Gynecologic
11-1 Bartholin Gland Abscess
Anthony Morocco
Clinical Presentation
A Bartholin gland cyst manifests as a painless mass (1 to 3 cm) in the labia. Abscesses are larger (up to 8 cm or more), are more painful, and develop over 2 to 4 days. Patients complain of severe vulvar pain, dyspareunia, and difficulty sitting or walking. The abscess may spontaneously rupture and drain after several days.1
Pathophysiology
The Bartholin glands are paired structures located in the labia minora. Cysts or abscesses of these glands occur in 2% of women.1 The glands are normally pea-sized and located at the 4- and 8-o’clock positions. They drain through ducts that exit between the hymenal ring and the labium. A Bartholin gland cyst results when the duct is blocked. An abscess occurs due to infection of a cyst.1 The organisms most commonly found in these abscesses are Bacteroides fragilis and Peptostreptococcus spp. Neisseria gonorrhoeae is found in 10% to 15% of cases.2
Diagnosis
Differential diagnosis includes several types of cyst (e.g., sebaceous), hematoma, carcinoma, fibroma, lipoma, endometriosis, and inguinal hernia.1
Clinical Complications
Potential complications of the abscess or drainage procedure include dyspareunia, excessive bleeding, cellulitis, and sepsis.1
Management
In patients younger than 40 years of age, asymptomatic Bartholin gland cysts require only treatment for discomfort or cosmesis. Older patients should have the cyst removed and tested to rule out carcinoma. Ruptured cysts and abscesses should be treated with sitz baths. Early abscesses may also benefit from sitz baths, because drainage may be more successful if it is delayed until the abscess is “pointing.” Simple lancing or needle aspiration of a cyst or abscess commonly results in recurrence of the lesion.1 Appropriate emergency treatment involves drainage and placement of a drainage catheter. After local anesthesia, an incision is made into the abscess through the mucosal side (inside the labium). After the pus has been drained and any loculations broken up, the catheter is placed in the abscess cavity and its balloon is filled with water. The catheter should remain in place for 4 to 6 weeks to allow formation of a permanent fistula. The patient should be tested for gonorrhea and chlamydia.2 Definitive treatment of recurrent Bartholin cyst or abscess by a gynecologist includes marsupialization, laser excision, or surgical excision.1
REFERENCES
1. Hill DA, Lense JJ. Office management of Bartholin gland cysts and abscesses. Am Fam Physician 1998;57:1611-1616, 1619-1620.
2. Zeger W, Holt K. Gynecologic infections. Emerg Med Clin North Am 2003;21:631-648.
11-2 Bacterial Vaginosis
Anthony Morocco
Clinical Presentation
Pathophysiology
BV is a common form of infectious vaginitis, with an incidence of 10% to 40%.1 Despite its common occurrence, the precise cause remains unclear. The importance of sexual transmission is unknown, but BV is associated with multiple sex partners and frequent douching.2 BV is most likely a polymicrobial anaerobic infection, with concurrent inhibition of the Lactobacillus organisms that normally inhabit the vagina. Gardnerella vaginalis, a gram-negative rod, plays a prominent role in BV, along with other anaerobes such as Bacteroides, Peptococcus, Prevotella, and Mycoplasma hominis.2,3 G. vaginalis may also be part of the normal vaginal flora; men may harbor the organism in the urethra, but they do not develop symptoms.3
Diagnosis
The diagnosis is based on identification of three of the following four clinical criteria on examination of vaginal fluid: presence of clue cells (desquamated epithelial cells with adherent bacteria); pH greater than 4.5; positive “whiff test” (presence of amine odor with potassium hydroxide); and a thin, adherent vaginal discharge. Gram staining, DNA probes, and other commercial assays may assist in diagnosis.1 Differential diagnosis includes infections such as Trichomonas, Candida, and Chlamydia and the presence of a vaginal foreign body.3
Clinical Complications
Management
All symptomatic patients should be treated, as should asymptomatic pregnant patients.2 Recommended antibiotic regimens for nonpregnant women include oral metronidazole 500 mg or intravaginal metronidazole gel. Less efficacious regimens include oral or intravaginal clindamycin and single-dose metronidazole therapy. Pregnant women should be treated with metronidazole or clindamycin. Treatment during pregnancy reduces the risk of obstetric complications.1,2,3 Treatment of sex partners is not recommended.2 Clinicians should consult current recommendations from the Centers for Disease Control and Prevention for doses and applicable duration of therapy.
REFERENCES
1. Zeger W, Holt K. Gynecologic infections. Emerg Med Clin North Am 2003;21:631-648.
2. Workowski KA, Levine WC. Sexually transmitted diseases treatment guidelines—2002. MMWR Morb Mortal Wkly Rep 2002;51(RR-6):1-80.
3. Fiumara NJ. Genital ulcer infections in the female patient and the vaginitides. Dermatol Clin 1997;15:233-245.
11-3 Vulvovaginal Candidiasis
Anthony Morocco
Clinical Presentation
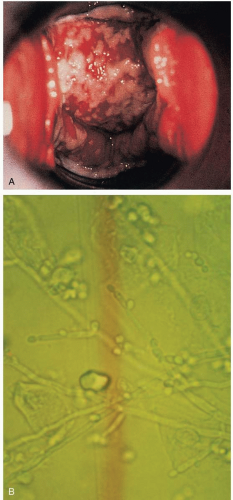
Patients with vulvovaginal candidiasis (VVC) present with pruritus; a white, curd-like vaginal discharge; erythema of the vulva; vaginal pain; dyspareunia; and dysuria.1
Pathophysiology
VVC, also called monilial vaginitis, is a common infection of the female genital tract, affecting 75% of women at least once. Recurrent VVC is defined as four or more episodes per year.1 VVC is most commonly caused by Candida albicans. Recurrent VVC is more likely to be caused by Candida glabrata or other non-albicans species (10% to 20% of cases).1 Risk factors for infection include antibiotic use, pregnancy, immunocompromised state, diabetes, corticosteroids, and higher-dose estrogencontaining oral contraceptives.2
Diagnosis
Yeasts and pseudohyphae may be visualized on a saline preparation of vaginal fluid with 10% potassium hydroxide (KOH) added. Candida can also be cultured from vaginal fluid; however, this organism is part of the normal vaginal flora in 10% to 20% of women who are asymptomatic.1
Clinical Complications
Patients with severe infections may develop extensive areas of erythema, edema, excoriation, satellite lesions, and formation of fissures.1
Management
The topical azoles (e.g., clotrimazole, miconazole), used intravaginally, are 80% to 90% effective in relieving symptoms and eradicating the pathogen. Oral fluconazole is also effective. Longer courses of treatment may be needed for recurrent VVC, non-albicans infections, and severe cases. Recurrent VVC may also require long-term suppressive maintenance therapy. Treatment of sex partners is not generally recommended except in cases of recurrent infection or balanitis.1
REFERENCES
1. Workowski KA, Levine WC. Sexually transmitted diseases treatment guidelines—2002. MMWR Morb Mortal Wkly Rep 2002;51(RR-6):1-80.
2. Sobel JD, Faro S, Froce RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol 1998;178:203-211.
11-4 Uterine Prolapse
Anthony Morocco
Clinical Presentation
Patients with uterine prolapse may present with complaints of pelvic pressure, low back pain, dyspareunia, or a mass in the vagina. Symptoms and degree of prolapse worsen with increases in intraabdominal pressure.1

Full access? Get Clinical Tree