 157 Iron, which is essential to the function of hemoglobin, myoglobin, many cytochromes, and many catalytic enzymes, can be extremely toxic when levels are elevated after an overdose or from accumulation in disease states.1 The acute ingestion of iron is especially hazardous to children. Ingestions of pediatric multivitamin formulations are the most common iron exposures. These occur in children younger than 6 years and are minimally toxic. Life-threatening toxicity is associated with ingestion of potent adult preparations, such as prenatal vitamins. Serious iron ingestions in adults are usually associated with suicide attempts.2 In assessment of the severity of an iron exposure, it is important to refer to the amount of elemental iron ingested because the toxicity of an iron compound depends on the amount of elemental iron it contains (Table 157-1). Different formulations of iron salts contain different percentages of elemental iron. The total amount of elemental iron ingested can be approximated by multiplying the estimated number of tablets by the fraction of elemental iron contained in the tablet. Manufacturers are also required to list the amount of elemental iron per tablet. Ingestions of less than 20 mg/kg of elemental iron usually cause no symptoms. Ingestion of 20 to 60 mg/kg results in mild to moderate symptoms, and ingestion of more than 60 mg/kg may lead to severe morbidity and mortality. Although the dose of elemental iron associated with 50% mortality (LD50) is 200 to 250 mg/kg, doses as small as 130 mg of elemental iron have been lethal in children.3 Newer forms of iron are carbonyl iron and iron polysaccharide; both are non-ionic and associated with lower toxicity. Neither form is directly corrosive, and the conversion to the iron ion, which is responsible for toxicity, is very slow. There are no reported cases of serious toxicity or death from the ingestion of these compounds.4,5 Iron has two distinct toxic effects: (1) it causes direct caustic injury to the gastrointestinal mucosa, and (2) it impairs cellular metabolism, primarily of the heart, liver, and central nervous system (CNS). The caustic effects of iron on the gut cause the initial symptoms of vomiting, diarrhea, and abdominal pain. Hemorrhagic necrosis of gastric or intestinal mucosa can lead to bleeding, perforation, and peritonitis.3 Unbound (free) iron moves into cells and localizes near the mitochondrial cristae, resulting in uncoupling of oxidative phosphorylation and impairment of adenosine triphosphate synthesis. Cell membranes are injured by free radical–mediated lipid peroxidation.3,6 Iron increases capillary permeability and both arteriolar dilation and venodilation, resulting in hypotension. Direct myocardial toxicity decreases cardiac output. Hydration of the iron molecule creates an excess of unbuffered protons, worsening metabolic acidosis.3 These effects, combined with severe gastrointestinal fluid losses, can lead to shock, cardiovascular collapse, and death.3 The clinical effects of acute iron poisoning occur in five stages. Not every patient goes through every phase. Phase I reflects the corrosive effects of iron on the gut. Vomiting occurs within 80 minutes of ingestion in more than 90% of symptomatic cases. Diarrhea, which can be bloody, soon follows. Phase II represents an apparent (but not complete) recovery that lasts less than 24 hours but can extend up to 2 days. Most patients recover after this point. Phase III is characterized by the recurrence of gastrointestinal symptoms, severe lethargy or coma, anion gap metabolic acidosis, leukocytosis, coagulopathy, renal failure, and cardiovascular collapse. Serum iron levels may have fallen to normal during this phase because of distribution of iron into the tissues. Metabolic derangements due to iron poisoning include hypoglycemia, leukocytosis, and severe lactic acidosis from hypoperfusion and interference with cellular respiration. Early coagulation defects are probably related to direct effects of iron on vitamin K–dependent clotting factors.7 Later coagulation defects are due to hepatic failure. Hypoglycemia and elevations of bilirubin and aspartate and alanine transaminases are other markers of hepatotoxicity. Phase IV, characterized by fulminant hepatic failure, occurs 2 to 5 days after ingestion. This is relatively rare, appears to be dose related, and is usually fatal.8 Phase V represents the consequences of healing of the injured gastrointestinal mucosa. It is characterized by pyloric or proximal bowel scarring, which is sometimes associated with obstruction. The presence of gastrointestinal symptoms suggests a potentially serious ingestion, whereas their absence is reassuring.5 A serum iron level measured at its peak, 3 to 5 hours after ingestion, is the most useful laboratory test to evaluate the potential severity of an iron overdose. Sustained-release or enteric-coated preparations may have erratic absorption, so a second level 6 to 8 hours after ingestion should also be checked. Peak serum iron levels below 350 µg/dL are generally associated with minimal toxicity; 350 to 500 µg/dL, with moderate toxicity; and above 500 µg/dL, with potentially severe toxicity (Table 157-2).5 Because iron is rapidly cleared from the serum and deposited in the liver, the level of iron after a substantial ingestion may be deceptively low if it is measured after its peak. TIBC is a crude test and is not useful to gauge the severity of iron poisoning.9 Table 157-2 Toxicity of Iron by Amount Ingested and Peak Serum Levels When serum iron levels are not immediately available, elevations of the serum glucose level above 150 mg/dL and leukocyte count above 15,000 are 100% specific for prediction of serum iron levels of more than 300 µg/mL. However, a sensitivity of only 50% limits their sole use as indicators of toxicity.10 Most tablets that contain a significant amount of elemental iron are radiopaque, although a false-negative radiograph may occur with chewable, liquid, and completely dissolved iron compounds. The presence of tablets on a radiograph correlates with the severity of the ingestion (Fig. 157-1).11,12 Repeated radiographs can also demonstrate the efficacy of gastrointestinal decontamination efforts. Decontamination may prevent absorption of additional iron from the gastrointestinal tract and can be performed concomitantly with interventions that address drug that has already been absorbed (see later section on deferoxamine). Activated charcoal does not bind iron, and neither gastric lavage nor ipecac effectively removes large numbers of pills. Iron tablets clump together as their outer coatings dissolve, often forming large pharmacobezoars. Whole-bowel irrigation is generally the preferred method of decontamination for significant iron ingestions.13 This recommendation is supported by the position statement of the American Academy of Clinical Toxicology and the European Association of Poison Centres and Clinical Toxicologists; it is based on case reports and the lack of effective alternative decontamination techniques for this potentially deadly toxin.14 For significant ingestions (>20 mg/kg of elemental iron), especially when tablets are identified on the abdominal radiograph, whole-bowel irrigation with a polyethylene glycol–electrolyte lavage solution (PEG-ELS; CoLyte, NuLytely, or GoLytely) should be initiated.14 The solution is either taken orally or, more often, administered through a small nasogastric tube.15 The usual rate of administration of PEG-ELS is 20 to 40 mL/kg/hr in young children and 1.5 to 2 L/hr in teenagers or adults, continued until the rectal effluent is clear and there is no radiographic evidence of pill fragments. This technique has been used in children, adolescents, and pregnant women without serious complications or electrolyte disturbances.13,16,17 Common side effects include nausea, vomiting, abdominal cramping, and bloating. Whole-bowel irrigation is contraindicated in the presence of bowel obstruction, perforation, or ileus.14 Hemodialysis and hemoperfusion are not effective in the removal of iron because of its large volume of distribution. Early exchange transfusions have been recommended for severely symptomatic patients with serum iron levels exceeding 1000 µg/dL.18,19 Deferoxamine chelates iron to form the water-soluble compound ferrioxamine, which is renally excreted and can be dialyzed; 100 mg will chelate 9.35 mg of elemental iron.3 Deferoxamine may also limit the entrance of iron into the cell and chelate intracellular iron. Because of its short half-life, it is administered as a continuous infusion at 15 mg/kg/hr for up to 24 hours.20 The maximum rate of administration is 35 mg/kg/hr. Rapid administration of deferoxamine can lead to hypotension, which resolves by reducing the initial rate of the infusion and slowly increasing it to the desired rate. Pregnancy is not a contraindication to deferoxamine.4,21,22 However, the pre-pregnancy weight should be used to calculate the dose. Deferoxamine can falsely lower serum iron levels, so measurements should be taken before its administration.23 The presence of ferrioxamine turns the urine a “vin rosé” color, which reflects the excretion of chelated iron. The deferoxamine challenge test, which relied on detection of this color change, has been used to detect the presence of free iron in the serum. However, the color change is difficult to detect, especially when the urine is dilute, with false-negative results even in cases of serious poisoning.24 Deferoxamine has been associated with acute respiratory distress syndrome and also with Yersinia sepsis. The pulmonary complications are usually related to high-dose deferoxamine for durations longer than 24 hours.20 The presence of fever and sepsis in a patient who has recently been treated for iron poisoning should prompt suspicion for Yersinia sepsis.25,26 The asymptomatic patient who is reliably known to have ingested less than 20 mg/kg of elemental iron and has a normal abdominal radiograph can be observed without further therapy. The patient can be discharged if he or she remains asymptomatic after 6 hours of observation.5 The patient who has ingested more than 20 mg/kg of elemental iron or has pills visible on an abdominal radiograph should receive whole-bowel irrigation.23 Follow-up abdominal radiographs can verify adequate gastrointestinal decontamination. The serum iron concentration should be checked 3 to 5 hours after ingestion. A second iron level 6 to 8 hours after ingestion should be decreasing. If peak levels are less than 300 µg/dL and are not rising and the patient is asymptomatic during 6 hours of observation, the patient can be discharged home. Moderate gastrointestinal toxicity can be expected with peak levels of 300 to 500 µg/dL. Deferoxamine should be used if these patients have symptoms of systemic toxicity evidenced by metabolic acidosis, repetitive vomiting, toxic appearance, lethargy, hypotension, or signs of shock. Patients with a serum iron level above 500 µg/dL require chelation with deferoxamine regardless of symptoms.4 If serum iron levels are not available, a normal serum glucose level and leukocyte count suggest a low iron level; if there are no signs or symptoms of toxicity during the 6-hour postingestion period and the abdominal radiographs do not show pills in the gastrointestinal tract, the patient can be sent home. Lead poisoning is a disease of industrialization and has become the most common environmental toxicologic problem in the United States.27 Most exposures are from inhalation of lead dust or fumes or ingestion of contaminated substances, such as paint chips. Less often, it results from direct skin contact with organic lead compounds or from retained bullets in or near joints.28 Approximately 3 to 4 million children (1 in 20) in the United States have toxic blood lead levels (BLLs), defined currently as levels exceeding 10 µg/dL.29 Although the addition of lead to household paint and gasoline was banned in the United States in the 1970s, residual lead-based paint is still found in 30 million homes.29 Other sources of toxic lead ingestions include curtain weights, buckshot, fishing weights, lead-contaminated soil or water, bootleg whiskey (“moonshine”), food or beverages stored or prepared in lead-soldered cans, lead-glazed pottery, and lead crystal decanters.30 Herbal and folk remedies, toys, and numerous products imported from Asia and Mexico can also contain dangerous amounts of lead.31,32 This has resulted in multiple drug and toy recalls in the United States. Lead found in buckshot can cause toxic effects in those who eat wild game.33 There is no known physiologic need for lead. Lead binds to sulfhydryl groups and other ligands and interferes with critical enzymatic reactions.12 Its toxic effects are most prominent in the hematopoietic, neurologic, and renal systems.34 Anemia, the classic manifestation of hematopoietic toxicity, may be either normochromic or hypochromic. The severity of the anemia correlates directly with the BLL. Inhibition of heme biosynthesis results in the accumulation of heme precursors, such as D-aminolevulinic acid and protoporphyrin. In the peripheral nervous system, segmental demyelination and degeneration of motor axons result in peripheral neuropathies. Wristdrop and footdrop are characteristic of adult lead poisoning. Lead toxicity also causes a host of neuropsychiatric disorders. In children, elevated BLL is associated with decreased intelligence (IQ) scores, hyperactivity, decreased attention span, overaggressive behavior, learning disabilities, and criminal behavior.35–38 It has also been associated with subclinical sensorineural hearing loss.39 Lead nephropathy is characterized by fibrosis in the proximal tubules, with relative sparing of the glomeruli. Hyperuricemic gout (“saturnine gout”) can result from increased reuptake of uric acid by the tubular cells.40 Lead poisoning also correlates with hypertension.41 Adults and children with severe acute toxicity may present with lead encephalopathy associated with increased capillary permeability and cerebral edema.42,43 Acute exposure to lead can result in symptomatic poisoning. “Lead colic” is characterized by cramping abdominal pain with nausea, vomiting, constipation, and, occasionally, diarrhea.43 Other characteristic symptoms and signs of acute toxicity include fatigue, anemia, peripheral neuropathy, renal impairment, and hepatic and CNS dysfunction. The CNS toxicity may be manifested as mild headache or personality changes to full-blown encephalopathy with coma, convulsions, and papilledema. Permanent neurologic and behavioral sequelae may occur. Although capillary lead levels correlate well with BLLs, the most informative biomarker is a BLL.44–46 The Centers for Disease Control and Prevention has defined a chronic BLL of more than 10 µg/dL as toxic for a child. Acute exposure can result in levels above 100 µg/dL (Table 157-3). Other ancillary data include findings on complete blood cell count, serum glucose level, blood urea nitrogen and creatinine concentrations, electrolyte levels, and urinalysis. A peripheral smear may show basophilic stippling. Markers of hepatic injury may be elevated after acute exposure. Because lead-containing paints and objects are radiopaque when lead is present in sufficient quantities, radiographs can confirm acute ingestion and also monitor the effectiveness of whole-bowel irrigation. In cases of altered mental status, seizures, or coma, a computed tomography scan of the head will show cerebral edema associated with acute lead encephalopathy and rule out other causes of these symptoms. In children, plain radiographs of the wrist and knees may show increased metaphyseal activity manifested as “lead bands” or “lead lines” that are characteristic of chronic exposures. Acute lead encephalopathy can be rapidly fatal. The initial goals in management are identification and treatment of all life-threatening conditions, followed by prevention of further exposure to lead, minimization of ingested lead absorption, enhancement of its elimination, and prevention or reversal of pathologic cell changes. Standard measures to control cerebral edema, including intubation and neurosurgical consultation for invasive monitoring of intracranial pressure, are indicated. When a severe poisoning is associated with recent ingestion or if radiopacities are seen on the radiograph, decontamination with whole-bowel irrigation should be considered.47,48 This intervention has not been prospectively studied but has been successful in case reports.14 Activated charcoal does not adsorb lead and should not be used.
Heavy Metals
Iron
Principles of Disease
Pathophysiology
Clinical Features
Diagnostic Strategies
ELEMENTAL IRON (mg/kg)
PEAK SERUM IRON LEVEL (µg/dL)
TOXICITY
<20
50-150
None
20-40
150-300
Mild
40-60
300-500
Moderate
>60
>500
Severe
Management
Deferoxamine
Disposition
Lead
Principles of Disease
Pathophysiology
Clinical Features
Diagnostic Strategies
Management

Full access? Get Clinical Tree


Heavy Metals
Only gold members can continue reading. Log In or Register to continue