GENITOURINARY INJURIES
CASE SCENARIO
A 22-year-old man presents to the emergency room after being involved in a motor vehicle accident in which his car was struck from the side. In the emergency room he is noted to be tachycardic, with a heart rate (HR) of 135, and hypotensive, with blood pressure (BP) 90/60. On physical examination he is noted to be diaphoretic, with right flank pain, costovertebral angle tenderness, and significant flank ecchymosis. His initial laboratory studies are notable for a HCT of 30. Two large-bore IVs and a Foley catheter are placed without difficulty, and the Foley drains bright red blood. His urinalysis shows >100 red blood cells (RBCs)/hpf.
EPIDEMIOLOGY
Diagnosis of injuries to the genitourinary system requires a high index of suspicion, and can be missed in the setting of distracting injuries. This chapter includes a systematic discussion of the presentation and management of trauma to all components of the genitourinary system, with an emphasis on radiological recognition to avoid dangerous delays in diagnosis.
 Renal Trauma
Renal Trauma
Overall, renal trauma accounts for 3% of all trauma admissions, and comprises 67% of cases of genitourinary (GU) trauma.1 Blunt renal trauma is 9 times more common than penetrating trauma, but is far less likely to be clinically significant (5% vs 64%).1 Renal trauma occurs in up to 10% of blunt injuries to the abdomen, and is often associated with concomitant liver or splenic injury.2
 Ureteral Injury
Ureteral Injury
Ureteral injuries are commonly missed on initial trauma survey, represent only 1% of all GU injuries, and require a high index of suspicion to diagnose. Risk factors for ureteral injury include prior radiation, retroperitoneal fibrosis, and iatrogenic causes such as intraoperative bleeding leading to rapid application of surgical clips or sutures. While 80% of ureteral injuries are iatrogenic, any penetrating injury to the upper or lower quadrants can inflict ureteral injury.3 Blunt trauma, particularly rapid deceleration injuries, can also lead to a ureteropelvic junction disruption or tear of the ureter.
 Bladder Injury
Bladder Injury
Bladder injuries make up 22% of GU trauma, but represent less than 2% of all injuries requiring surgery. Roughly two-thirds of all bladder injuries are blunt, and the remaining are penetrating injuries.4 Bladder injuries are more common in children, in whom the bladder is an abdominal organ unprotected by the bony pelvis.
 Urethral Injury
Urethral Injury
Urethral injuries comprise 3% of all genitourinary trauma, and are most commonly seen in the setting of pelvic fractures. Posterior urethral injuries (prostatic and membranous urethra) are seen in 4% to 14% of pelvic fractures, often with a concurrent bladder injury.5 Anterior urethral injuries (bulbar and pendulous urethra) are less common, comprising 10% of all urethral injuries, and are most commonly seen after straddle injury or gunshot trauma.
 Scrotal Trauma
Scrotal Trauma
Scrotal trauma is rare, accounting for less than 1% of all trauma in the United States; however, it confers significant morbidity. In significant blunt scrotal trauma, testicular rupture occurs with a frequency as high as 50%. Scrotal injuries make up 2% of all civilian gunshot wounds, and associated injuries are common (thigh, femoral vessels, perineum, penis/urethra).
 Trauma to Penis/External Genitalia
Trauma to Penis/External Genitalia
The penis or external genitalia are affected in 7% of all GU traumas. Isolated penile trauma is relatively uncommon, and is generally due to penile fracture. It is less commonly seen with gunshot injuries and amputation.
PATHOPHYSIOLOGY
 Renal Trauma
Renal Trauma
The kidneys sit in the retroperitoneum and are protected by the lower ribs and surrounding organs such as the liver, colon, and spleen. Gerota’s fascia provides an envelope that compartmentalizes and tamponades renal bleeding. While Gerota’s fascia can be torn during injury, bleeding stays retroperitoneal (unless the peritoneum is also perforated), and consequently, hemorrhage may be contained.
 Ureteral Injury
Ureteral Injury
The proximal ureter receives its blood supply medially from the ureteral artery, a branch of the renal artery. The ureteral artery runs longitudinally down the ureter, while perforating arteries from the aorta supply the mid-ureter, and the internal iliac feeds the distal ureter laterally. The blood supply from these arteries is tenuous, however, and the region of the ureter distal to the injury may become devascularized in trauma.
 Bladder Injury
Bladder Injury
Extraperitoneal bladder ruptures are commonly seen in the setting of pelvic fracture (80%).6 It had been previously thought that most extraperitoneal bladder injuries occurred because pelvic bone fragments penetrated the bladder wall. It is now thought, however, that extraperitoneal bladder ruptures more commonly occur due to burst or shearing energy from the force of trauma tearing the bladder from its fascial attachments. Thus, the extraperitoneal bladder rupture usually occurs concurrently with the pelvic fracture, rather than secondary to it.7 The dome of the bladder is its weakest point due to the lack of fascial support, and this is where intraperitoneal bladder ruptures most commonly occur.
 Urethral Injury
Urethral Injury
Urethral distraction injuries often occur in the setting of pelvic fractures (posterior urethra) or straddle injuries (anterior urethra). Pubic diastasis predisposes patients to urethral trauma, and so the initial survey may provide a clue to the presence of these injuries.
CLINICAL PRESENTATION
 Renal Trauma
Renal Trauma
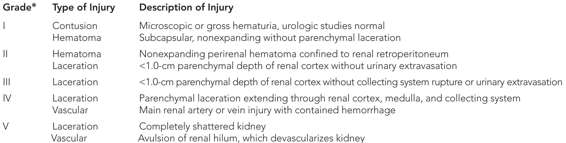
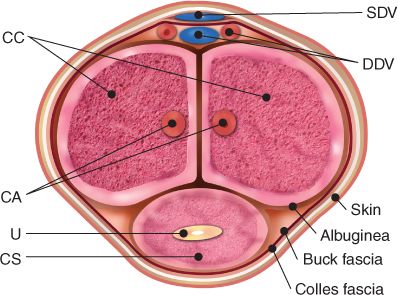
Symptoms and signs associated with renal injury may include flank pain, hematuria (if the injury involves the collecting system), and flank or costovertebral angle hematoma. Patients with high-grade renal injuries frequently present with hemodynamic instability, while patients with lower-grade injuries may be clinically stable. Renal injuries often occur in the setting of polytrauma, especially in association with rib fractures. The grading of renal injuries is detailed in Table 30–1 and Figure 30–1.
*Advance one grade for multiple injuries to the same organ.
Reproduced with permission from Moore, E. E., Shackford, S. R., Pachter, H. L. et al.: Organ injury scaling: spleen, liver, and kidney. J Trauma, 1989;Dec;29(12):1664–1666
Figure 30–1 The American Association for the Surgery of Trauma renal injury scoring system. (Reproduced with permission from Wessells H1, McAninch JW: Effect of colon injury on the management of simultaneous renal trauma, J Urol. 1996 Jun;155(6):1852–1856.)9,10
 Ureteral Injury
Ureteral Injury
Most ureteral injuries are iatrogenic, with 52% to 82% occurring during gynecologic procedures and 9% during low anterior resection or abdominoperineal resection.3 Ureteral injuries are often asymptomatic initially, and in the setting of polytrauma, may be difficult to diagnose clinically. Hematuria is an unreliable indicator in ureteral injuries.8 An undiagnosed ureteral injury can lead to urine leak, ileus, chemical peritonitis, and potentially sepsis. Over time, the injured ureter can stricture, leading to infection or renal failure.
 Bladder Injury
Bladder Injury
Bladder injuries may present with abdominal pain, tenderness, and ecchymosis. Over 95% of major injuries will present with gross hematuria. A bladder injury may also be suspected if a Foley is placed, is in the correct position, and does not return urine. Intravesical bladder ruptures may lead to a chemical peritonitis, while this is not commonly seen in extraperitoneal bladder ruptures.
 Urethral Injury
Urethral Injury
Posterior urethral injuries classically present with blood at the meatus, a high-riding prostate, and perineal hematoma. In practice, however, blood at the meatus may be the only clue. It can be difficult to palpate the true prostate in the setting of pelvic bleeding. Likewise, perineal hematoma is rare. Anterior urethral injuries will present with hematuria, and if a corporal injury occurs, presentation will be comparable to that of a penile fracture.
 Scrotal Trauma
Scrotal Trauma
Patients with injuries to the scrotum and its contents typically present with scrotal or abdominal pain, and occasionally scrotal ecchymosis. Ecchymosis may be due to testicular rupture, injury to the spermatic cord, or tear of one of the scrotal vessels. Testicular torsion is also seen in boys and young men, and can present with scrotal pain followed by nausea and vomiting, with a horizontal lie to the affected testis.
 Trauma to Penis/External Genitalia
Trauma to Penis/External Genitalia
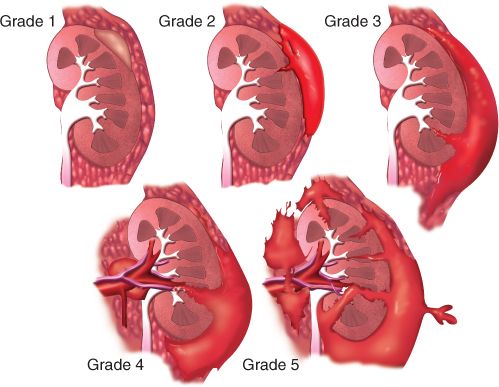
Penile fractures typically present during intercourse with sudden pain and a popping sensation followed by rapid detumescence and ecchymosis. Anterior urethral injury may also occur and has a similar presentation. If the bleeding is contained to Buck’s fascia, the phallus will have an eggplant appearance. If Buck’s fascia is torn, the hematoma may extend to the scrotum and perineum in a butterfly pattern, contained within Colles’ fascia (Figure 30–2).
Figure 30–2 A schematic drawing showing the penis in cross-section. Buck’s fascia and Colles’ fascia can be seen enveloping both the corpora cavernosa (CC) and the corpus spongiosum (CS). Also seen are the superficial dorsal vein (SDV), deep dorsal vein (DDV), cavernosal arteries (CA), and urethra (U). (Reproduced with permission from Bertolotto, M., Serafini, G., Savoca, G. et al.: Color Doppler US of the postoperative penis: anatomy and surgical complications, Radiographics 2005;May-June;25(3):731–748.)1
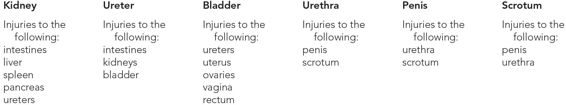
DIFFERENTIAL DIAGNOSIS
See Table 30–2.
WORKUP AND CHOICE OF IMAGING
 Renal Trauma
Renal Trauma
In an adult, indications to obtain imaging for possible renal injuries include the following: penetrating trauma, rapid deceleration injuries with injuries to the spine or ribs, microscopic hematuria (>5 RBCs/hpf) with shock, and gross hematuria. The same is true in pediatric patients except that microscopic hematuria <50 RBCs/hpf does not require imaging.12 The imaging test of choice is a hematuria/triphasic computed tomography (CT) scan that will allow identification of vascular, renal parenchymal, and ureteral injuries. If contrast cannot be given, a non-contrast CT may be performed, but this is inferior in the diagnosis and grading of renal injuries, and cannot detect ureteral injuries. One may safely avoid imaging in the stable adult with microscopic hematuria, as the likelihood of significant injury is low.13
Grade IV and V injuries should be followed up with a contrast CT at 48 hours to determine if the injury has evolved, particularly if there is clinical evidence of expanding hematoma or urinoma. A stable urinoma may be safely observed, as >80% will resolve spontaneously.
If the patient is unstable and it is impossible to obtain a preoperative abdomen/pelvic CT scan before proceeding to the operating room, prior to nephrectomy one may obtain an on-table intravenous pyelogram (IVP) by injecting 2 cc/kg of IV contrast and attaining a plain film at 10 minutes, to assess function of the contralateral kidney. It is essential to ensure a functioning contralateral kidney if a nephrectomy needs to be performed. An on-table IVP is unreliable, however, for assessing ureteral injury, and will miss such injuries in 36% of cases.
 Ureteral Injury
Ureteral Injury
The key to early diagnosis of ureteral injuries is a high index of suspicion, as hematuria may be absent in 25% of cases. A hematuria/triphasic CT is indicated in all stable patients with penetrating injuries to the flank or upper quadrants, or after a rapid deceleration injury. If IV contrast cannot be given, a retrograde pyeloureterogram can be performed, to assess for contrast extravasation and to allow simultaneous stent placement; however, this may not be practical in the acute setting.
 Bladder Injury
Bladder Injury
While a hematuria/triphasic CT is the standard for imaging the upper urinary tract, a CT cystogram or retrograde cystogram is the study of choice for imaging the bladder, as the bladder filling from a hematuria CT is insufficient to identify bladder injuries. A CT cystogram is preferable, and is performed by filling the bladder with 400 cc of contrast. Full bladder and post-drainage CTs are obtained. For a retrograde (fluoroscopic) cystogram, filling the bladder with a minimum of 400 cc of contrast and 4 films (empty, full, partly drained, post-drainage) are commonly obtained to detect bladder perforations.
 Urethral Injury
Urethral Injury
Retrograde urethrography is the imaging test of choice for urethral injuries, whether strictures or tears are suspected. If possible, the patient should be placed in the figure-4 position with one leg flexed at the hip and knee and the thigh externally rotated. A roll or wedge should be placed under the contralateral hip, and the phallus placed pointing toward the flexed hip. A Foley should be placed in the distal urethra so the fossa navicularis can be occluded with 2 cc in the balloon to prevent backflow. The contrast should be diluted to 30% and may be instilled via the Foley in 10-cc increments under fluoroscopy.
A percutaneous or open suprapubic tube should be placed if a Foley cannot be inserted safely. With a suprapubic tube in place in a stable patient, a combined antegrade and retrograde urethrogram can be performed, giving a more accurate assessment of stricture length and urethral alignment, although this may not be feasible in the acute setting.
 Scrotal Trauma
Scrotal Trauma
Doppler ultrasound of the scrotum is the test of choice for all blunt injuries to the scrotum. Performing an ultrasound for penetrating scrotal injuries prior to surgical exploration is not essential, but preoperative CT may be helpful in identifying foreign bodies such as bullet fragments or shrapnel within the scrotum, as intraoperative location can be difficult. In addition, the location of a foreign body may change over time, so a recent CT may be useful if surgery is delayed.
 Trauma to Penis/External Genitalia
Trauma to Penis/External Genitalia
Penile fracture is a surgical emergency, and imaging should not delay surgical intervention unless the diagnosis is in question. A penile ultrasound with Doppler or magnetic resonance imaging (MRI) may aid if the diagnosis is in doubt. A retrograde urethrogram or cystoscopy performed in the operating room (OR) is important to rule out urethral injury, as this occurs in 16% of patients.14
IMAGING FINDINGS
 Renal Trauma
Renal Trauma
Signs of renal injury on CT include a perinephric hematoma, renal laceration, and extravasation of contrast from the renal parenchyma or the renal pelvis (Table 30–3 and Figures 30–3 through 30–6).