Headaches
Jay E. Selman MD
INTRODUCTION
By age 15 years, 50% of children will have experienced at least one headache (Scheller, 1995). Effective management requires recognition and classification of the headache type, appropriate evaluation, selection and monitoring of therapeutic interventions, and family support. When the headaches do not follow the expected course, neurologic consultation is necessary. This chapter provides a framework for the diagnosis and management of both migraine and nonmigraine headaches in children and adolescents.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Understanding the anatomic sites from which pain can emanate is important in the evaluation and treatment of headaches. The major anatomic structures with pain receptors include the cranium; musculoskeletal attachments; and ophthalmologic, otorhinolaryngologic, and dental structures. Cranial structures include the scalp, periosteum, meninges, and large arteries and veins.
Major ophthalmologic pathologic processes involved in headaches include infection and inflammation of the globe, conjunctivae, sclerae, and adnexa, as well as glaucoma (increased intraocular pressure). Refractive errors seldom cause headaches. Screening with the Snellen chart can reassure the family.
Otorhinolaryngologic etiologies include sinusitis, otitis media, pharyngeal irritation and infection, peritonsillar abscess, and glossopharyngeal nerve irritation (Bordley & Bosley, 1973). Dental causes include temporomandibular joint (TMJ) dysfunction and pathologic processes within the tooth, including the pulp, dentin, cementum, and the periodontal structures. Dental pain is usually identifiable by inspection, application of heat, local pressure, or percussion. TMJ syndrome occurs in children and adolescents. Dental consultation can provide additional help.
Pathophysiologic theories of migraine etiology include the vascular, neurogenic, unified or neurovascular, and serotonergic. The vascular hypothesis postulates that neurologic symptoms, such as aura, result from intracranial vasoconstriction, whereas pain follows extracranial vasodilation. The neurogenic hypothesis attempts to explain the spreading wave of reduction in cerebral blood flow (oligemia), which has been documented in special studies of patients having actual migraine headaches. This pattern typically begins over the occipital area and spreads anteriorly. The current hypothesis states that the altered neuronal function results in oligemia.
The unified, or neurovascular, hypothesis unifies these two mechanisms and relates a complex interaction between the trigeminal-vascular complex, intracranial vessels, brainstem, and cortical structures and events. Individuals who are susceptible to migraine may have a “central neuronal hyperexcitability,” which reduces the threshold for headaches. Certain factors (eg, dietary, hormonal, hereditary) may trigger the release of serotonin and norepinepherine from neurons in the locus ceruleus and the dorsal raphe of the brainstem. This cascade of events leads to the manifestations of the migraine headache. Once activated, the neurons release vasoactive peptides, such as calcium gene related protein, substance P, and acetylcholine, which cause a “sterile” inflammatory response and vasodilation (Waeber, 1998; Sarhan, 1998). The trigeminal nerve, which innervates many cranial vessels, carries impulses to the remainder of the brain, which interprets the signals as pain.
The serotonergic (5-hydroxytriptamine [5-HT] or serotonin) hypothesis builds on the preceding model, because the nerve cells of the dorsal raphe are serotonergic. Possible explanations of serotonergic imbalance, which appears to play a key role in migraine headaches, include suboptimal 5-HT synthesis, unstable 5-HT complexes, excessive metabolism of 5-HT, and defects in 5-HT receptor function. The 5-HT1 receptor agonists, such as rizatriptan, sumatriptan, and ergotamine, ameliorate or abort the migraine attacks, while the 5-HT2 receptor antagonists, including the tricyclic antidepressants and methysergide, are prophylactic agents. The much-improved efficacy and side-effect profile of the triptan drugs (eg, sumatriptan, rizatriptan, naratriptan) probably reflect their specificity as compared with other drugs, such as the tricyclics, β-blockers, and methysergide, which affect many other neurotransmitter systems.
Some researchers believe that all headaches, including tension type and migraine, belong to a single clinical spectrum related to the same basic etiology but differing in clinical manifestations. However, clinical management requires consideration of the epidemiology and management of each type separately.
HEADACHE TYPES
Display 51-1 delineates the major headache types and categories, as defined in the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) and by the International Headache Society (IHS, 1997). The headache types reviewed here are the most relevant for children and adolescents.
DISPLAY 51–1 • Headache Types
Migraine
Without aura
With aura
Complicated
Basilar artery
Equivalents
Abdominal
Cyclic vomiting
Benign positional vertigo
Acute confusional state
Tension type
Episodic
Chronic
Headache caused by mass lesion
Neoplasm
Subdural hematoma
Chiari I malformation
Arteriovenous malformation
Aneurysm
Headache from other causes
Exertional
Post-shunt
Benign intracranial hypertension
Cervicogenic
Temperomandibular joint syndrome
Sinus
Post–lumbar puncture
Altitude sickness
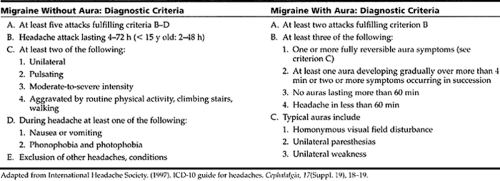
Twenty three million Americans have migraine headaches (IHS, 1997). Migraine headache can occur with or without an aura. Table 51-1 outlines the diagnostic criteria for these two most common forms of migraine headaches.
Many clinicians have suggested various modifications because they believe that the criteria delineated in Table 51-1
exclude many children and some adolescents who actually have migraine. These include reducing the duration to 1 hour and including either unilateral or bilateral localization, abdominal pain, and a family history of migraine as diagnostic criteria (Raieli et al., 1995; Scheller, 1995; Winner et al., 1995; Sweeting & West, 1998). In clinical practice most neurologists do not adhere rigidly to the criteria of the ICD-10 classification.
exclude many children and some adolescents who actually have migraine. These include reducing the duration to 1 hour and including either unilateral or bilateral localization, abdominal pain, and a family history of migraine as diagnostic criteria (Raieli et al., 1995; Scheller, 1995; Winner et al., 1995; Sweeting & West, 1998). In clinical practice most neurologists do not adhere rigidly to the criteria of the ICD-10 classification.
Although migraine auras usually precede the migraine, they may occur with the headache itself. One unusual aura variant is the “Alice in Wonderland” syndrome, in which there is visual distortion, with either micropsia or macropsia (Emergy, 1977).
Types of Migraine Headaches
Complicated migraine requires fulfilling the criteria for migraine per Table 51-1 and the presence of focal neurologic deficits for 7 days or the demonstration of ischemic infarction in an anatomically appropriate area by neuroimaging. Other causes of infarction must be excluded (IHS, 1997). Although often familial, complicated migraine requires a very thorough evaluation for vascular, inflammatory, and metabolic problems (Arroyo et al., 1990). Magnetic resonance imaging (MRI) is the preferred imaging test. MRI can reveal periventricular white matter changes that may not correlate well with neurologic deficits. However, cortical abnormalities, which can occur alone or with the periventricular changes, have a greater correspondence with clinical findings.
Patients who have had cranial irradiation for leukemia or other neoplasms (especially when accompanied by chemotherapy) may develop a migraine-like syndrome or a stroke many years later. However, the mechanism is probably different, resulting from radiation damage to the endothelium of the cranial vessels (Shuper et al., 1995).
Basilar artery migraine is a special subtype of migraine that begins in early childhood, often before 4 years of age (Barlow, 1994). Most striking is the dramatic, precipitous, and often recurrent presentation of multiple neurologic deficits, all of which are attributable to transient disturbances in the posterior circulation (vertebro-basilar artery). Symptoms include transient ataxia, vertigo, diplopia, alternating hemiparesis, facial paresis, tinnitus, hearing impairment, ataxia, vomiting, paresthesias, and depressed level of consciousness. Attacks tend to be more severe with increasing age of onset. Many children with vestibular symptoms will have labyrinthine dysfunction on electronystagmographic testing, especially if the episodes are moderate or severe (Eviator, 1981). A strong female preponderance and a very striking family history of migraine are commonly present in up to 86% of families studied, usually among female members on the maternal side.
Differential diagnoses include stroke, arteriovenous malformations (AVMs), toxic-metabolic encephalopathies, and neoplasms. Fortunately, most patients recover completely.
Although basilar artery migraines usually cease in adolescence, many patients will later develop more typical migraines.
Although basilar artery migraines usually cease in adolescence, many patients will later develop more typical migraines.
Children and adolescents presenting with possible basilar artery migraine require a thorough neurologic assessment, MRI scan, and appropriate laboratory screening.
Abdominal migraine presents with episodic abdominal pain, with or without vomiting and headaches. In a large epidemiologic survey, Abu-Arafeh and Russell (1995b) found that about 10% of a community-based sample of 1754 children ages 5 to 15 years had migraine headaches, while 4% had abdominal migraine. The clinical patterns and provoking and ameliorating factors were virtually identical in the two groups. Nevertheless, this diagnosis requires a thorough evaluation to exclude other causes of abdominal pain. A recent open-label study of 36 children with abdominal migraine revealed a 75% “excellent” response to propranolol (Inderal) and a 33% response to cyproheptadine (Worawattanakul, Rhoads, Lichtman, & Ulshen, 1999). Refer to Chapter 38 and Chapter 57 for more information about differential diagnosis of abdominal pain. Chapter 21, Chapter 23, Chapter 40, and Chapter 62 may contribute to the formulation of the differential diagnosis.
Cyclic vomiting is an uncommon “periodic” (or recurrent) syndrome in children and adolescents (Cavazzuti, 1982). The clinical characteristics are fairly stereotyped in the individual patient. Discrete episodes of vomiting, which occur without apparent triggering events, last from 1 day to several weeks, usually averaging 2 to 3 days. Withers and colleagues (1998), who studied 32 children and adolescents, reported an average of about nine attacks of cyclic vomiting per year, with two thirds of the patients missing more than 10 days of school annually. At times, the vomiting was severe enough to require hospitalization. Precipitating events included intercurrent infections and stress. In some patients, other neurologic phenomena occurred, including headaches, vertigo, hypotonia, auras, and drowsiness resembling those seen in basilar artery migraines. Although many children with cyclic vomiting later develop typical migraine syndromes, there is also an increased incidence of psychological problems.
A thorough evaluation to exclude structural disease of the central nervous system; gastrointestinal lesion disorders; metabolic encephalopathies, such as maple syrup urine disease; porphyria; and hyperammonia-related syndromes is essential (Withers et al., 1998). Butalbital and propranolol have produced equivocal responses. Gokhale and colleagues (1997) reported that using phenobarbital 30 to 120 mg at bedtime led to significant improvement. The main adverse reaction to barbiturates is hyperactivity, known to occur in up to 30% of children.
Benign positional vertigo (BPV), a periodic syndrome occurring in about 2.5% of children, causes recurrent, discrete episodes of vertigo lasting from seconds to several minutes (Britton, 1988). Nausea, vomiting, anxiety, nystagmus, vasomotor changes, and sometimes headache may accompany the episodes, although the neurologic examination and electroencephalogram (EEG) are normal (IHS, 1997). Among children with BPV, there is a 2.5-fold increase in migraine headaches, abdominal pain, and motion sickness (Abu-Arafeh & Russell, 1995a).
A careful history and examination are critical in making the diagnosis of BPV. Initial episodes or persistent neurologic deficits require a neurologic evaluation, including MRI scanning. Although rare, other conditions, such as neoplasms (medulloblastoma, meningioma), cerebellar proc-esses, and inner ear pathology (perilymphatic fistula, Meniere’s disease), may cause similar symptoms.
Acute confusional state with disorientation occurs infrequently in children after mild head injury and may recur with subsequent trauma (Gascon, 1970). As the child matures, typical migraine headaches may develop. Some cases may represent episodes of transient global amnesia that may be related to brief vasoconstriction of the arteries supplying the hippocampus (Jensen, 1980).
Epidemiology
Infancy
Although headaches can begin in infancy, the family often does not recognize such episodes as migraines (Barlow, 1994). Manifestations in infancy include vomiting, pallor, crying, and behavioral changes. As children develop the ability to communicate, parents become increasingly aware of the headaches. By 3 to 4 years of age, the child can indicate head pain.
Childhood
Epidemiologic studies from many countries and cultures confirm clinical experience that headaches occur frequently in childhood. Although the incidence is equal in both sexes in the preadolescent period, headaches occur more frequently in girls than boys in adolescence. In a general population survey of 5-year-old Finnish children, 50% had had a headache in the previous 6 months; the prevalence of migraine was 7% (Sillanpaa & Anttila, 1996). This 50% figure represents an increase in headache incidence in the intervening decades since Bille’s work in 1962. Bille’s classic study found that 2.5% of 9000 Swedish children studied had frequent headaches, with 14% having frequent migraine headaches (Bille, 1962). Psychosocial stress seems to have contributed to this increase. Other behavioral problems, including temper tantrums and stomach aches, occurred much more often in children with headaches, but the explanation of this association is unclear (Sillanpaa & Anttila, 1996).
Adolescence
A general population survey of 13-year-old Finnish children conducted in 1992 demonstrated that 51% had had a headache in the previous 6 months. Ten percent of these subjects had had a migraine in the same period (Sillanpaa & Anttila, 1996). Again, these figures suggest a significant increase in the incidence of migraine headache in the years since Bille (1962) conducted his research, finding that 16% of his Swedish subjects had recurrent headaches, with 5% having frequent migraines.
Tension-Type Headaches
Two types of tension-type headaches (TTH) occur: episodic and chronic. Episodic TTH is a very common disorder that may or may not be associated with tenderness of the pericranial muscles. Children and adolescents may have both migraine headaches and TTH. However, most TTHs are relatively mild and respond to simple analgesic treatment. Display 51-2 presents diagnostic criteria for episodic TTH.
DISPLAY 51–2 • Diagnostic Criteria for Episodic Tension-Type Headaches
At least 10 episodes fulfilling criteria B–D with fewer than 15 headache-days per month for at least 6 months, but fewer than 180 headache-days per year
Duration from 30 minutes to 7 days
Two or more of the following:
Pressing/tightening (nonpulsatile) quality
Mild-to-moderate intensity that may inhibit but not prohibit activities
Bilateral location
Not aggravated by routine activity
Both of the following:
No nausea or vomiting
Phonophobia or photophobia may be present, but not both
Absence of other specific headache disorders (eg, chronic post-traumatic)
Adapted with permission from International Headache Society. (1997). ICD-10 Guide for Headaches. Cephalalgia, 17(Suppl. 19), 14–16.
When chronic TTH exists, a careful search for possible stressors is extremely important. Because TTH can occur with migraine headaches, the clinician should evaluate both conditions. Wober-Bingol and colleagues (1996) found that
the major differentiating factors between migraine and TTH were the intensity of the headaches and the presence of nausea and vomiting. Children with TTH often report more trigger factors than those with migraine, but there is an increase in associated musculoskeletal symptoms in children with headaches, regardless of the type. Children with migraines or TTH have more somatic complaints and school absences than children without headache, especially if they have both types (Carlsson, 1996). Many adults with chronic TTH (previously known as chronic daily headaches) actually began having them in childhood or adolescence. Episodic TTH may “transform” into chronic TTH. Precipitating factors can include head, neck, or back trauma; viral illnesses; sinusitis; and surgical procedures (Marcus, Scharff, Mercer, & Turk, 1999). Display 51-3 presents the diagnostic criteria for chronic TTH.
the major differentiating factors between migraine and TTH were the intensity of the headaches and the presence of nausea and vomiting. Children with TTH often report more trigger factors than those with migraine, but there is an increase in associated musculoskeletal symptoms in children with headaches, regardless of the type. Children with migraines or TTH have more somatic complaints and school absences than children without headache, especially if they have both types (Carlsson, 1996). Many adults with chronic TTH (previously known as chronic daily headaches) actually began having them in childhood or adolescence. Episodic TTH may “transform” into chronic TTH. Precipitating factors can include head, neck, or back trauma; viral illnesses; sinusitis; and surgical procedures (Marcus, Scharff, Mercer, & Turk, 1999). Display 51-3 presents the diagnostic criteria for chronic TTH.
DISPLAY 51–3 • Diagnostic Criteria for Chronic Tension-Type Headaches
History of headaches occurring more than 15 days per month for at least 6 months, or at least 180 days per year, and criteria B–D
Must have two of the following:
Pressing/tightening pain, must be nonthrobbing
Mild-to-moderate intensity may inhibit but does not prohibit activities
Bilateral location
Not aggravated by routine physical activity
Both of the following:
No vomiting present
None or only one of the following is present:
Nausea
Photophobia
Phonophobia
Absence of other specific headache disorders (eg, chronic post-traumatic)
Adapted with permission from International Headache Society. (1997). ICD-10 Guide for Headaches. Cephalalgia, 17(Suppl. 19), 16–17.
Headache Caused by Mass Lesions
Commonly occurring lesions associated with increased intracranial pressure and headaches include neoplasms, subdural and epidural hematomas, empyemas, Chiari I malformations, AVMs, and aneurysms. The common characteristics of intracranial mass lesions include distortion and destruction of anatomic structures, obstruction of the flow of cerebrospinal fluid (CSF), and changes in the compliance of brain tissues. The rapidity of presentation is proportional to the rate of change of the mass, brain compliance, and intracranial pressure (ie, the slower the onset of the pathologic process, the later the presentation).
Intracranial neoplasms are the second most common tumor seen in children. Cohen and Duffner report the prev-alence at 2.4 per 100,000 (Swaiman, 1994). Risk factors include genetic conditions, such as neurofibromatosis, ataxia-telangiectasia, immunosuppression, and exposure to x-rays and other toxins.
Intracranial lesions develop in the supratentorial or infratentorial compartments or in the midline. Supratentorial lesions present with focal neurologic deficits, headaches, or seizures, which may be localized or generalized. Infratentorial lesions present with headaches and signs of increased intracranial pressure, visual symptoms, dyscoordination (lateral cerebellum), gait ataxia (midline or lateral cerebellum), and cranial nerve abnormalities (diplopia, facial weakness, dysphagia, dysarthria). Midline tumors typically have associated visual problems, endocrine dysfunction (eg, appetite, thirst, and growth disorders), headaches, and emotional disturbances. Acute obstruction of the aqueduct of Sylvius, which connects the third and fourth ventricles in the midline, results in rapid dilation of the frontal horns and lateral ventricles, thereby causing lethargy, vomiting, and diplopia.
A choroid cyst of the third ventricle can act as a ball-valve, causing intermittent obstruction of the CSF pathways and therefore very positionally dependent symptoms. Infraten-torial neoplasms account for approximately 50% of tumors in children younger than 12 years but decrease significantly through adolescence toward the adult pattern of 80% to 90% supratentorial and 10% to 20% infratentorial. The most typical presentation is a gradual but progressive onset of minor symptoms, such as mild headaches that will respond initially to simple analgesics.
• Clinical Pearl
Headaches associated with mass lesions increase in frequency and severity; they may be present upon awakening or will awaken the child from sleep at night or occur with exertion. As this pattern evolves, vomiting, diplopia, lethargy, and loss of neurologic function may accompany the headache. Any suspicion of an intracranial mass requires an urgent neurologic assessment.
With either subdural or epidural hematomas, the history of head trauma, albeit mild, is almost always elicitable. Typically, focal headaches begin gradually, followed by an altered level of consciousness. Focal neurologic deficits and seizures can also occur. The interval between the head trauma and the presentation of symptoms can vary significantly with subdural hematomas, which result from tearing of the bridging veins across the calvarium.
Epidural hematomas result from trauma in which lateral head injury causes shearing of the middle meningeal artery. About 70% of epidural hematomas are associated with skull fractures. Hemorrhage in the epidural space can occur immediately or after a brief period (minutes to a few hours) of relative normalcy, the “lucid period.” Once present, symptoms of increased intracranial pressure can develop very rapidly because the bleeding occurs under arterial pressure. The mortality rate approaches 25%.
When the primary care provider suspects either a subdural or epidural hematoma, an emergency computed tomography (CT) scan of the brain without contrast is mandatory. The clinician should contact both a neurologist and a neurosurgeon immediately if the CT scan confirms the diagnosis or if the child has any abnormalities on neurologic examination.
Occasionally an empyema may form in the subdural space, either directly from nearby infected sinuses or indirectly from hematogenous seeding. Headaches and fever often occur early in the process. Because these infections can rapidly cause severe disability or death, emergency neurologic, neurosurgical, and ear, nose, and throat consultations are imperative.
Chiari I malformation is a congenital anomaly, leading to displacement of the cerebellar tonsils into the spinal canal at the craniocervical junction. Although often asymptomatic for decades, some patients present with headaches in childhood or adolescence. Typically occipital or frontal, the headaches are often accompanied by neck pain, gait ataxia, dysphagia, nystagmus, and even respiratory distress. The presence of the latter is an ominous finding because rarely, Chiari I malformations can affect the brainstem respiratory centers and cause traction on the lower spinal nerves, resulting in respiratory failure and death.
An AVM is a congenital malformation that usually pre-sents as seizures or focal neurologic deficits as a result of local ischemia or hemorrhages. However, associated headaches may resemble migraine headaches or TTH.
Any patient with a persistent, unilateral headache always confined to the same side of the head may have an AVM that is leaking intermittently.
An aneurysm, a congenital malformation in the medial or muscular layer of medium and large arteries, weakens the arterial wall at the bifurcation. As individuals age, the defect tends to enlarge, thereby increasing the probability of rupture. The aneurysm can leak without rupturing completely, producing the “sentinel” or warning headache caused by blood in the subarachnoid space or a pressure effect. Meningeal symptoms can accompany these headaches. A family history of aneurysms should increase the clinician’s index of suspicion.
Headache From Other Causes
Children and adolescents experience other headaches with which the primary care provider should be familiar, including exertional, post-shunt, benign intracranial hypertension, TMJ, cervicogenic, sinus, post–lumbar puncture, and altitude sickness headaches.
Exertional headaches occur rarely in children and occasionally in adolescents. They typically develop with sudden vigorous physical exertion without warming up and with sudden physiologic activities, such as coughing, sneezing, or even yawning. Adolescents report similar headaches with sexual activity. Some patients with typical migraines note exertion as a triggering event. The differential diagnosis should include posterior fossa lesions, subdural hematoma, Chiari I malformation, congenital lesions of the craniocervical junction, and pheochromocytoma. The quality of the headache is variable but often has a throbbing or pulsatile character. Other patterns include sharp or stabbing pain that is unilateral or bilateral.
Management of exertional headaches requires an accurate diagnosis. Adequate hydration and warm-up prior to strenuous physical activity are needed to increase the cardiac output slowly. If these measures fail, then indomethacin, isometheptene (Midrin), or ergotamine tartrate can be used about 30 to 60 minutes before the activity. Propranolol is a useful prophylactic agent.
Post-shunt headaches are potentially ominous. Immediately after the procedure for obstructive hydrocephalus, usually a ventriculo-peritoneal shunt, the headaches may result from failure of the shunt apparatus (valve, tubing, connections, or obstruction of the proximal or distal ends). Subdural hematomas may result from rapid decompression of the ventricles, inward movement of the brain, and shearing of the extradural veins. After the perioperative period, the main concerns are shunt failure and infection. The latter usually presents with fever, headache, irritability, vomiting, and change in mental status. Shunt failure can cause a rapid increase in intracranial pressure, obtundation, and even death. After the shunt has been in place for several months, the brain compliance is often significantly reduced. Therefore, a small increase in the volume of CSF, caused by shunt malfunction, will result in a disproportionate elevation in intracranial pressure.
Any suspicion of shunt failure or malfunction requires an emergency pediatric neurosurgical consultation. Depending on scope of practice, the provider should know how to tap the commonly used reservoirs, because this can always be done emergently if no surgical help is available.
Benign intracranial hypertension occurs more often in adolescent females with obesity and menstrual irregularities. Potential provoking factors include the use of steroids, macrodantins, tetracyclines, fat-soluble vitamins, isoretinoin compounds (Bigby, 1988), chronic otitis media, and Lyme disease. Patients present with headaches, diplopia from sixth nerve palsy, papilledema, and vomiting. The greatest danger is sudden blindness, which can evolve rapidly in the absence of other symptoms. Treatment consists of lumbar puncture(s), acetazolamide (Diamox), steroids, and a neurologic and possibly an ophthamologic consultation. Long-term management includes a weight-loss program in obese children. In severe cases, especially when visual function is threatened, a lumboperitoneal shunt or optic nerve fenestration may be required.
Uncommon in children and adolescents, cervicogenic headaches arise in the neck region. The pain may radiate fairly widely to the temporal and frontal areas. Typically, tenderness of the cervical paraspinous muscles and loss of range of motion are the clinical highlights of this entity (Sjaastad et al., 1989). Conservative treatment with reduction of the weight of book bags, application of heat, anti-inflammatory medications, and physical therapy may be helpful.
Headaches related to TMJ dysfunction have been found in up to 80% of children, adolescents, and adults presenting to a specialized clinic for facial and myofascial pain disorders, including TMJ (Pilley et al., 1992). Other symptoms include ear pain, throat symptoms, dizziness, muffling, jaw clicking and clenching or locking, popping in and around the ear, loss of range of movement, or clicking sensation (Cooper & Cooper, 1993; Capurso et al., 1997). Examination reveals tenderness over the preauricular area. Palpation of the pterygoid muscles in the hypopharynx often identifies areas of tenderness. Many patients also complain of neck pain. More severe problems require a comprehensive dental examination, which may entail special radiographs, scintigraphic scans, or MRI scans.

Full access? Get Clinical Tree