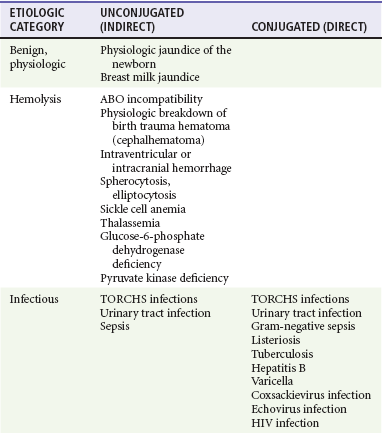
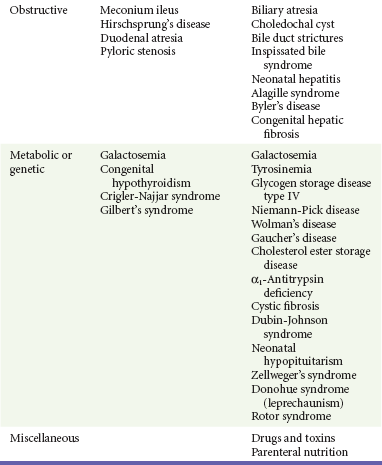
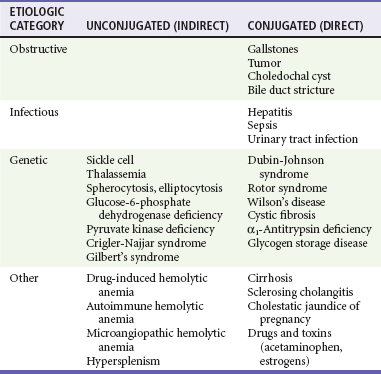
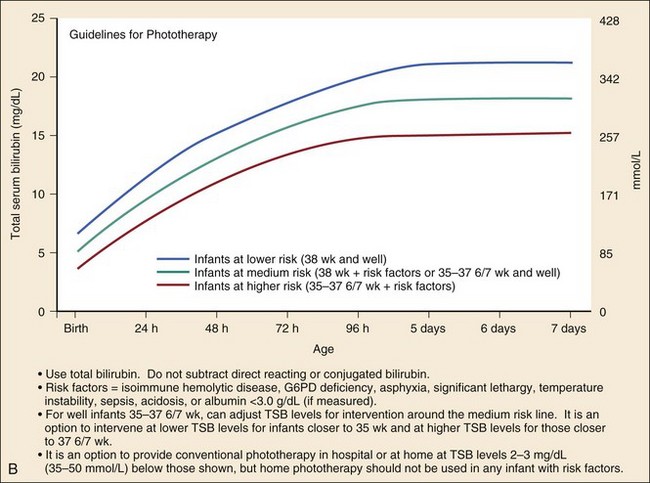
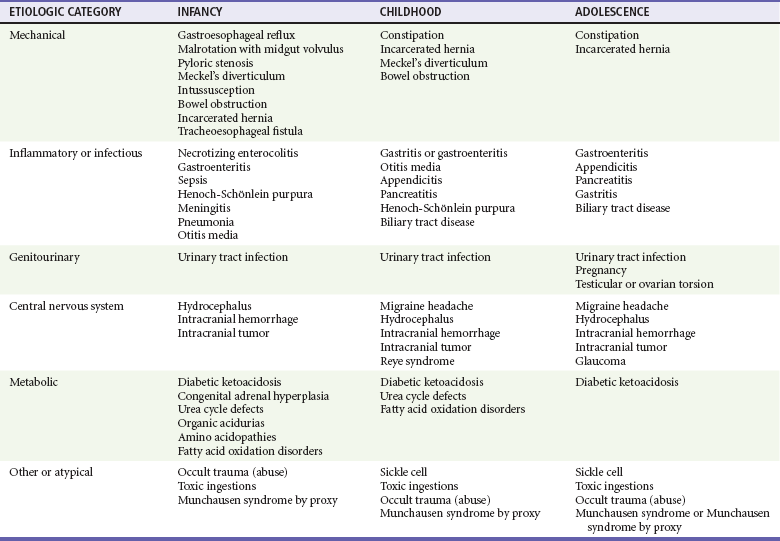
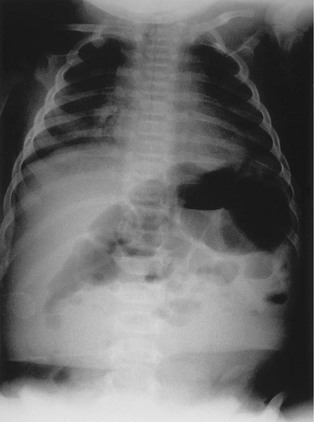
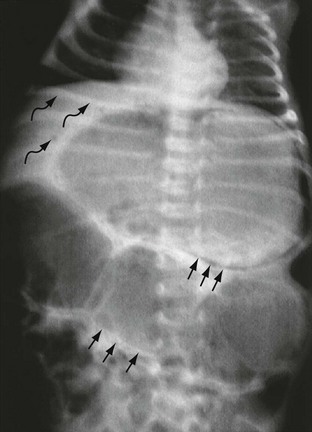
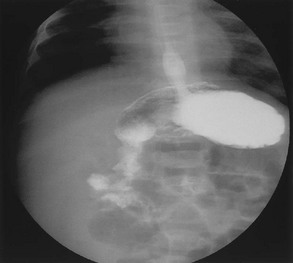
Chapter 172 The exact pathogenetic mechanism of breast milk jaundice is uncertain. Breast milk jaundice may be hormonally mediated or related to intestinal excretion and resorption of bile. Other causes of jaundice vary significantly, depending on the percentage conjugation and the age of the infant (Tables 172-1 and 172-2). Although jaundice in adults usually is the direct result of primary liver disease, infantile jaundice has a variety of extrahepatic causes—genetic, metabolic, infectious, and obstructive. The list of diagnostic possibilities in neonatal jaundice is extensive and requires careful consideration because the morbidity and mortality rates for many of these entities are high. Toxic levels of bilirubin (more than 20 mg/dL and dependent on age) may be associated with neurotoxicity, encephalopathy, and the development of kernicterus. Kernicterus is characterized by yellow staining in areas of the brain, including the basal ganglia. Clinical manifestations begin with poor feeding and lethargy and may progress to muscle rigidity, opisthotonos, seizures, and death. Survivors may have residual problems with coordination and hearing and learning disabilities.1 The cornerstones of therapy are phototherapy and exchange transfusion. Although physiologic jaundice of the newborn and breast milk jaundice are most common, it is important to identify truly pathologic causes of jaundice. Initial testing requires determination of fractionated levels of total and direct bilirubin. Box 172-1 lists indications for workup in infants presenting with hyperbilirubinemia. Conjugated (direct) hyperbilirubinemia is always pathologic. In such cases, a minimal workup should include a complete blood count (CBC) with peripheral smear and a Coombs test for immune-mediated major blood group incompatibility. Ill-appearing infants also require finger-stick blood glucose measurement, electrolyte panel, urine assay for reducing substances, and serum ammonia determination to rule out inborn errors of metabolism.2 Birth history should be obtained to elicit any history of trauma because large, resolving hematomas can result in jaundice. Family history should focus on identification of siblings or other relatives with a history of jaundice or genetic or metabolic disorders and any unexplained infant deaths. Tables 172-1 and 172-2 present full lists of differential considerations for jaundiced infants and children, respectively. Treatment of infants with hyperbilirubinemia centers on the prevention of kernicterus. Guidelines for use of phototherapy and exchange transfusion have been recommended by the American Academy of Pediatrics3 (Fig. 172-1). Feeding should be continued to the extent possible because oral intake stimulates enterohepatic circulation and decreases bilirubin levels. Unless the infant is severely jaundiced, breast-feeding can be continued and supplemented with formula as needed. Infants who are premature or who have significant comorbidities require treatment at lower levels. Phototherapy often is now readily available on an outpatient basis. Hypertrophic pyloric stenosis is the most common cause of infantile gastrointestinal obstruction beyond the first month of life. This condition occurs in 1 of every 250 live births.4 Boys are affected at four times the rate of girls. Hypertrophic pyloric stenosis tends to run in families; however, the exact pattern of inheritance is unclear. The incidence rate is 1 in 14 if the father is affected; the rate is even higher if the mother is affected.4 Whites are affected more often than African Americans, and the disease is rare in Asian Americans. Children may have a palpable pylorus, commonly referred to as an olive in the right epigastrium, on abdominal examination. Placement of a nasogastric tube and emptying the stomach or placement of the infant in the prone position often facilitates palpation. Hypertrophic pyloric stenosis may be confirmed by ultrasonography or upper gastrointestinal series. Ultrasonography is the diagnostic modality of choice because it is simple, readily available, and without serious complications such as aspiration. With both modalities, reported accuracy is greater than 95%. Ultrasound examination reveals a thickened pylorus, which is diagnostic.5 A characteristic “string sign,” reflecting passage of contrast material through the narrowed pyloric sphincter, can be seen in the upper gastrointestinal tract. In advanced stages with complete obstruction at the pylorus, plain films may reveal an enlarged body of the stomach and pylorus (Fig. 172-2). Etiologic possibilities vary by whether the course of vomiting has been sudden in onset, gradually progressive, or chronic. The frequency and volume of emesis may have important implications about the severity of disease and the potential risk for dehydration or electrolyte disturbance. In infants, other major considerations in the differential diagnosis include gastroesophageal reflux and malrotation. The age of the child and the timing of vomiting provide important clues to the etiology. Reflux classically begins early in life, usually shortly after birth, and remains relatively constant. With pyloric stenosis, vomiting does not begin until 2 to 3 weeks of age and then becomes increasingly severe and projectile; the emesis is rarely if ever bilious. In neonates, bilious vomiting requires diagnostic evaluation to rule out the possibility of malrotation with volvulus.6 The imaging modality of choice for pyloric stenosis is ultrasonography. Many causes of vomiting do not have a true gastrointestinal origin, including sepsis, increased intracranial pressure, middle ear disturbances, urinary tract infections, inborn errors of metabolism, pain, medications, and drug intoxications. Differential considerations for vomiting in children vary by age (Table 172-3). Treatment consists of fluid and electrolyte replacement and surgical consultation. Fluid resuscitation should begin with a bolus of 20 mL/kg of normal saline, followed by additional boluses as necessary to treat signs of shock. When the patient is stable and shows no signs of shock, 5% dextrose and half-normal saline at 1.5 to 2 times maintenance may be administered. Potassium supplementation is often necessary. Hypertrophic pyloric stenosis is a chronic, progressive disease, not an acute ischemic process. Confirmatory radiographic diagnosis with ultrasonography may be done on a semiurgent basis as the patient’s condition warrants. Pediatric surgical consultation is recommended although usually not emergent. The definitive corrective surgical procedure is the Ramstedt pyloromyotomy, which has an excellent track record of safety.7 More recently, laparoscopic pyloromyotomy has gained increasing acceptance as being safe and effective.8 Associated mortality is rare. Malrotation occurs in 1 in 500 live births and has a male predominance by at least 2 : 1.9 Among infants with malrotation, volvulus eventually will develop in approximately 75%, and 75% of these infants present within the first month of life. Overall, 90% of patients present within the first year of life, although cases of adult midgut volvulus have been reported.9 Bilious emesis is the hallmark presentation and is seen in more than 75% of cases.6,9,10 Malrotation with volvulus carries a mortality rate of 3 to 15%.9 During embryologic development, the gastrointestinal tract rotates around the superior mesenteric artery. As it completes the rotation, the duodenum forms a C-loop and is fixed to the retroperitoneum in the left upper quadrant at the ligament of Treitz. The cecum becomes similarly fixed in the right lower quadrant. The duodenum and cecum normally come to lie widely separated and loosely connected by a broad-based mesentery. They are fixed firmly in position by peritoneal attachments called Ladd’s bands. In cases of malrotation, the duodenum and the cecum do not rotate completely but end up close to each other, suspended in the midgut region by their vascular attachment containing the superior mesenteric artery. This unusually close proximity of the intervening mesentery results in a short stalk of mesentery that easily twists on itself, resulting in obstruction of the distal duodenum and compression of the superior mesenteric artery. Vascular compression results in ischemia of the bowel and, if it is not rapidly reversed, necrosis of the bowel wall in 1 to 2 hours.9,11 Twisting of the pedicle also results in various degrees of obstruction secondary to Ladd’s bands that are malpositioned and straddling the duodenum. Infants classically present with sudden-onset bilious emesis and abdominal distention.12 The obstruction may be relatively high, however; consequently, a distended abdomen may not always be present. Infants usually appear quite ill and may present in shock.13,14 Infants also may present with a history of intermittent, relatively mild episodes of emesis that suddenly become more intense. Although bilious emesis in a neonate suggests the possibility of acute obstruction and volvulus, presenting manifestations in children may be nonspecific, such as abdominal distention or an ill appearance.12,13 Diagnostic strategies may include a plain film of the abdomen, an upper gastrointestinal series, or a computed tomography (CT) scan of the abdomen. The imaging modality of choice is an upper gastrointestinal series with small bowel follow-through. Findings on plain abdominal films may include air-fluid levels suggesting obstruction, dilated loops overlying the liver, and a paucity of small bowel gas distally11 (Fig. 172-3). In addition, a “double-bubble sign” may be present. The classic double bubble represents a dilated stomach and obstructed proximal duodenum and is seen with duodenal atresia and malrotation with midgut volvulus. Duodenal atresia is limited to the newborn nursery and is manifested within 24 hours of life. Malrotation with midgut volvulus typically is manifested with bilious vomiting within the first month of life. The modified double-bubble sign seen with hypertrophic pyloric stenosis represents a dilated body of the stomach and pylorus and is associated with nonbilious emesis. The diagnostic procedure of choice to determine midgut volvulus is the upper gastrointestinal series, which reveals abnormal position of the duodenal C-loop (Fig. 172-4) and small bowel with a characteristic corkscrew appearance (Fig. 172-5).11 It is very low risk, but an experienced technician or a radiologist is required to perform the test. An ultrasound scan may be obtained because of abdominal pain and may reveal abnormal positioning of the duodenal C-loop and superior mesenteric artery; a “whirlpool sign” is described with the spiraled mesentery causing an echogenic twisting pattern. The place of ultrasonography in the evaluation of children with midgut volvulus has yet to be determined.10,15 CT is usually not recommended as it carries the risk of additional radiation without benefit of improved diagnostic ability over upper gastrointestinal series. Figure 172-4 Upper gastrointestinal film, obtained in the same infant as in Figure 172-3, reveals abnormal positioning of the duodenal C-loop to the right of the spinal column, consistent with malrotation. (Courtesy Mark A. Hostetler, MD.) Figure 172-5 Another spot film from the upper gastrointestinal series obtained in the infant in Figure 172-3. This radiograph shows the characteristic corkscrew appearance seen on small bowel follow-through in patients with malrotation. (Courtesy Mark A. Hostetler, MD.) Vomiting in childhood is common and occurs across a wide spectrum of illnesses (see Table 172-3). Causes vary by the age of the child and whether the course of vomiting has been sudden in onset, gradually progressive, or chronic. Gastroesophageal reflux classically begins early in life, usually shortly after birth, and remains relatively constant. With pyloric stenosis, vomiting does not begin until the age of 2 to 3 weeks and then becomes increasingly severe, projectile, and nonbilious. Acute obstruction causes sudden-onset vomiting, which may be bilious. In a neonate, bilious vomiting requires diagnostic evaluation to rule out the possibility of malrotation with volvulus.12,13 NEC is another consideration but most often is manifested within the first weeks of life. Neonates with NEC may present with obstructive signs and symptoms, including bilious emesis and abdominal distention. Whereas malrotation usually is associated with a paucity of small bowel air on plain films, NEC is characterized radiographically by diffusely dilated loops of small bowel. In addition, the presence of pneumatosis intestinalis is diagnostic of NEC but is not a feature of malrotation. Infants with bilious emesis of sudden onset who appear ill or have a distended abdomen require emergency consultation with a pediatric surgeon.16 Intravenous access should be obtained and laboratory studies performed for CBC, electrolyte values, and liver function. Repeated fluid boluses of normal saline, 20 mL/kg, are necessary until adequate circulation has been obtained. A finger-stick sample for blood glucose determination and specimens for blood and urine cultures should be obtained. A nasogastric or orogastric tube should be placed. After consultation with a pediatric surgeon, an upper gastrointestinal series may be needed emergently. Ill-appearing infants require broad-spectrum, triple-antibiotic coverage with ampicillin, gentamicin, and either clindamycin or metronidazole. Time is of the essence in the evaluation and operative management of these patients. Rapid pediatric surgical consultation should be obtained in any neonate or infant with bilious vomiting even before diagnostic studies have been performed, especially for infants who appear ill. In contrast to hypertrophic pyloric stenosis, in which surgery does not need to be immediate, operative intervention must be rapid to save the bowel from necrosis. NEC, the most common gastrointestinal emergency in neonates, affects 2000 to 4000 infants in the United States every year.17 NEC also is the most common cause of intestinal perforation during the newborn period.17 Because most affected infants are premature and acquire the condition in the neonatal intensive care unit, NEC usually is not considered a disease of the emergency department (ED). Many of these infants may be discharged relatively early, however, because they are “feeding and growing” and come to treatment in the first month of life. Ten percent of infants with NEC are full-term babies.18 Development of NEC is related closely to gestational age. In infants born at 24 to 28 weeks of gestation, NEC develops within 2 to 3 weeks of life19; in those born at 29 to 32 weeks of gestation, it is seen within 1 to 3 weeks of life. Among more mature or full-term infants, NEC tends to develop in the first week of life.17 Complications in children who survive NEC may include strictures (in 10-20% of cases), fistulas, and short gut syndrome. The exact pathophysiologic mechanism of NEC is unclear but seems to be multifactorial. Proposed risk factors include prematurity, aggressive enteral feedings, birth-related hypoxic-ischemic insults, and infectious causes. Prematurity is the most common and universally accepted risk factor; 90% of all affected infants are premature at birth.18,19 Rapid advancement of feedings also has been associated with increased rates of NEC.20 Infection has been implicated as an important causative mechanism.21 Evidence suggests that hypoxic-ischemic insults are not an independent risk factor for the development of NEC.18 The primary pathologic event may be inflammation or injury to the intestinal wall, which begins in the mucosa and then extends transmurally. The distal ileum and proximal colon are more commonly affected, and the involvement may be continuous or patchy.22 Infants with NEC present with feeding intolerance and emesis. Emesis may be either nonbilious or bilious. On occasion, individual loops of bowel become distended with air and are palpable on abdominal examination. In the more severe stages of the disease, infants may appear extremely ill, with hematemesis, hematochezia, and shock. NEC commonly is placed into one of three clinical stages on the basis of criteria developed by Bell.23 Stage I represents early or suspected NEC based on feeding intolerance, vomiting, or ileus. Stage II represents definite NEC as proved by abdominal radiographs showing intestinal dilation and pneumatosis intestinalis. Stage III represents advanced disease and is associated with perforation. Infants in this stage are acutely ill, with marked abdominal distention, metabolic acidosis, disseminated intravascular coagulation, and shock. Dilated loops of bowel are a common but nonspecific finding in stage I. Another early and more specific radiographic sign is the loss of a normal symmetrical gas pattern and replacement with an asymmetrical pattern of bowel gas, with a variable degree of dilation. Intramural air (pneumatosis intestinalis) is specific for NEC and is present in stage II23 (Fig. 172-6). Pneumatosis is present in 75% of patients with NEC.18 Air also may be seen within the biliary tract (portal vein gas) or occasionally in the gastric wall (pneumatosis gastralis; see Fig. 172-6). Portal vein gas is present in 10 to 30% of cases.18 Ultrasonography and barium enema, which have been described as adjunctive diagnostic imaging modalities in patients with suspected NEC, are rarely helpful in the ED. No individual laboratory features are diagnostic or specific for NEC. Etiologic possibilities vary according to whether the emesis is bilious and the course of vomiting has been sudden in onset, gradually progressive, or chronic (see Table 172-3). Gastroesophageal reflux classically begins early in life, usually shortly after birth, and remains relatively constant in character. Pyloric stenosis—related vomiting does not begin until 2 to 3 weeks of age and then becomes increasingly severe and projectile. In neonates, bilious vomiting requires careful consideration to rule out the possibility of malrotation with volvulus. As noted previously, with malrotation, a paucity of small bowel air usually is noted on plain films, whereas with NEC, diffusely dilated loops of small bowel typically are seen. In addition, the presence of pneumatosis is diagnostic of NEC but is not a radiographic feature of malrotation. Patients thought to have NEC should receive nothing by mouth (i.e., NPO [nil per os] status), with placement of either an orogastric or a nasogastric tube for decompression of the stomach and small bowel. These patients frequently appear quite ill and may have periods of apnea or significant respiratory distress. The airway should be secured as indicated. Intravenous access should be established and routine laboratory studies performed to include CBC, electrolyte panel, type and screen, and coagulation studies (prothrombin time [PT] and partial thromboplastin time [PTT]). A bedside blood glucose value should be obtained. Cultures of the blood and urine also are indicated. Careful attention should be given to management of fluids and electrolytes because considerable third spacing of fluids may occur in these patients. Repeated fluid boluses at 20 mL/kg of normal saline should be administered until adequate circulation is obtained. These boluses may be augmented with dopamine or epinephrine drips as necessary for patients in refractory shock when euvolemia has been achieved. Fluids should be continued with 5% dextrose in water and half-normal saline at a minimum of 1.5 to 2 times maintenance. Infants with NEC require broad-spectrum, triple-antibiotic coverage with ampicillin, gentamicin, and either clindamycin or metronidazole. Emergent consultation should be obtained from a pediatric surgeon. Patients with evidence of perforation, peritonitis, or gangrenous bowel require surgical intervention. Only one half to three quarters of patients with perforation have free air detectable on radiographs.23 Intussusception is the most common cause of intestinal obstruction in children younger than 2 years and occurs most commonly in infants 5 to 12 months of age.11,23 An estimated incidence of 1 per 2000 children younger than 15 years, with a male predominance, has been reported.23 Siblings of affected children have a relative risk 15 to 20 times higher than that in the general population. The mortality rate for untreated intussusception is high. The exact etiology of intussusception is unclear, but the most prevalent theory relates to a lead point that causes telescoping of one segment of intestine into another.23 As the process continues and intensifies, edema develops and obstructs venous return, resulting in ischemia of the bowel wall. As ischemia of the bowel wall continues, peritoneal irritation ensues, and perforation may occur. In younger children, lead points are most often the result of enlarged Peyer’s patches secondary to a recent viral infection. In children older than 5 years, an underlying lesion is found in more than 75% of cases; lesions include HSP vasculitis, Meckel’s diverticulum, lymphoma, polyps, postsurgical scars, celiac disease, and cystic fibrosis.23–27 Intussusception may occur at any point along the gastrointestinal tract. Ileocolic intussusceptions are most common. Ileoileal intussusception may occur in children with HSP.
Gastrointestinal Disorders
Specific Disorders
Principles of Disease
Clinical Features
Diagnostic Strategies
Differential Considerations
Management
Hypertrophic Pyloric Stenosis
Diagnostic Strategies
Differential Considerations
Management
Malrotation with Midgut Volvulus
Principles of Disease
Clinical Features
Diagnostic Strategies

Differential Considerations
Management
Necrotizing Enterocolitis
Principles of Disease
Clinical Features
Diagnostic Strategies
Differential Considerations
Management
Gastroesophageal Reflux
Intussusception
Principles of Disease

Full access? Get Clinical Tree


Gastrointestinal Disorders
Only gold members can continue reading. Log In or Register to continue