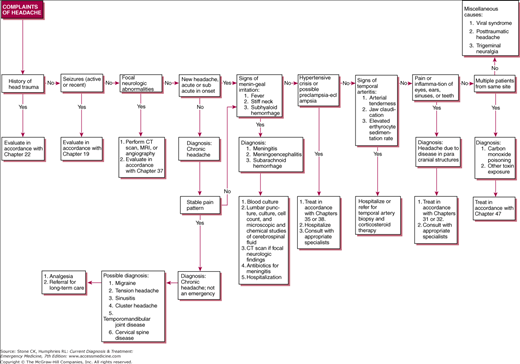
Immediate Evaluation and Management of Headache Caused by Life-Threatening Conditions
Patients may have headache following one or more grand mal seizures. However, because the seizures may themselves be due to serious underlying disease (eg, subdural hematoma), evaluation of this problem takes precedence (Chapter 19).
The presence of new focal neurologic abnormalities with headache, especially if papilledema is present as well, is strongly suggestive of a mass lesion (tumor, hematoma, abscess). Computed tomography (CT) scan or magnetic resonance imaging (MRI) should be done as soon as possible to make the diagnosis. Further evaluation is discussed in Chapter 37.
The single most important item of information to obtain from a patient with headache is whether the headache is new or acute in onset. A new headache is one occurring in a patient without a history of headaches, or a novel pattern or quality of pain in a patient with a history of headaches. A headache that is acute in onset is far more likely to have underlying pathology that may be life-threatening requiring prompt investigation.
If the headache is acute or subacute in onset, subarachnoid hemorrhage or meningitis must be suspected. The usual manifestations are signs of meningeal irritation (stiff neck; positive Kernig and Brudzinski signs) and fever. These findings may be minimal or even absent in very young or very old patients. Seizures, confusion, or coma may be present as well. Subarachnoid hemorrhage should be strongly suspected in a patient with abrupt onset of headache that is unique to the patient’s experience, especially if meningeal irritation or focal neurologic findings are present. An emergency CT scan is the initial test of choice. However, as many as 2% of patients with subarachnoid hemorrhage can have a normal CT scan within the first 12 hours after the hemorrhage begins. If the diagnosis is unclear, lumbar puncture should be performed.
Meningitis should be strongly suspected in a patient who presents with headache accompanied by fever, especially if signs of meningeal irritation are present. Antibiotic therapy should be started as soon as possible (based on microorganisms most common for each age group) before the CT scan or lumbar punctures are performed (Chapter 42). However, if there are signs of focal neurologic findings in a patient with fever, a brain abscess should be suspected and the lumbar puncture (but not antibiotics) should be delayed until a CT scan is performed.
Moderate elevations of blood pressure alone seldom cause headache; however, severe hypertension as seen in hypertensive crises and eclampsia can be associated with headache. If hypertension is present and the patient is pregnant or has signs of cerebral dysfunction (confusion, obtundation, or coma) or other end-organ damage (retinitis; nephritis with proteinuria), a life-threatening emergency exists.
Note: In pregnancy, a slight increase in blood pressure may be more significant than in the nonpregnant patient. See Chapter 34 (see Hypertensive Crisis) or Chapter 38 (see Eclampsia).
Temporal arteritis is a rare but treatable disease with serious sequelae that must be considered in every elderly patient with new headache. The principal manifestations are headache with temporal artery tenderness (not found in every case) and a markedly elevated erythrocyte sedimentation rate. Sudden irreversible monocular blindness may occur. If this condition is suspected, immediate treatment with steroids is indicated and hospitalization should be considered to confirm the diagnosis by means of temporal artery biopsy.
New or acute headaches are often caused by disease in the eyes, ears, sinuses, or teeth. Look carefully for iritis or acute glaucoma (Chapter 31) or for sinusitis, otitis media, or dental caries or abscess (Chapter 32). Treatment should be focused on the primary condition.
Multiple patients from the same vicinity with complaint of headache suggest carbon monoxide poisoning or other toxin exposure. Patients should be questioned specifically about heating sources (eg, gas heat or oven), burning materials (eg, charcoal) in poorly ventilated areas, use of household cleaners, or other chemical exposure. Specific treatment of carbon monoxide poisoning and other toxin exposure is discussed in Chapter 47.
Even after careful initial history and physical examination, the diagnosis may not be apparent in the patient with new headache. Patients with recent onset of new headache should be hospitalized if there is any suspicion of a life-threatening process. Increasing severity of subacute headache over days or weeks, even without focal signs, suggests serious intracranial disease, and the patient should undergo appropriate diagnostic procedures. Subacute headaches without progressive symptoms and chronic headaches may be referred and evaluated on a nonemergency basis.
Approach to the Diagnosis of Headache
Headache is caused by traction, displacement, inflammation, or distention of pain-sensitive structures in the head or neck. Disorders of the scalp, teeth, eyes, and ears and of the mucous membranes of the nose, sinuses, and oropharynx can produce pain. Pain-sensitive structures about the calvarium include the scalp and its blood vessels, the neck muscles, and the upper cervical nerves. The skull, brain, and most of the dura are not pain sensitive. In general, discrete intracranial lesions above the cerebellar tentorium produce pain in trigeminal distribution (anterior to ears), whereas lesions in the posterior fossa project pain to the second and third cervical dermatomes (posterior to ears).
Chronic headache (duration of months or more) is usually not due to a serious disorder, but headache of acute onset or of a changing pain pattern demands prompt evaluation in the emergency department. If the patient has a chronic headache disorder, determine whether the present headache differs from or is identical to the patient’s chronic problem. Headaches in the early morning or those causing waking may indicate an increase in intracranial pressure and prompt an evaluation for intracranial tumor.
Primary headache disorders such as migraine and tension headaches commonly have a family history of headaches.
Hemicranial or retroocular pain.
Commonly diffuse, occipital, or bandlike pain.
Often focal (“right here”).
Stabbing pain localized to the second or third division of the trigeminal nerve.
Commonly described as throbbing and often preceded by prodromal symptoms or auras, for example, scintillating scotomas or other visual changes.
Usually steady pain.
A shooting or stabbing character.
Commonly maximal on awakening.
Frequently awaken patients from sleep and often recur at the same time of day or night.
May develop at regular intervals, especially with recurrent stressful situations.
Frequently relieved by pressure on the ipsilateral temporal or carotid artery; by darkness, sleep, or vomiting; or during pregnancy.
Often exacerbated by events such as coughing and sneezing that transiently raise intracranial pressure.
Tension, emotional stress, and fatigue.
Hunger, nitrite-containing foods (hot dogs, salami, sausage), chocolate, aged cheeses, bright lights, menses, alcohol, caffeine, monosodium gluta-mate, aspartame, and insomnia.
Alcohol.
Chewing and eating.
Nausea or vomiting is common with migraine and posttraumatic headache syndromes and may be seen late in the course of mass lesions. Photophobia is prominent with migraine headache but occurs also with meningitis, especially viral (aseptic) meningitis. Myalgias of pericranial muscles (eg, posterior neck muscles) often accompany tension headaches and viral syndromes. Rhinorrhea and lacrimation during headache typify the cluster variant of migraine and are ipsilateral to the pain.
Has the headache that the patient is presenting with previously been evaluated, and what tests (CT scan, MRI, lumbar puncture, pertinent laboratory data) have been performed?
Find out what medications have worked in the past for this patient and if the patient commonly takes medications for prevention of headache. Clinical response of decreased pain to a medication should no be used as a lone indicator of a benign etiology of the headache.
The presence of fever supports a diagnosis of meningitis, encephalitis, or headache associated with viral infection. A low-grade fever may also occur in temporal arteritis.
Hypertension per se rarely causes headache, but chronic hypertension is the major risk factor for stroke, especially intracerebral hemorrhage. Intracerebral hemorrhage may be associated with acute headache. Blood pressure may be markedly elevated during hypertensive encephalopathy or as a result of preeclampsia–eclampsia, subarachnoid hemorrhage, or brain-stem stroke.
Neurofibromas or café au lait spots of Recklinghausen disease may be associated with benign or malignant intracranial tumors.
Cutaneous angiomas sometimes accompany arteriovenous malformations of the central nervous system; rupture results in subarachnoid hemorrhage and acute headache.
Note nodularity or tenderness compatible with temporal arteritis.

Full access? Get Clinical Tree