Muscle layers in the GI tract
Patterns of motility
Basal electrical rhythm (BER)
Distal to the oesophagus, smooth muscle cells exhibit spontaneous variations in transmembrane potential, between –70 and –40 mV, termed basal electrical rhythm (BER). This rhythm is controlled by the interstitial cells of Cajal, pacemaker cells with an intrinsic frequency. As in the myocardium, the pacemaker with the highest frequency dominates.
BER determines the maximum rate at which contractions can occur. When the transmembrane potential crosses the threshold voltage, approximately –40 mV, ion channels open. The resultant influx of sodium and calcium ions is seen as spike-burst activity, and this is associated with smooth muscle contraction (Figure 20.2). Gap junctions between neighbouring cells allow electrical activity to propagate such that smooth muscle cells act as a syncytium and contract in a coordinated manner.
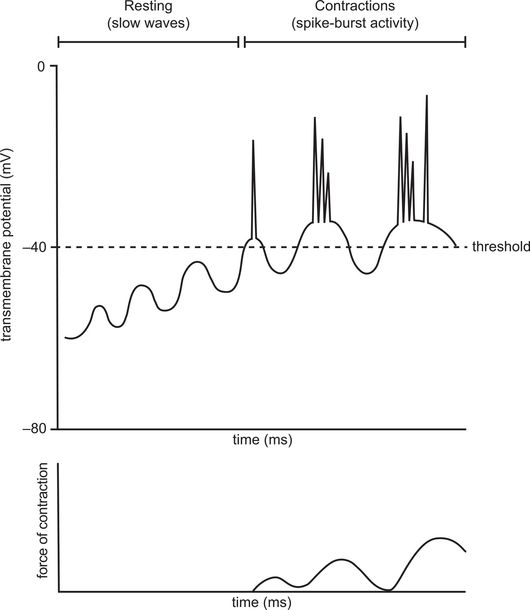
Basal electrical rhythm without and with spike potentials and relationship to muscular contraction
The frequency and amplitude of BER varies along the bowel and is modulated by nervous system control, hormones and drugs. Acetylcholine stimulates contraction by raising the cell membrane potential, thus increasing spike-burst activity. Conversely, adrenaline is inhibitory, hyperpolarising the cell membrane and reducing spike-burst activity.
Basal electrical rhythm (BER) determines the maximum rate at which contractions can occur. The frequency and amplitude of BER varies along the bowel and is modulated by nervous system control, hormones and drugs.
Peristalsis
Peristalsis is a reflex response to gut wall stretch that occurs throughout the GI tract. When luminal contents stretch the wall, a contraction forms behind that point and a relaxation is generated in front of it. Contents are then moved along the bowel by a wave of radially symmetrical contraction and relaxation of smooth muscle, similar to the mechanism used by earthworms to drive locomotion. It is a manifestation of two reflexes within the enteric nervous system (ENS). Mechanical distension stimulates afferent enteric neurones which synapse with two sets of interneurones. One group of interneurones activates excitatory motor neurones proximal to the bolus and stimulates contraction of smooth muscle. The other group of interneurones activates inhibitory motor neurones that stimulate relaxation of smooth muscle beyond the bolus.
Regulation mechanisms
Gut motility is modulated by neural and chemical control mechanisms which are complex and often work simultaneously on secretory function (Figure 20.3). Several gut reflexes, such as peristalsis, rely on the integrity of the myenteric plexus and although modulated by extrinsic nerve supply will continue in isolated bowel. Extrinsic neural input is predominantly involuntary via the autonomic nervous system through sympathetic and parasympathetic fibres. Somatic (voluntary) control is present only during the initial stages of swallowing and in external anal sphincter control of defecation.
| Modality | Nerves/ganglia | Sensory afferents | Secretomotor efferents | Motor efferents |
|---|---|---|---|---|
| Parasympathetic | Vagus and sacral fibres; preganglionic | Pain, distention, toxins | ↑ gastrin ↑ salivary production ↑ pancreatic and bile secretion | ↑ motility ↑ tone ↑ force of contraction ↑ gastric emptying |
| Sympathetic | Coeliac, mesenteric and pelvic ganglia; postganglionic | Pain, distention | ↑ salivary production | ↓ motility ↓ gastric emptying vasoconstriction |
Swallowing
Swallowing moves food from the mouth to the stomach without aspiration into the trachea. It is a reflex with voluntary and involuntary components which cannot be interrupted once initiated. Swallowing is coordinated by the swallowing centre located in the reticular system of the medulla and lower pons. This receives sensory inputs from the trigeminal, glossopharyngeal, superior laryngeal, recurrent laryngeal and vagus nerves, with motor efferents mainly carried by the vagus.
Oral stage
The oral or voluntary stage is the only part of the swallowing reflex where conscious control is possible. Masticated food is pushed into the pharynx by upward and backward pressure of the tongue against the hard palate.
Pharyngeal stage
Sensory receptors on the tonsillar pillars detect pressure from the food bolus and transmit signals to the swallowing centre, which then initiates the involuntary stages of the swallowing reflex. The soft palate is elevated, closing off the nasopharynx, and respiration is halted. The vocal cords are closed and the larynx moves anteriorly and cephalad, allowing the epiglottis to cover the glottis. This movement opens the upper oesophagus and contributes to upper oesophageal sphincter relaxation. The superior constrictor muscle of the pharynx initiates a wave of smooth muscle contraction that propels the bolus into the oesophagus.
Oesophageal stage
The primary peristaltic wave started in the pharynx moves the food bolus down the oesophagus where lower oesophageal sphincter (LOS) relaxation allows entry to the stomach. If primary peristalsis fails, secondary peristalsis is initiated by the continued stimulation of oesophageal stretch receptors.
Oesophagus
The oesophagus is 30 cm long in the adult and has upper and lower sphincters. The oesophagus differs from the rest of the GI tract in that the upper 6 cm consists of striated skeletal muscle with no spontaneous contractile activity.
The upper oesophageal sphincter consists of the cricopharyngeal and pharyngeal constrictor muscles. It is innervated by the vagus and is usually in a state of tonic contraction to prevent entrainment of air during respiration.
The lower oesophageal sphincter (LOS) is a functional zone of increased intraluminal pressure in the lower 2–4 cm of the oesophagus (Figure 20.4). The intrinsic component of the LOS is formed from semicircular oesophageal muscle fibres on the left and gastric sling fibres on the right. The external component is formed from the crural diaphragm. The LOS is usually closed but briefly relaxes during swallowing to allow the bolus to pass into the stomach.
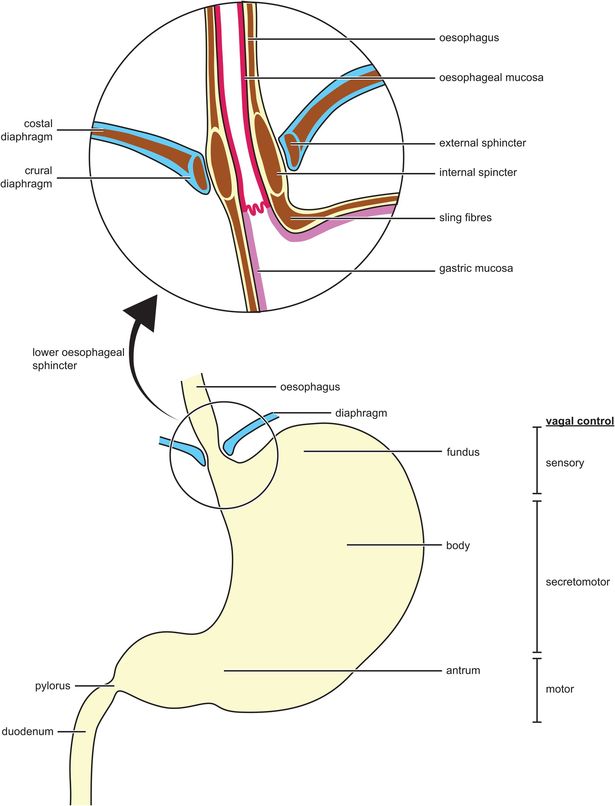
The lower oesophageal sphincter and the stomach
Barrier pressure
Barrier pressure is the pressure difference between the LOS and the intragastric pressure, normally 15–25 mmHg. When there is a fall in LOS tone or an increase in intragastric pressure, reflux of stomach contents into the oesophagus can occur, which encourages regurgitation, the passive transit of gastric contents into the pharynx (Figure 20.5). The acute angle where the oesophagus joins the stomach and the encircling diaphragmatic muscle results in a flutter-valve action below the diaphragm that helps to prevent reflux when intragastric pressure is raised.
| Increased LOS tone | Decreased LOS tone |
|---|---|
| Cholinergic stimulation (suxamethonium, neostigmine) Dopaminergic inhibition (metoclopramide, prochlorperazine) Gastrin α-adrenergic stimulation β-adrenergic blockade Motilin Prostaglandin F2 Cyclizine | Antimuscarinics (atropine, glycopyrrolate) Dopamine Cholecystokinin α-adrenergic blockade β-adrenergic stimulation Secretin Prostaglandin E1 Thiopental Alcohol |
Stomach
The stomach has three main types of contraction. Firstly, during the ‘fed’ state, the proximal stomach (fundus and upper body) exhibits slow sustained contractions that generate a basal intragastric pressure facilitating gastric emptying. As food enters the stomach the proximal stomach relaxes, minimising any further increase in intragastric pressure (receptive relaxation). Secondly there are rhythmic synchronised contractions in the lower part of the stomach (antral systole) which mix food with acid, mucus and pepsin, grinding it down to a fine paste called chyme. Chyme splashes against a contracted pyloric sphincter which allows the controlled passage of liquid and small food particles into the duodenum. Thirdly, between meals, there are occasional bursts of very strong, synchronised contraction that are accompanied by opening of the pyloric sphincter. These are called ‘housekeeper’ waves because their function is to sweep any indigestible material out of the stomach. They are initiated by motilin and halted by eating.
Gastric emptying
The pylorus does not close completely during antral systole, and small amounts of liquid chyme are squirted into the duodenum with each contraction. This emptying is regulated to optimise small bowel performance via complex control mechanisms. Gastric emptying is reduced with pain, anxiety and stress mediated by activation of the sympathetic nervous system. Distension of the stomach leads to the stimulation of vagal and local enteric reflexes and the release of gastrin. As a result there is increased secretion of acid and antral peristaltic activity, thereby increasing gastric emptying and the production of chyme.
The composition of the chyme reaching the duodenum also regulates gastric emptying. If the stomach empties too quickly, duodenal receptors may be activated by stretch, increasing acidity, osmolarity or concentration of fatty or amino acids. This initiates reflex arcs that reduce gastric emptying. As a result, carbohydrate-rich meals leave the stomach within a few hours, protein more slowly, and fatty food the slowest.
If small bowel contents rich in fat reach the ileum, an inhibitory reflex termed the ‘ileal brake’ reduces gastric emptying, pancreatic secretion and small bowel transit to improve digestion and absorption. This is hormonally mediated by peptide YY.
Small and large bowel
The small bowel is around 5 m long in the adult. Several motility patterns occur which contribute to transit times that are longer in the fed state compared with the fasted state, thus encouraging absorption.
The large bowel is important for absorption of water and electrolytes, the production of vitamins such as vitamin K by colonic bacteria, and the storage of faeces. The motility characteristics of the colon maximise contact with the mucosa and facilitate mass movement for defecation.

Full access? Get Clinical Tree







