Fig. 22.1
Common sites of ectopic pregnancy
Symptoms and Signs
The triad of amenorrhea, vaginal bleeding, and lower abdominal pain in sexually active women should raise the suspicion for an ectopic pregnancy.
Clinical exam should include a bimanual pelvic examination that may reveal unilateral lower pelvic tenderness and an adnexal mass (depending on how advanced the pregnancy is).
Initial screening should include a rapid urine pregnancy test, but a quantitative serum human chorionic gonadotropin (hCG) is needed for confirmation.
Pelvic or transvaginal ultrasound is typically warranted and may reveal a gestational sac within the uterus or in the adnexa (occasionally even an embryo).
If an intra- or extrauterine pregnancy is not seen with a highly suspicious clinical presentation and an hCG level of 1500 mIU/ml or less, the hCG should be repeated in 24–48 h.
In a normal pregnancy, these levels typically double every 48 h, as opposed to ectopic pregnancies, where the rise is typically subtler.
If not, an absolute hCG level may not differentiate between a uterine versus an ectopic pregnancy. Rather, a trend should be followed over time.
Management
The gold standard is exploration, with most experienced surgeons favoring the laparoscopic approach, unless the patient is in extremis.
If the patient is in shock or if the abdomen is distended with blood, emergent laparotomy is preferred.
The goal of exploration is to remove the ectopic gestation while preserving reproductive function.
If the fallopian tube appears mildly affected, salpingotomy (Fig. 22.2) – in which the gestational sac is removed through an incision in its anti-ligamental aspect – might be possible
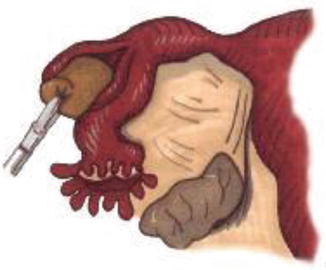
Fig. 22.2
Salpingotomy with retrieval of ectopic pregnancy
If the tube is more extensively damaged, complete salpingectomy may be necessary.
Carefully selected hemodynamically stable and reliable patients with pregnancies <3 cm, absence of embryonic cardiac activity, and serum hCG levels of <10,000 mIU/ml may also be considered for medical management.
Several regimens based on the cytotoxicity of methotrexate on the developing embryo have been proposed.
Consultation with an obstetrician gynecologist for follow-up is advisable.
Expectant management of a documented ectopic pregnancy may also be an option in physiologically stable patients with minimal pain and with hCG levels <1000 mIU/ml and declining.
Patients must be counseled regarding the risks of rupture and hemorrhage, and emergency management must be readily available.
Serial serum hCG levels should be trended for appropriate decreases postoperatively or with medical management or observation.
Should at any point the pregnant female deteriorate clinically or become hemodynamically unstable, a trip to the operating room is warranted.
22.2 Ovarian Torsion
Definition: torsion of the fallopian tube and ovary around the infundibulopelvic ligament compromising vascular supply to the torsed organ represents a surgical emergency that, if left untreated, may lead to ovarian infarction and diffuse peritonitis with significant morbidity.
Causes: abnormal enlargement of the adnexa by neoplasms or more frequently by cysts.
More commonly encountered in females in their early reproductive years but may also occur after menopause.
Symptoms and Signs
Usual presentation:
Typically, severe unilateral lower quadrant pain of acute onset, frequently associated with nausea and vomiting
Initially
After episodes of milder localized pain, corresponding to partial twisting and spontaneous detorsion
Clinical exam: unilateral lower quadrant tenderness and rigidity (may be mistaken for acute appendicitis when it involves the right adnexa)
Laboratory markers
Elevated CRP
Ultrasonography
Typically demonstrates a mass in the affected region
However, arterial flow may or may not be noted even in the presence of torsion.
CT: mass in the affected quadrant with benign characteristics, with the uterus typically deviating towards the affected adnexa.
Management
Emergency surgical intervention is warranted in all females with confirmed or suspected ovarian torsion.
Unless infarction has led to disseminated peritonitis and hemodynamic instability, this can be undertaken safely with laparoscopy.
Principles of management:
Untwist the torsed adnexum
Assess viability
If viability is satisfactory, some advocate securing the ovary onto the psoas (to minimize recurrence).
If there is no evidence of reperfusion or if infarction has occurred, oophorectomy.
Similarly, a gangrenous adnexum must be completely removed.
Ideally, removal of the cause of the torsion (cyst resection – if present) should be done at the time of the initial procedure.
However, cystectomy or partial oophorectomy may be very challenging in an inflamed and fragile ovary.
In such cases, it may be best to reevaluate the patient in 6–8 weeks, and if the ovarian mass is persistent, schedule elective laparoscopic cystectomy.
22.3 Infections Requiring Surgical Intervention
22.3.1 Pelvic Inflammatory Disease (PID)
Defined as any infectious process of the upper female genital tract caused by upward migration of pathogenic microorganisms, most commonly Neisseria gonorrhea and Chlamydia trachomatis or less commonly Mycoplasma, Ureaplasma, or anaerobes from the lower urogenital tract.
Is not a single disease entity, but rather represents a spectrum of infectious processes involving the uterus, fallopian tubes, and ovaries, resulting in endometritis, salpingitis, and oophoritis; it may also involve adjacent pelvic organs resulting in peritonitis, tubo-ovarian abscesses (TOA), and less frequently perihepatitis (Fitz-Hugh-Curtis syndrome).
Prompt diagnosis and treatment is of paramount importance in order to preserve fertility and avoid complications associated with PID, such as infertility, ectopic pregnancy, and chronic pelvic pain.
Patients are usually young, have a long sexual history typically with multiple sex partners, and lack of use of barrier contraceptives.
Approximately 780,000 new cases of PID are diagnosed annually in the United States, but more likely many go unrecognized and untreated.
Symptoms and Signs
Diagnosis can be challenging due to a wide range of presentations.
Common symptoms include fever, nausea and vomiting, lower abdominal pain, and purulent vaginal discharge.
Differential diagnosis includes appendicitis, inflammatory bowel disease, urinary tract infections, ectopic pregnancy, and ovarian torsion.
Presence of cervical motion tenderness and uterine or adnexal tenderness should raise suspicion, while laparoscopy with directed biopsies remains the golden standard for definitive diagnosis.
Positive laboratory findings include presence of white blood cells on cervical wet prep, elevated sedimentation rate and C-reactive protein, or positive serological testing for gonorrhea and/or chlamydia.
Transvaginal ultrasonography and computed tomography typically reveal thickened, fluid-filled fallopian tubes with or without free pelvic fluid and/or organized infected fluid collections.
Management
Medical: the Centers for Disease Control and Prevention recommend one of the following regimens:
Outpatient treatment options
Ceftriaxone plus doxycycline (in the absence of pregnancy) with or without metronidazole, usually for 14 days
Cefoxitin with probenecid plus doxycycline with or without metronidazole, usually for 14 days
Newer-generation fluoroquinolone with or without metronidazole for 14 days
Inpatient treatment options
Cefotetan every 12 h or cefoxitin every 6 h, plus doxycycline every 12 h or clindamycin every 8 h plus gentamicin every 8 h or ampicillin/sulbactam every 6 h plus doxycycline every 12 h.
After at least 24 h of intravenous antibiotics, oral antibiotics (doxycycline or clindamycin) continued at home after discharge from the hospital. Total treatment with medicine usually lasts for 14 days.
Surgery
May be required for TOA (30 % of all patients hospitalized for PID)
Suspected in the presence of lateralized lower abdominal pain that may mimic acute appendicitis and is typically identified in women with recurrent episodes of inadequately treated PID and chronically persistent symptomatology.
Bimanual clinical examination: tender adnexal mass may be palpated.
Pelvic or transvaginal ultrasound is typically confirmatory, as is computed tomography.
If no response to trial of oral or intravenous antibiotics (third-generation cephalosporins plus doxycycline with or without metronidazole for 14 days) within 48–72 h, percutaneous or surgical drainage of the abscess is mandated.
May be necessary for ruptured abscesses
High mortality rate if not recognized and managed promptly.
Full access? Get Clinical Tree







