Roya Saffary
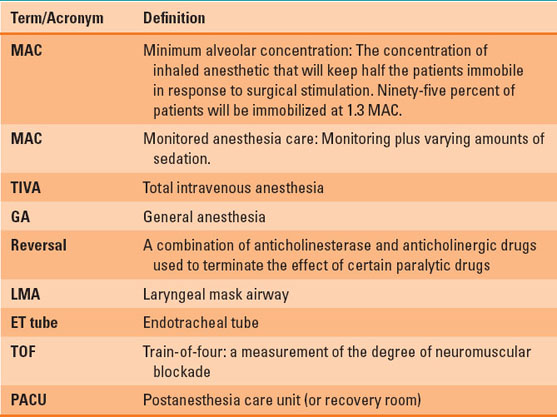
The operating room is a complex environment full of bright lights, sharp instruments, and elaborate equipment, with people speaking a strange language (Table 19-1). Modern surgery can remove, repair, or even replace almost every body part. Anesthesia makes these interventions possible, but anesthesia itself can be complicated and overwhelming. This chapter follows a “typical” patient through the planning and conducting of a general anesthetic, highlighting many of the decisions involved. This chapter’s purpose is to demystify anesthetic care and provide a basic understanding of the steps involved in planning and conducting a safe procedure.
 VIDEO 19-1
VIDEO 19-1
General Anesthesia: An Example
I. Purpose/Goals of an Anesthetic
A. What Is Anesthesia?
General anesthesia is a process whereby the patient is rendered unconscious in a reversible, controlled manner. Anesthetics induce unconsciousness by binding to specific receptors throughout the brain, brainstem, and spinal cord. Emerging evidence suggests that anesthetics interrupt the neural networks that underlie consciousness. General anesthetics also produce immobility. Although anesthetics most likely make patients unconscious by acting on the brain, immobility appears to result from effects on the brainstem.
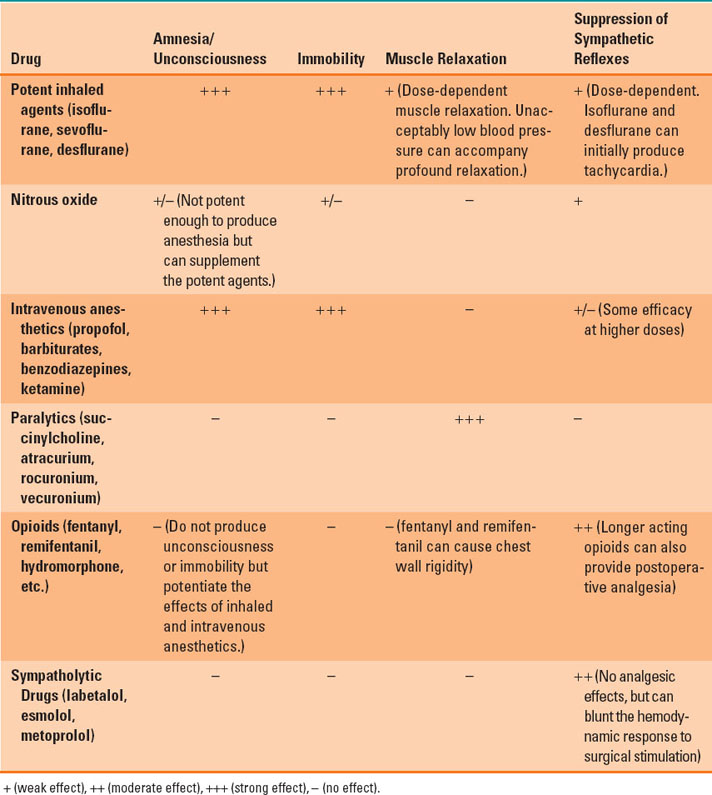
Some operations require skeletal muscle relaxation. Complete muscle paralysis can produce immobility in response to surgical stimulation, although paralysis without unconsciousness can lead to awareness with recall, an uncommon but potentially horrifying complication. In addition, muscle relaxation provides optimal conditions for endotracheal intubation and improves surgical exposure during intra-abdominal and intrathoracic procedures. Although a patient may not move, the body can mount a robust sympathetic response to surgical stimulation with hypertension, tachycardia, and tachypnea. The last element of general anesthesia aims at controlling these changes. Some drugs provide all of the elements of anesthesia, while others have more specific roles. Table 19-2 shows the actions of some commonly used anesthetic drugs.

Anesthetics most likely produce unconsciousness by acting on the brain. However, immobility appears to result from their effects on the brainstem.
Table 19-1 Common Anesthesia-Related Terms and Acronyms
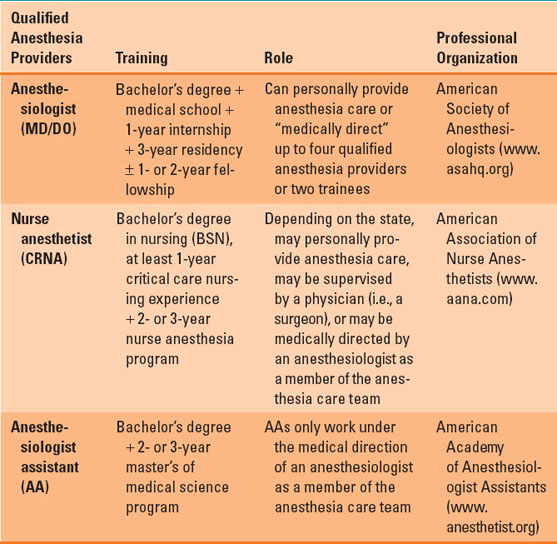
B. Who Gives Anesthesia?
There are a variety of medical professionals who will be encountered on an anesthesia rotation (Table 19-3). These people are known as qualified anesthesia care providers. They have different backgrounds and training and may work alone or as part of an anesthesia care team.
C. What Are the Risks of Anesthesia?
Most anesthesia consent forms include a list of possible complications. Some of these, such as sore throat and postoperative nausea or vomiting, are common but transient. Others, such as dental damage or corneal abrasion, are less common but self-limited or repairable. A few, including awareness, brain damage, or death, are rare but catastrophic. About 1 in 10,000 patients will have awareness during anesthesia. Patients with a previous episode of awareness with recall are at increased risk of this complication after a subsequent anesthetic (1). Death solely due to anesthesia is very rare, occurring in fewer than 1 in 100,000 anesthetics.

Awareness during anesthesia is rare, occurring in about 1 in 10,000 cases.
II. Preoperative Evaluation
A. Patient Assessment
Surgery stresses the body, and anesthetics have significant physiologic effects. Therefore, before giving any anesthetic, the anesthesiologist evaluates the patient, looking for problems that might increase risk. This assessment requires knowledge of the patient’s past and current medical and surgical conditions. The preoperative evaluation may be completed in person by the anesthesiologist, by a nurse in a preoperative clinic or via a phone interview, or by the patient via a web-based questionnaire. In many centers, healthy patients presenting for outpatient surgery and any patient needing emergency surgery may be evaluated on the day of the operation.
Table 19-2 Actions of Commonly Used Anesthetic Drugs
The preanesthetic evaluation begins with the chief complaint. In this case, what surgery is needed and why. Although this information should be available in the medical record, confirming the site and side of surgery directly with the patient is an important safeguard against wrong-site, wrong-side surgery. Next the patient’s age, height, and weight are reviewed. Extremes in any of these values can present unique concerns (see Chapters 28 and 33). Reviewing the patient’s surgical history can alert the anesthesiologist to significant medical problems. Questions about previous anesthetics can help prepare for a difficult airway, postoperative nausea and vomiting, and other possible complications. Even if a patient has never had anesthesia, the family history might reveal malignant hyperthermia, pseudo-cholinesterase deficiency, or other heritable problems. The anesthesiologist also checks the patient’s medications and allergies and asks targeted questions about the patient’s medical problems and systems review.
Table 19-3 Who’s Who in the Operating Room
On the day of surgery, the anesthesiologist reviews the patient’s history and conducts a focused physical examination with emphasis on the heart, lungs, airway, and, if regional anesthesia is planned, the site of the regional anesthetic. Most patients need only this focused history and physical examination before undergoing anesthesia. Some, because of coexisting diseases, and others, because of the proposed surgery, will need additional evaluation.
B. Anesthetic Plan
Anesthesia is often viewed as “putting the patients to sleep.” However, there are multiple ways to provide an anesthetic. Choosing the best approach requires an understanding of each patient, his or her medical history, and the proposed procedure. Ideally, an anesthetic should produce the minimum physiologic trespass, optimal surgical conditions, and a comfortable and expeditious recovery.

The duration of required fasting (NPO) before an anesthetic depends on the type of food or liquid ingested. For clear liquids, it is as short as 2 hours, but for fatty foods, it is at least 8 hours.
C. Nil Per Os Status
General anesthesia and sedation place patients at risk for regurgitation and aspiration of gastric contents. This complication can produce problems ranging from mild chemical pneumonitis and pneumonia to death (see Chapter 40). To minimize this risk, a patient should fast before an elective anesthetic. The duration of fasting (nil per os [NPO]) depends on the type of food or liquid ingested (Table 19-4). Despite these NPO guidelines, patients may take oral medications with a sip of water on the day of surgery (see Chapter 16).
Table 19-4 Duration of Preoperative Fasting
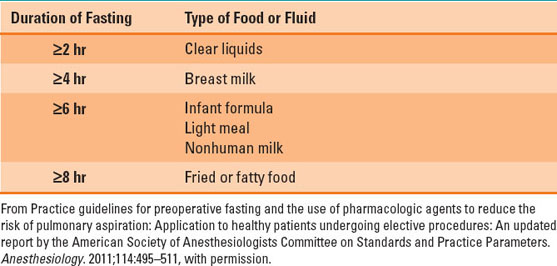
There are exceptions to these rules. Emergency surgeries must begin regardless of the duration of fasting. Trauma patients, those in severe pain, and those with nausea and vomiting or intestinal obstruction may have full stomachs regardless of how long they have been NPO. For these patients, the anesthesiologist may choose a “rapid sequence” induction to quickly secure the airway and minimize the risk of aspiration. Also, due to the physiologic changes of pregnancy, parturients are treated as having a full stomach regardless of their last food or liquid intake (see Chapter 31).
D. Informed Consent
The last step in the preoperative evaluation is obtaining informed consent, which should be targeted to the patient’s specific risks and concerns. Disclose pertinent risks and allow the patient to ask questions. In some cases (i.e., minors), a legal guardian or medical proxy will give consent. Regardless, it is important for the patient to understand and agree with the anesthetic plan. Rarely, in a life-threatening emergency, anesthesia and surgery may proceed without informed consent.
E. Premedication
Many patients are anxious when they are getting ready to have surgery. A thorough preoperative consultation with an anesthesiologist is the best way to relieve a patient’s anxiety (2). In addition, patients sometimes receive a small dose of intravenous benzodiazepine (i.e., midazolam) for additional anxiolysis before entering the operating room. Midazolam should be used carefully. Oversedated patients may not cooperate with moving and positioning in the operating room. In outpatient settings, even small doses of midazolam can delay discharge. The elderly are especially sensitive to its sedating effects.
III. Intraoperative Management
Although complications can occur at any time during an anesthetic, induction and emergence are especially fraught. During induction, the anesthesiologist administers drugs that render the patient unconscious and have significant cardiac and respiratory effects. Anesthetics can lower the patient’s blood pressure by dilating arteries and (mostly) veins, depressing cardiac function, or both. Unconscious patients have diminished upper airway muscle tone, which can obstruct breathing. Many anesthetics act at the brainstem to decrease respiratory drive. Paralytic agents directly affect respiratory muscles. The anesthesiologist gauges and mitigates these effects with careful monitoring and appropriate interventions.
A. Monitoring
Because most anesthetics depress cardiorespiratory function and surgery can increase heart rate and blood pressure, anesthesiologists use both noninvasive and invasive methods to monitor the patient. The most important of these monitors are looking at the patient to help assess oxygenation and perfusion, listening to breath sounds to detect airway problems, bronchospasm, and pulmonary edema, and touching the patient’s skin for clues about perfusion and body temperature.
Routine noninvasive monitors include electrocardiogram, blood pressure, pulse oximetry, capnography, and temperature. The electrocardiogram provides information about cardiac rate and rhythm and may detect myocardial ischemia. Blood pressure can vary depending on the depth of anesthesia, the degree of surgical stimulation, and the patient’s volume status. Pulse oximetry provides critical information about the adequacy of oxygenation and detects the presence of pulsatile blood flow. Capnometry and capnography detect the presence and adequacy of ventilation. Lastly, changes in body temperature occur routinely during anesthesia, and hypo- and hyperthermia are possible.
When paralytic agents are used during an anesthetic, neuromuscular function should be evaluated with a twitch monitor. This device consists of a pair of electrodes placed over a motor nerve (usually the ulnar or facial nerve). The electrodes are connected to a device that delivers a reproducible electrical stimulus. The most commonly used stimulus pattern is called a train-of-four (TOF), consisting of four equal pulses delivered at half-second intervals. In patients with normal neuromuscular function, these four pulses will elicit four equal muscular twitches. Stimulating the ulnar nerve will trigger finger flexion and thumb adduction. If the electrodes are on the facial nerve, the orbicularis oculi muscle causes the patient to wink. During onset of muscle paralysis, all four twitches will decrease at the same time and may completely disappear. As the effects of the nondepolarizing muscle relaxant begin to wane, the twitches reappear in a different pattern. Initially, only the first twitch appears. As neuromuscular function recovers further, the other twitches reappear. However, the first twitch (T1) is stronger than the subsequent twitches. The ratio of the fourth twitch (T4) to T1 is a measure of neuromuscular function. When T4:T1 is ≥0.9, the patient should be able to breathe normally and have intact upper airway reflexes (see Chapter 11). Incomplete recovery of neuromuscular function is common and is associated with hypoxemia, airway obstruction, and an increased risk of postoperative pulmonary complications (3).


Full access? Get Clinical Tree








