Nerve supply of the hand and forearm.
The brachial plexus arises from the ventral rami of C5–T1 and provides muscular and cutaneous innervation. Distal upper extremity innervation is derived from all five nerve roots of the brachial plexus [1]. In addition to the nerve supply to the hand, it is also imperative to consider the need for analgesia of the upper arm if a tourniquet will be used [2].
Interscalene nerve block (ISB):
Indications. Operative procedures involving shoulder, distal 2/3 of clavicle and proximal 1/3 of humerus.
Suitability: ISB is not recommended for hand surgery as the C8–T1 nerve roots, or inferior trunk, are often spared resulting in inadequate blockade of the medial hand.
Disadvantages. Even with the use of US-guided techniques targeting each individual nerve root, complete surgical blockade of the hand and forearm is only achievable in 40% of patients [3–4].
Complications. Phrenic nerve blockade with diaphragmatic paralysis, recurrent laryngeal nerve blockade, and Horner’s syndrome secondary to blockade of the sympathetic cervical chain [5].
Supraclavicular nerve block (SCB):
Indications. Operative procedures involving any part of the upper limb.
Suitability. SCB provides consistently reliable anesthesia of the upper limb [6]. Patients undergoing hand surgery, however, may be dissatisfied with numbness affecting the entire upper limb.
Disadvantages. It is necessary to localize the lower truck, as otherwise ulnar sparing may occur [7].
Complications. Similar to ISB but with increased incidence of pneumothorax and decreased incidence of phrenic nerve blockade.
Infraclavicular nerve block (ICB):
Indications. Operative procedures involving the distal upper arm, elbow, forearm, and hand.
Suitability. Equally safe and effective and requiring less time to perform than a multi-injection axillary block [8], ICB has experienced renewed popularity in the age of US guidance. Compared with targeting each cord, a single injection provides rapid and reliable anesthesia when the needle is positioned superficial to the posterior cord with local anesthetic spread around the artery to the medial and lateral cords [9–10]. Additionally, ICB provides coverage of the musculocutaneous nerve, allowing an upper arm tourniquet to be tolerated.
Disadvantages. ICB is a deeper block and needle visualization can be challenging.
Complications. Minimal risk of pneumothorax or phrenic nerve paresis.
Axillary nerve block (ANB):
Indications. Forearm and hand surgery.
Suitability. ANB has been popular for many years due to its accessible location with a perivascular injection, paresthesia, neurostimulation, or US-based approach and low risk of serious complications.
Disadvantages. Single-injection ANBs are not as reliable as single-injection ICBs; however, multi-injection ANBs have similar success rates (85–92%) [11–12]. Blockade of the musculocutaneous nerve in the fascial plane between biceps and coracobrachialis is required [13]. The intercostobrachial nerve, which arises from the ventral ramus of T2, can be blocked by infiltration of a subcutaneous injection in the axillary fossa for upper arm surgeries.
Complications. Hematoma and vascular puncture are more common than with other techniques.
2. Expand on the incidence of phrenic nerve paralysis following different regional anesthetic block locations
The phrenic nerve originates from C3–C5, travels across the anterior scalene muscle and passes in front of the subclavian artery to enter the thorax. It supplies motor and sensory innervation to the diaphragm with sensory supply to the mediastinal pleura and pericardium [14]. Ultrasound assessment demonstrates a mean distance of 0.18 cm between the plexus and the phrenic nerve at the level of C5–C6, increasing to 1.08 cm at the level of C7–T1 [15].
The incidence of phrenic nerve blockade is dependent on both the proximity of needle insertion in relation to the phrenic nerve and the volume and concentration of local anesthetic that is used for the nerve block [16–17].
Interscalene nerve block, when using a traditional nerve stimulation approach, almost universally results in phrenic nerve involvement (Figure 32.2) [18]. Unilateral diaphragmatic paralysis results in a reduction in functional vital capacity (FVC) of up to 25% in healthy patients [19]. While some studies have demonstrated a reduction in the incidence of phrenic nerve paralysis with US techniques by using a reduced volume of local anesthetic or applying pressure proximal to the injection site, these techniques are not consistent [17, 20–21]. It should be assumed that an ISB using ≥20 ml of volume will result in ipsilateral phrenic nerve paralysis [22].
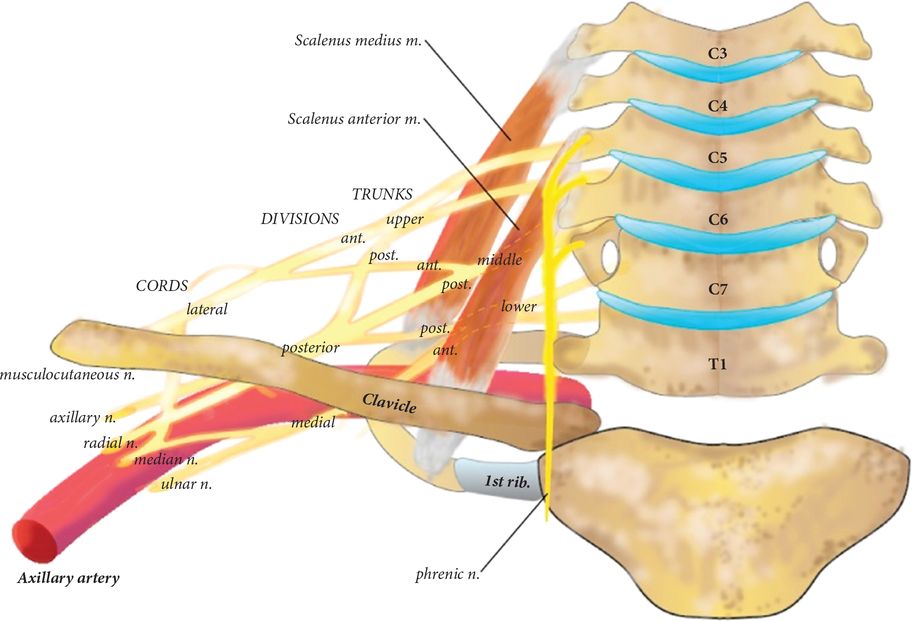
Location of the phrenic nerve in relation to the brachial plexus.
In the majority of patients, the resulting hemidiaphragmatic paresis causes little or no noticeable effect due to compensation by the intercostal muscles [23]. In patients with significant respiratory disease, the reduction in FVC may cause respiratory impairment [24].
While SCB is less likely to induce diaphragmatic paralysis, reported rates reach 50 to 67% [25–26]. In obese patients, severe respiratory compromise after SCB has been described [27–28]. This is most likely due to a further reduction in lung capacity in patients where baseline FRC already approaches residual volume. Consequently, bilateral ISB or SCB are contraindicated. If phrenic nerve paralysis is a concern, consider ICB or ANB [29].
While phrenic nerve paralysis usually resolves, permanent phrenic nerve damage after ISB for shoulder surgery is a recognized complication [18, 30]. In one study, all of the patients who had prolonged neurological dysfunction were male and had a body mass index >25 kg/m2. There likely are multifactorial reasons for the increased incidence in this group, including a significant element of intraoperative surgical trauma [31].
3. Describe the use of distal nerve blockade in this case
With increased utilization of regional anesthesia and US-guided techniques, the use of distal nerve blockade has declined. These techniques remain useful, however, when either more proximal nerve blockade is not feasible, bilateral surgical procedures are required, or to supplement an incomplete brachial plexus block [32]. While distal nerve blockade avoids the complications of phrenic nerve paralysis, pneumothorax, and major vessel injury associated with more proximal approaches, it requires multiple injections.
Median nerve block: The median nerve is effectively blocked at the mid-distal volar aspect of the forearm due to its distance from the brachial artery and its position between flexor digitorum superficialis and flexor digitorum profundus [33]. It appears as a hypoechoic structure in comparison to the surrounding hyperechoic tendons [34]. It may also be blocked medial to the brachial artery in the antecubital fossa.
Radial nerve block: The radial nerve bifurcates just distal to the antecubital fossa to form superficial and deep branches; therefore nerve blockade should occur proximal to this separation [35]. It is located by first visualizing the brachial artery in the mid-upper arm. The radial nerve is found lateral to the artery and may be seen crossing the humerus in the spiral groove.
Ulnar nerve block: The ulnar nerve descends posteromedially to the humerus and passes through the cubital tunnel between the olecranon and the medial epicondyle to enter the forearm medial to the ulnar artery. Nerve blockade may be performed in the mid-upper forearm by tracing the nerve as it runs from the cubital tunnel until it begins to move more medial to the artery. Injection at this site is more successful because the sensory branches divide approximately 5 cm above the wrist [36].
The ulnar nerve may also be visualized proximal to the cubital tunnel. Blockade should not occur in the cubital tunnel as this may cause increased pressure and potential nerve damage. Approximately 5 to 7 ml of local anesthetic solution should be injected around each nerve in order to provide adequate anesthesia [37].
4. Discuss sedation options given the patient’s history if a regional anesthetic is utilized
OSA is an increasingly common condition thought to affect ≥20% of the US population [38]. Characterized by obstructive episodes, daytime somnolence, and snoring, treatment consists of continuous positive airway pressure (CPAP) devices and lifestyle modification [39]. Obstructive sleep apnea has been recognized as an independent risk factor for complications after anesthesia including postoperative hypoxemia, ICU admission, and prolonged hospital stay [40]. Practice guidelines for patients with OSA include use of peripheral nerve blockade with or without moderate sedation for superficial procedures [41].
Sedation is commonly employed for procedures performed under peripheral nerve blockade to improve patient comfort and reduce anxiety. Benzodiazepines, opioids, and propofol are the most frequently utilized agents. While these medications, used individually or in combination, can provide safe and appropriate levels of sedation in patients with OSA, studies have shown that they also may lead to significant airway compromise and hypoxemia [42–43]. Dexmedetomidine has been used successfully for sedation in patients with severe OSA, as patients maintain spontaneous ventilation with minimal respiratory impairment and are easily arousable [44–45]. Regardless of the sedation modality chosen, standard ASA monitors including end-tidal CO2, supplemental oxygen, and occasionally non-invasive ventilation may be employed to reduce the potential for serious complications [41]. Each case must be assessed on an individual basis in order to determine whether it may proceed as an outpatient procedure.
References

Full access? Get Clinical Tree




