Head Trauma: Medical Management
James Hutchison MD, FRCPC, FAAP
Anne-Marie Guerguerian MD, FAAP, FRCPC
EPIDEMIOLOGY AND ETIOLOGY
Most children with multiple trauma are at risk of secondary hypoxic-ischemic brain injury due to shock, hypotension, hypoxia, and intracranial hypertension.3, 4, 5, 6, 7, 8 and 9
Injuries are most commonly due to motor vehicle collisions, falls, and bicycle and sports related injuries.1
Most head injuries are caused by blunt trauma.
Head trauma secondary to child abuse is most common in infants and is associated with a higher mortality.10
Males are more commonly injured than females.
The peak incidences occur in toddlers and adolescents.
Diffuse axonal injury (shear injury of the white matter) is more common and intracranial hematomas requiring surgical evacuation are less common in children than in adults.
Current CT imaging techniques underestimate diffuse axonal injury; therefore children can have severe diffuse axonal injury with only subtle or no focal white matter lesions visible on CT imaging.
Epidural hematomas are a neurosurgical emergency and most often follow trauma to the temporal region.
There may be a period of consciousness followed by rapid deterioration and coma.
See Chapter 6 on Surgical Management of Head Trauma for details.
Survivors of head trauma have a high incidence of functional and neuropsychological dysfunction.1,11, 12 and 13
Children who have coma need early comprehensive assessment and care by a multidis-ciplinary rehabilitation team.
PATHOPHYSIOLOGY
Intracranial Compliance Curve
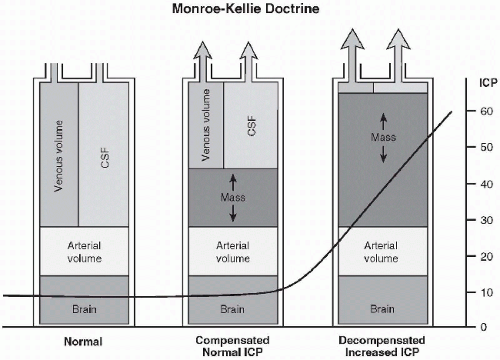
The intracranial vault contains brain matter, blood, and cerebrospinal fluid (CSF) in a closed space.
An expanding mass, such as a hematoma or cerebral contusion, will first displace venous blood and CSF, and intracranial pressure will initially remain stable.
As a mass expands, eventually no space remains and the intracranial pressure (ICP) rises exponentially (Munroe-Kellie doctrine; see Fig. 5-1).
The brain is said to be “tight” when relatively small increases in intracranial volume lead to relatively large increases in intracranial pressure.
Open fontanelles in an infant do not protect the brain from increased ICP.3
Cerebral Blood Flow and Edema
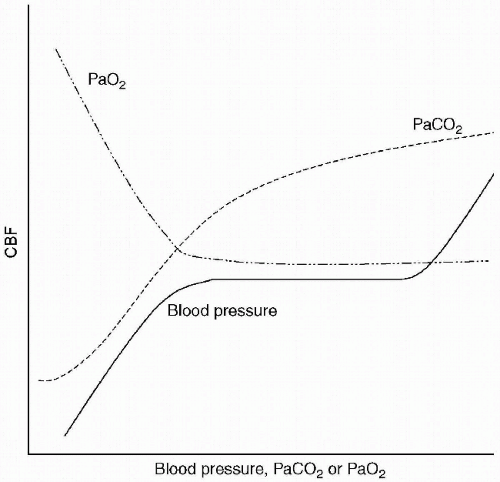
Arterial oxygen tension (PaO2), arterial carbon dioxide tension (PaCO2), and blood pressure have important effects on cerebral blood flow (Fig. 5-2).
High cerebral blood flow may result in intracranial hypertension.
Low cerebral blood flow results in cerebral ischemia.
Cerebral blood flow is relatively constant (autoregulation) over a broad range of blood pressures in healthy viable brain.
Autoregulation is lost in injured brain areas.
These areas are susceptible to further ischemic injury during hypotension.
Infants and young children have a relatively high baseline cerebral blood flow compared to older children and adolescents, which may increase risk of rapid cerebral edema and intracranial hypertension.
Brain edema occurs due to vasogenic (disruption of the blood-brain barrier) and cytotoxic edema.
As PaO2 drops below 60 mmHg, cerebral blood flow rises exponentially.
Therefore keep PaO2 > 80 mmHg or SaO2 > 95%.
Hypercarbia results in cerebral hyperemia but aggressive hyperventilation results in cerebral ischemia.
Maintain PaCO2 35 to 40 mmHg and monitor end-tidal CO2 continuously.
Areas that are injured may lose autoregulation.
Measure blood pressure and maintain blood pressure in the high normal range for age.
Cerebral Metabolic Rate
Cerebral metabolic rate will be increased by fever, seizures, pain, and agitation, which may lead to increased cell death, hyperemia, and intracranial hypertension.
There is a massive inflammatory response following head trauma. Fever develops in the majority of children and adolescents within hours of the injury.14,15
Maintain normothermia, give prophylactic anticonvulsants, and maintain deep sedation and analgesia after ensuring a secure airway.
Brain Cell Death
Brain cell death occurs in contusions and in areas of shear injury.
Contusions are often seen in a “coup and contre-coup” distribution.
Many viable cells are selectively vulnerable to subtle insults such as hypoxia and hypotension.
Great care must be taken to rapidly recognize and treat hypoxia, shock, and hypotension.
DEFINITION/RISK FACTORS
Severe traumatic brain injury is defined as those children with a Glasgow Coma Score (GCS) of ≤8 following head trauma.
Patients with a GCS of 3 to 4, cardiac arrest, or severe hypotension, shock, or hypoxia have a worse prognosis.
INITIAL MANAGEMENT
Indications to perform early intubations:
Upper airway obstruction from:
Actual or potential loss of pharyngeal muscle tone.
Inability to clear oral secretions or vomit.
Seizures.
Foreign body.
Coma or decreasing level of consciousness with a GCS ≤ 8 or deteriorating GCS.
Loss of protective airway reflexes such as cough and gag.
Respiratory arrest, failure, or depression; hypoxia: inability to maintain PaO2 > 60 mmHg or SaO2 > 93% despite supplemental oxygen; respiratory acidosis.
To facilitate hyperventilation if severe increased ICP is suspected (rapidly deteriorating GCS or herniation syndrome).
Seizures or status epilepticus.
Decompensated shock.
ABC MANAGEMENT