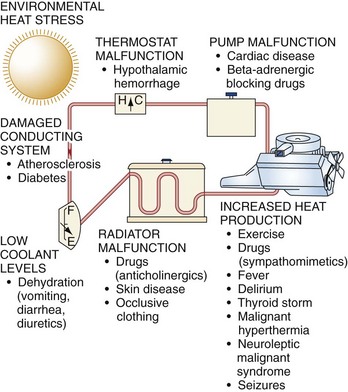
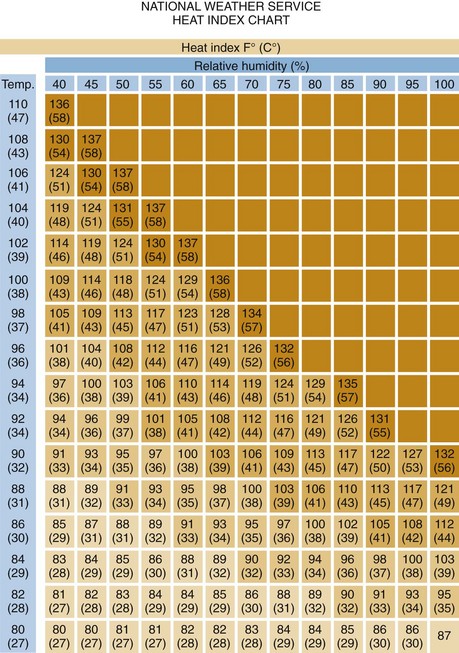
Chapter 141 Humans have been plagued by heat illness throughout recorded history, often as the result of military exercises, athletic events, or recreational activities. When environmental heat stress is maximal, strenuous exercise is not required to produce heat illness. The ancient Greeks named a disease that resembled heatstroke siriasis after the dog star Sirius, which accompanies the summer sun. The U.S. Army reported at least 125 deaths from heatstroke during basic training in the years 1941 to 1944.1 Modern military organizations continue to encounter heat illness because of the requirement to train unacclimatized troops with forced heavy physical exercise. Furthermore, athletes are prone to heat illness; heat stroke is the third leading cause of death among all U.S. athletes. In particular, football has the greatest number of heat stroke fatalities and a 10 times higher rate for heat illness, resulting in time lost from high school athletic activities.2,3 The elderly and poor, often lacking adequate air conditioning and nutrition, and those with preexisting disease are prone to heat illness during environmental extremes. In heat wave years in the United States, approximately 10 times as many deaths are reported as during non–heat wave years. It is also estimated that at least 10 times as many heat-aggravated illnesses occur because of myocardial infarction, cerebrovascular accident, and other causes. More than 700 excess deaths were caused by the heat during the 1995 heat wave in Chicago. The heat wave during the summer of 2003 is estimated to have caused 14,800 deaths in France, and climate models suggest an increase in both frequency and intensity of heat waves in temperate areas in the future.4 Heat production can be increased up to 20-fold by strenuous exertion. Rectal temperatures as high as 42° C are recorded without ill effects in trained marathon runners. Metabolic factors, such as hyperthyroidism and sympathomimetic drug ingestion, can dramatically increase heat production. Environmental heat not only adds to the heat load but also interferes with heat dissipation. The physics of heat transfer as it relates to human physiology involves four mechanisms: conduction, convection, radiation, and evaporation.5 Conduction.: Conduction is the transfer of heat energy from warmer to cooler objects by direct physical contact. Air is a good insulator; therefore, only approximately 2% of the body heat loss is by conduction. In contrast, the thermal conductivity of water is at least 25 times that of air. Convection.: Heat loss to air and water vapor molecules circulating around the body is termed convection. As ambient temperature rises, the amount of heat dissipated by convection becomes minimal, and once air temperature exceeds the mean skin temperature, heat is gained by the body. Convective heat loss varies directly with wind velocity. Loose-fitting clothing maximizes convective (and also evaporative) heat loss. Radiation.: Radiation is heat transfer by electromagnetic waves. Although radiation accounts for approximately 65% of heat loss in cool environments, it is a major source of heat gain in hot climates. Up to 300 kcal/hr can be gained from radiation when a person is directly exposed to the hot summer sun.6 Evaporation.: Evaporation is the conversion of a liquid to the gaseous phase. Evaporation of 1 mL of sweat from the skin cools the body by 0.58 kcal. As ambient temperature rises, evaporation becomes the dominant mechanism of heat loss. Panting mammals such as dogs have an oropharyngeal countercurrent flow mechanism (carotid rete mirabile) that results in selective cooling of the brain. In humans, respiratory and countercurrent mechanisms are minimal sources of heat loss, and the dominant mode of cooling in hot conditions is evaporation of sweat from the skin. Thermosensors.: Temperature-sensitive structures are located both peripherally in the skin and centrally in the body. Skin temperature changes, however, correlate poorly with changes in the rate of heat loss.7 Thermosensitive neurons are in the preoptic anterior hypothalamus. They are activated when the temperature of the blood circulating through that area exceeds a “set point.” The skin temperature affects heat loss because a person resting in a warm environment initiates sweating, even though the core temperature remains constant. In contrast, changes in core temperature are more potent than skin temperature changes in producing heat-dissipating responses.8 Central Integrative Area.: The central nervous system (CNS) interprets information received from the thermosensors to properly instruct thermoregulatory effectors. The concept of a central thermostat by which an alteration shifts effector thresholds in the same direction fits a variety of clinical situations. For example, fever, the circadian rhythm of temperature variation, and the 0.5° C difference in rectal temperature after ovulation can be explained by variation of a thermal set point. Thermoregulatory Effectors.: Sweating and peripheral vasodilation are the major mechanisms by which heat loss can be accelerated. In a warm environment, evaporation of sweat from the skin is the most important mechanism of heat dissipation. Heat loss from the skin by convection and radiation is maximized by increased skin blood flow to facilitate sweating. The vascular response to heat stress is cutaneous vasodilation and compensatory vasoconstriction of splanchnic and renal beds. These vascular changes are under neurogenic control and allow heat to be dissipated quickly and efficiently, but they place a tremendous burden on the heart.9 For blood pressure to be maintained, cardiac output increases dramatically. For this reason, saunas and hot tubs may be dangerous for patients with cardiac disease. Cardiovascular and baroreceptor reflexes also affect skin blood flow. Reduced forearm sweating and vasodilation are observed in severely dehydrated subjects exercising in a warm environment.10 Acclimatization is defined as “a constellation of physiologic adaptations that appear in a normal person as the result of repeated exposures to heat stress.” Daily exposure to work and heat for 100 min/day results in near-maximal acclimatization in 7 to 14 days. This is characterized by an earlier onset of sweating (at a lower core temperature), increased sweat volume, and lowered sweat electrolyte concentration. Acclimatization is hastened by modest salt deprivation and delayed by high dietary salt intake. As acclimatization proceeds, the sweat sodium concentration decreases while the volume increases.11 The cardiovascular system plays a major role in both acclimatization and endurance training, largely resulting from an expansion of plasma volume.12 Heart rate is lower and associated with a higher stroke volume. Other physiologic changes include earlier release of aldosterone, although acclimatized individuals generate lower plasma levels of aldosterone during exercise heat stress. Total body potassium depletion of up to 20% (500 mEq) by the second week of acclimatization can occur as a result of sweat and urine losses coupled with inadequate repletion.12 Although many similarities exist between thermoregulatory responses to heat and exercise, the well-conditioned athlete is not necessarily heat acclimatized. For heat and exercise-induced adaptive responses to be maintained, heat exposure needs to continue intermittently at least on 4-day intervals. Plasma volume decreases considerably within 1 week in the absence of heat stress.12 Predisposing Factors for Heat Illness The goal is to maximize voluntary fluid intake and gastric emptying so that fluid can rapidly enter the small intestine, where it is absorbed. Gastric emptying is accelerated to 25 mL/min by large fluid volumes (500-600 mL) and cool temperatures (10-15.8° C). High osmolality inhibits gastric emptying; osmolality of less than 200 mOsm/L is optimal. Most commercially available electrolyte solutions contain excessive sugar. Hydration can be monitored by measurement of body weight before and after training or athletic competition. An athlete with a loss of 2 or 3% body weight (1.5-2 L in a 70-kg man) should drink extra fluid and be permitted to compete only when body weight is within 0.5 to 1 kg (1 or 2 pounds) of the starting weight on the previous day. A weight loss of 5 or 6% represents a moderately severe deficit and usually is associated with intense thirst, scanty urine, tachycardia, and increase in rectal temperature of approximately 2° C. Such athletes should be restricted to light workouts after hydration until they return to normal weight. A loss of 7% or more of body weight represents severe water depletion; participation in sports should not be permitted until the athlete is examined by a physician. Wrestlers frequently fast, restrict food and fluid intake, and exercise vigorously wearing vapor-impermeable clothing to lose weight quickly so that they can compete in a lower weight class.13 Evaporative cooling can be lost when clothing inhibits air convection and evaporation. Loose-fitting clothing or ventilated fishnet jerseys allow efficient evaporation. Light-colored clothing reflects rather than absorbs light. Water evaporated from clothing is much less efficient for body cooling than is water evaporated from the skin.14,15 The body’s heat dissipation mechanisms are analogous to the cooling system of an automobile (Fig. 141-1). Coolant (blood) is circulated by a pump (heart) from the hot inner core to a radiator (skin surface cooled by the evaporation of sweat). Temperature is sensed by a thermostat (CNS), which alters coolant flow by a system of pipes, valves, and reservoirs (vasculature). Failure of any of these components can result in overheating. Radiator function depends on the skin and sweat glands. Occlusive, vapor-impermeable clothing hinders evaporative and convective cooling. Anticholinergic medications and some drugs of abuse interfere with sweating and produce heat illness.11 Various skin diseases, including miliaria (prickly heat rash), extensive burns, scleroderma, ectodermal dysplasia, and cystic fibrosis, are risk factors. Anhidrosis can be secondary to either central or peripheral nervous system disorders as well. Increased heat production causing heat illness most often accompanies exercise in hot, humid environments. Athletes and military recruits are commonly affected. When heat and humidity are extreme, exertion is not necessary to produce heat-related problems. Several indices help objectify heat strain. The indices can be divided into two categories: heat scales that are based on meteorologic parameters only and heat scales that combine environmental and physiologic parameters.16 The wet bulb globe temperature heat index is an excellent meteorologic measure of environmental heat stress (Box 141-1). It includes the effects of temperature, humidity, and radiant thermal energy from the sun. When climatic conditions exceed 25° C wet bulb, even healthy people are at high risk if they choose to exercise. Above 28° C, exercise and strenuous work should be avoided or limited to extremely short periods.17 The heat strain index is widely accepted as an example of an index that includes environmental and physiologic factors. There are several variations and modified heat strain indices in existence, with varying ease of use and accuracy (Fig. 141-2).16 Before the advent of air conditioning, mortality increased threefold to fivefold in nursing homes and threefold in the general population during heat waves. Mortality in geriatric patients correlates with average weekly peak air temperature. Most deaths in the 2003 European heat wave occurred in elderly patients. Microclimates conducive to heat illness are produced in the interiors of automobiles, tanks, and tents in the sun as well as in engine rooms, hot tubs, and saunas.4 Children are more susceptible to heat stressors because the higher surface area–to–mass ratios allow increased absorption of heat. They also have lower sweat rates per gland.18 Endogenous factors, such as hyperthyroidism and pheochromocytoma, can also drastically increase heat production. An overdose of sympathomimetics or stimulants, such as amphetamines, cocaine, and phencyclidine, can cause fatal hyperpyrexia. High ambient temperature is associated with a significant increase in mortality from cocaine overdose. Many younger patients who die of hyperthermia test positive for cocaine.19 Heatstroke can occur with delirium resulting from ethanol withdrawal.20 There are also reports of heatstroke occurring in well-trained military soldiers or athletes who ingest dietary supplements containing ephedrine or the ergogenic aid creatine.21,22 Certain patients undergoing general anesthesia rapidly experience severe hyperthermia, muscle rigidity, and acidosis. This syndrome, termed malignant hyperthermia, is the result of a genetically determined instability of skeletal muscle sarcoplasmic reticulum that allows inappropriate intracellular calcium release. Dantrolene, which lowers myoplasmic calcium, is effective in the prevention and treatment of this syndrome.23 Malignant hyperthermia is rarely seen in outpatient settings, but a clinically similar entity, neuroleptic malignant syndrome, is often encountered. This syndrome is induced by antipsychotic medications and is characterized by muscle rigidity, severe dyskinesia or akinesia, hyperthermia, tachycardia, dyspnea, dysphagia, and urinary incontinence. Although the lead-pipe rigidity and hyperthermia are reminiscent of malignant hyperthermia, the putative mechanism is different. Dopamine receptor blockade in the corpus striatum caused by butyrophenones and similar agents produces severe muscle spasticity and dystonia, leading to overproduction of heat. Some antipsychotics also cause suppression of thirst recognition. Other miscellaneous risk factors include obesity.24 Individuals with a history of heatstroke, with or without an inherent aberration that predisposed them to the initial episode, are at increased risk for a recurrence. It is both diagnostically and therapeutically important to identify patients suffering from a febrile response rather than heat illness. For many years, fever was attributed to pyrogens released by bacteria or viruses (exogenous pyrogens) or to cells undergoing autolysis after phagocytic activity (endogenous pyrogens).25 These circulating pyrogens would directly affect the thermoregulatory control center. It now appears that fever is the result of triggering by pyrogens of pathways involving cytokine receptors or other signals to reset the thermal set point in the preoptic area of the anterior hypothalamus to a new level above 37° C.25 Because fever is the product of a molecular interaction that establishes a new physiologic thermal set point, therapeutic attempts to lower temperature are opposed by body mechanisms that attempt to maintain the new set point. Thus attempts at whole-body cooling produce violent shivering and discomfort.26 The use of agents to block the causative molecular interaction is the most clinically effective approach. Antipyretics block the action of the pyrogen at hypothalamic receptor sites through inhibition of prostaglandin synthesis.27 These antipyretics are not effective against and should not be used to control environmental hyperthermia. Heat cramps are brief, intermittent, and often severe muscle cramps occurring typically in muscles that are fatigued by heavy work. Heat cramps appear to be related to a salt deficiency. Heat cramps occur most commonly during the first days of work in a hot environment and develop in persons who produce large amounts of thermal sweat and subsequently drink copious amounts of hypotonic fluid.28 Athletes, roofers, steel workers, coal miners, field workers, and boiler operators are among the most common victims of heat cramps. Heat cramps tend to occur after exercise when the victim stops working and is relaxing (Box 141-2). In this respect, they differ from the cramps experienced by athletes during exercise, which tend to last for several minutes, are relieved by massage, and resolve spontaneously.
Heat Illness
Perspective
Principles of Disease
Heat Production
Heat Regulation
Acclimatization
Pathophysiology
Fever versus Hyperthermia
Minor Heat Illness
Physiology
Clinical Factors

Full access? Get Clinical Tree


Heat Illness
Only gold members can continue reading. Log In or Register to continue
 extreme danger
extreme danger danger
danger



