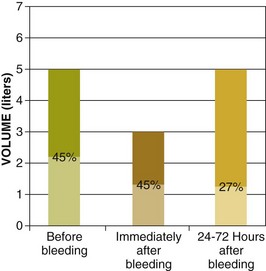
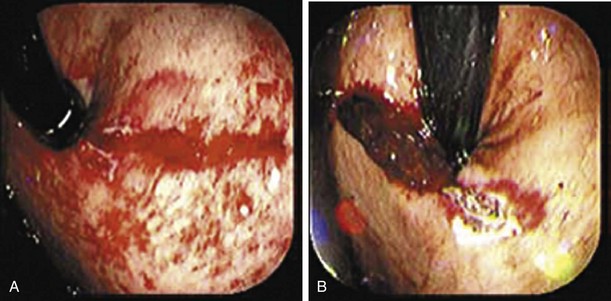
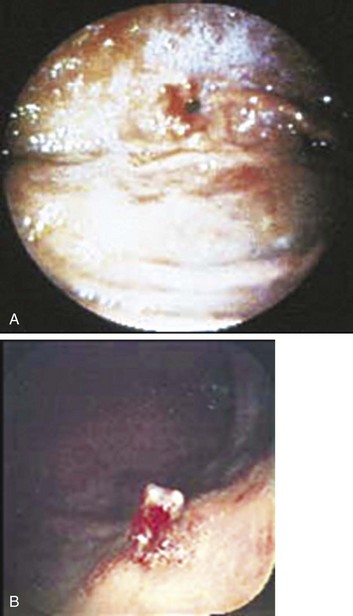
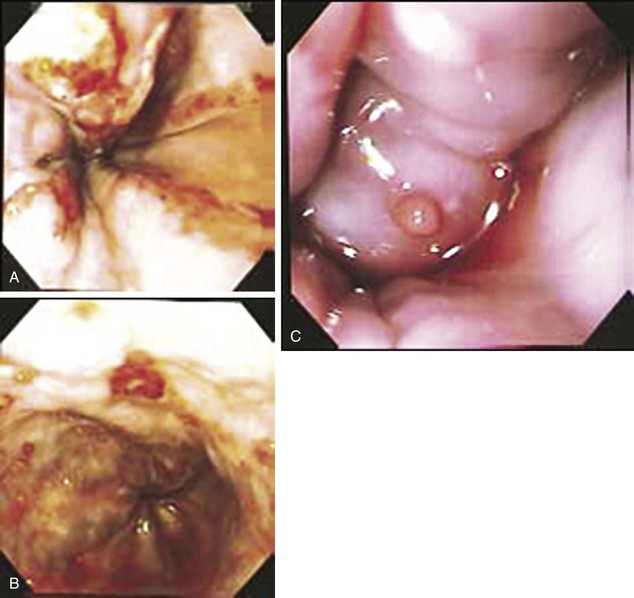
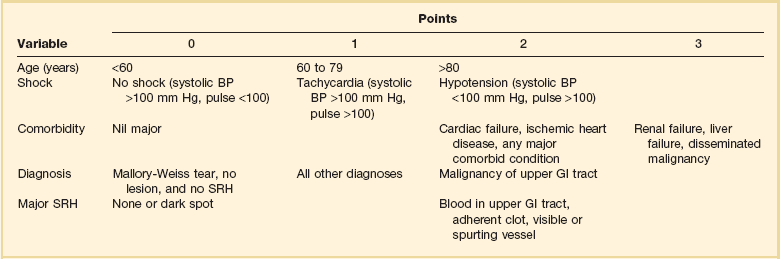
76 More than 300,000 annual hospitalizations in the United States are attributed to GI bleeding.1 Upper GI bleeding accounts for most of these hospitalizations, with an incidence rate of 100 cases per 100,000,1 whereas the incidence of lower GI bleeding is estimated at 20 to 27 cases per 100,000.2,3 Mortality rates vary depending on the source of the bleeding. Most nonvariceal upper GI bleeding studies document mortality rates approximating 10%.4,5 These rates have not changed over the past 2 decades despite the evolution of acid suppression therapy, which is probably explained by an aging population with increased comorbid diseases. Mortality rates for lower GI bleeding are usually in the range of 5%.6,7 The clinical findings in a patient with GI bleeding are crucial in determining the site, cause, and rate of bleeding. The first step in clinical evaluation is to assess the severity of the bleeding. This is done primarily by measuring hemodynamic parameters in an attempt to quantify the amount of blood volume lost (Table 76.1).8 Because bleeding can represent a dynamic ongoing situation, continuous monitoring of hemodynamics is necessary to guide resuscitation efforts and provide key prognostic information. In patients with GI bleeding, two large-bore intravenous catheters should be placed immediately on arrival to restore euvolemia. Table 76.1 Hemodynamics, Vital Signs, and Blood Loss From Rockey DC: Gastrointestinal bleeding. Gastroenterol Clin North Am 2005;34:581-588. The hematocrit at initial evaluation may not reflect the severity of the bleeding because very recent loss of both plasma and red blood cells leads to a percentage of red blood cells in the remaining blood (which defines the hematocrit) that is close to the same value. The hematocrit drops when hemodilution occurs as extravascular fluid enters the vascular space to restore volume, a process that may take up to 72 hours (Fig. 76.1).9 The rapidity of blood and colloid infusion depends in part on the patient’s cardiovascular condition. Placement of a central venous pressure catheter can help one base decisions on more objective findings. Several recent studies found that transfusion was associated with higher risk for nosocomial infection, multiorgan dysfunction, acute respiratory distress syndrome, and death.10 Current transfusion trends are to administer blood to patients with hemoglobin less than 7 mg/dL and to avoid transfusion when it’s above 10 mg/dL. However, the threshold for blood transfusion should take into consideration the patient’s underlying condition, hemodynamic status, and markers of tissue hypoxemia.11 In patients with conditions associated with defects in platelet or coagulation factors, these substances should be replaced. Patients requiring massive transfusion of packed red blood cells require fresh frozen plasma and platelets. Hypocalcemia can develop in these patients because of the large amount of citrate received with massive transfusion, and thus calcium replacement should be considered, especially in individuals with end-stage liver disease and heart failure, in whom citrate metabolism may be impaired.12 The initial evaluation of patients with nonvariceal upper GI bleeding should include risk stratification of patients into low- and high-risk categories for rebleeding and death based on clinical, laboratory, and when available, endoscopic criteria.10 This allows appropriate intervention and minimizes morbidity and mortality risks. The most extensively validated scores for risk stratification are the Blatchford and Rockall scores13,14 (Tables 76.2 and 76.3). Similarly, risk stratification in lower GI bleeding helps in guiding the management of these patients. Hemodynamic instability, ongoing hematochezia, and comorbid illnesses have been consistently associated with poor outcome in lower GI bleeding.15 Table 76.2 Blatchford Score for Gastrointestinal Bleeding* *The score is calculated by adding the points from each variable. A score of zero is associated with a low risk of the need for endoscopic intervention From Blatchford O, Murray WR, Blatchford M: A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet 2000;356:1318-1321. Table 76.3 Rockall Scoring System for Risk of Rebleeding and Death in Acute Gastrointestinal Bleeding* BP, blood pressure; GI, gastrointestinal; SRH, stigma(ta) of recent hemorrhage. *The score is calculated by adding the points from each variable. A score of 2 or less is associated with a low risk of further bleeding or death. From Rockall TA, Logan RF, Delvin HB, et al: Risk assessment after acute upper gastrointestinal haemorrhage. Gut 1996;38:316-321. After hemodynamic stabilization is achieved, a careful history and clinical examination are imperative to make a preliminary assessment of the location and cause of the bleeding. Important historical features in the evaluation of GI bleeding are shown in Box 76.1.8 Hematemesis typically points to an upper source of bleeding, proximal to the ligament of Treitz. In rare cases, hematemesis can be a sign of swallowed blood from oral, pharyngeal, or nasal bleeding. Melena is defined as black tarry stool with a glistering sheen and results from degradation of blood in the GI tract. At least 50 mL of blood in the upper GI tract is required to cause melena, although volumes up to 100 mL may be clinically silent.16 Melena usually indicates upper GI bleeding, but its source may be the small bowel and sometimes even the proximal part of the colon when the volume of blood is too small to cause hematochezia. Coffee-ground emesis is typically a sign of recent, but currently inactive upper GI bleeding, and its appearance is caused by the acid’s effect on blood in the lumen. Hematochezia is generally associated with colonic bleeding but can also be caused by more proximal bleeding. Proximal bleeding in association with hematochezia is usually more hemodynamically significant. The use of a nasogastric tube in patients presenting with GI bleeding is a common practice but at the same time controversial. The presumed benefits of nasogastric lavage include confirmation of an upper GI source of bleeding, better visualization during endoscopy, and prediction of high-risk lesions such as an oozing or spurting lesion and nonbleeding visible vessel. A bloody aspirate suggests, with some degree of certainty, an upper source of bleeding because false-positive results are rare and generally related to nasogastric trauma.17 In one study looking at patients presenting with suspected upper GI bleeding, 45% of cases with a bloody aspirate were associated with a high-risk lesion on endoscopy versus 15% when the aspirate was clear or bilious.18 Identifying patients with high-risk lesions is important because those patients have the worst outcome and early endoscopic therapy may have the most benefit. However, the positive and negative predictive values of a bloody aspirate for high-risk lesions are only 45% and 85%, respectively, which makes basing the decision of an early endoscopy on the information obtained by the nasogastric lavage controversial. In a recent retrospective study looking at the impact of performance of nasogastric lavage, this practice was associated with earlier time to endoscopy but had no effect on mortality rate, length of hospital stay, surgery, or transfusion requirements.19 In our opinion, if an upper endoscopy is planned in the next 12 to 24 hours after presentation of a patient with suspected upper GI bleeding, nasogastric lavage should be avoided owing to lack of proven benefit and major discomfort and pain inflicted to the patient. In the setting of hematochezia with hemodynamic instability, extremely brisk upper GI bleeding should be suspected, and a positive nasogastric aspirate can confirm this suspicion. The initial laboratory evaluation in patients with GI bleeding should include a complete blood count, liver enzymes, prothrombin time, blood urea nitrogen (BUN), and creatinine. As mentioned earlier, the first hematocrit level may be falsely reassuring, so management decisions should rely on other parameters such as hemodynamics and the nature of the bleeding. A high white blood cell count should alert one to the presence of ischemia or infarction. Thrombocytopenia can be a sign of portal hypertension, and a critically low platelet count, as well as a high prothrombin time, should be addressed immediately by transfusion of platelets and fresh frozen plasma. An elevation in the BUN level out of proportion to creatinine is compatible with upper GI bleeding but may also be seen with intravascular volume depletion from any source of bleeding. In one study, this ratio was significantly higher in patients with upper GI bleeding than in those with lower GI bleeding (22.5 ± 11.5 vs. 15.9 ± 8.2; p = 0.001); however, the degree of overlap shows the poor discriminatory value of this ratio.20 In another study, a ratio greater than 36 had a specificity of 27% and a sensitivity of 90% for upper GI bleeding.21 Nonvariceal upper GI bleeding remains a significant cause of death and morbidity despite recent advances in pharmacologic and endoscopic therapy. The cause of nonvariceal bleeding encompasses a large array of diagnoses involving multiple organs above the ligament of Treitz and at times outside the GI tract. The causes and frequency of nonvariceal bleeding are listed in Table 76.4.22 Table 76.4 Causes of Nonvariceal Upper Gastrointestinal Bleeding From Ferguson CB, Mitchell RM: Nonvariceal upper gastrointestinal bleeding: Standard and new treatment. Gastroenterol Clin North Am 2005;34:607-621. PUD traditionally refers to gastric and duodenal ulcers, gastritis, and duodenitis. A number of population-based and prospective studies rank PUD as the most common source of acute upper GI bleeding, with PUD representing up to 50% of all such cases.23 However, recent analysis from the Clinical Outcomes Research Initiative (CORI) database reported that the most common endoscopic finding in persons with acute upper GI bleeding was “mucosal abnormality” (40%), and gastric or duodenal ulcers were found in 20.6%.24 Eradication of Helicobacter pylori and extensive use of PPIs are probably responsible for this observed decline in the frequency of PUD. The most important factors predisposing to ulcer disease include acid, H. pylori infection, and NSAIDs; however, the role of some of these risk factors in inducing ulcer bleeding remains unclear. Indirect evidence regarding the role of acid in ulcer bleeding comes from data showing that acid suppression by PPIs in patients with active or recent bleeding reduces the risk for rebleeding.25 Evidence of the association between NSAIDs and ulcer bleeding is strong and comes from both placebo-controlled and case-control studies.26,27 The pathogenesis of bleeding from an ulcer involves aneurysmal dilation with an intense arteritis associated with a marked inflammatory response.28 When eroding into large vessels, ulcers can cause catastrophic bleeding. This most commonly occurs in the posterior portion of the duodenal bulb, where ulcers can erode directly into the pancreaticoduodenal artery. Mallory-Weiss tears (MWTs) are mucosal and occasionally submucosal lacerations caused by sudden increases in pressure within the cardia and lower esophagus produced by retching. MWTs are responsible for 5% to 15% of upper GI bleeding.23 The majority of upper GI bleeding caused by MWTs stops spontaneously and does not require any blood transfusion or endoscopic treatment. However, some cases are severe enough to require endoscopic hemostasis and occasionally angiography with embolization or even surgery. A history of retching on arrival at the emergency department is not always present.29 Endoscopically, tears are usually 1.5 to 2 cm in length and occur at the gastroesophageal junction or, most commonly, in the proximal part of the stomach (Fig. 76.2). Angiodysplasia, also referred to as arteriovenous malformation or vascular ectasia, is another source of upper GI bleeding and accounts for approximately 5% to 10% of cases.23 It occurs in inherited syndromes such as hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome) and blue rubber bleb nevus syndrome, but most cases are acquired.30 The association of angiodysplasia with medical conditions such as renal failure, aortic stenosis, connective tissue disease (scleroderma), and von Willebrand disease has been recognized, but the evidence for these associations is limited.23,31 Dieulafoy’s lesion is an underrecognized cause of upper GI bleeding and is described as a visible vessel protruding from a small mucosal defect without any underlying ulcer.23 It has also been called “caliber-persistent artery” in submucosal tissue. Bleeding from Dieulafoy’s lesion represents less than 5% of cases of upper GI bleeding.32,33 The lesion is generally located on the lesser curvature within 6 cm of the gastroesophageal junction and can be difficult to detect because of its small size and normal surrounding mucosa (Fig. 76.3).31 Benign and malignant neoplasms are responsible for less than 5% of upper GI bleeding.34 Bleeding can be the initial symptom of tumors originating from the esophagus, stomach, or small intestine. These neoplasms can be primary malignancies, such as adenocarcinoma of the esophagus, stomach, or duodenum; squamous cell carcinoma of the esophagus; and gastric or duodenal lymphomas. Gastrointestinal stromal cell tumors (GISTs), carcinoid tumors, and lipomas are examples of benign tumors that can cause upper GI bleeding.23 Upper GI bleeding from an aortoenteric fistula is very rare but should be considered in the appropriate clinical setting (such as a patient with a history of aortic aneurysm repair). Fistulas are generally located in the third portion of the duodenum. Patients will frequently have a small hemorrhage first, known as a “herald bleed,” that occurs before a major hemorrhage.35 Hemosuccus pancreaticus is an uncommon cause of upper GI bleeding that occurs secondary to pseudoaneurysm formation and rupture into the pancreatic duct as a complication of a pancreatic pseudocyst in patients with chronic pancreatitis.36 The incidence of varices among all cirrhotic patients is around 50%. However, if monitored long enough, varices eventually develop in most cirrhotics.37 Variceal hemorrhage occurs in a third of cirrhotic patients with varices. Although portal hypertension is defined by an HVPG greater than 5 mm Hg, Garcia-Tsao and colleagues showed that varices do not develop and hence do not bleed as long as the HVPG is less than 12 mm Hg.38 However, once this threshold is reached, there is poor correlation between the pressure gradient and the risk for bleeding. Other risk factors associated with variceal bleeding include the degree of liver disease (provided by Child’s classification), variceal location and size (higher risk near the gastroesophageal junction and with large varices), and the presence of particular endoscopic signs (red wale markings suggestive of dilated longitudinal venules, cherry-red spots, and hematocystic spots consisting of small red dots or a reddish blister-like formation on the variceal surface and the white or purple nipple sign on a varix) (Fig. 76.4).37,39 Sarin and colleagues classified gastric varices into two groups: (1) isolated gastric varices (IGVs) and (2) gastroesophageal varices (GEVs) that are continuous with esophageal varices and extending to the cardia (GEV 1) or to the fundus (GEV 2).40 The authors found that GEV 1 was the most common type of gastric varix but IGV was the type that bleeds the most. Although the incidence of bleeding from gastric varices is in the range of 10% to 36%, it is usually massive and associated with high mortality rates.41 After the initial evaluation, resuscitation, and stabilization of a patient with upper GI bleeding, effort is directed at localization and treatment of the hemorrhage. Endoscopy has become the preferred diagnostic and therapeutic modality for upper GI bleeding because of its accuracy and low complication rate. With its use, a specific diagnosis can be achieved in 95% of patients. The use of promotility agents such as metoclopramide and intravenous erythromycin (250 mg by intravenous bolus or 3 mg/kg over a 30-minute period) before the endoscopic examination can significantly improve mucosal visibility by promoting gastric motility and emptying of gastric contents.42–44 An analysis of data from erythromycin trials showed that pre-endoscopic erythromycin was cost effective.45 The optimal timing of endoscopy remains a balance between clinical need and resources and is still subject to controversy.22 Recent guidelines recommend the performance of upper endoscopy within 24 hours in patients with suspected nonvariceal upper GI bleeding.11 Endoscopy has to be delayed or deferred in selected high-risk patients such as patients with bowel perforation or acute coronary syndrome. In a meta-analysis looking at timing of endoscopy, no significant reduction in rebleeding, surgery, or mortality rate was found with urgent endoscopy (1 to 12 hours) compared with later endoscopy (more than 12 hours).11 In a subset of patients with bloody gastric lavage, length of hospital stay and blood tranfusion requirements were significantly lower in the urgent endoscopy group (within 12 hours).46 One major role of endoscopy is to identify stigmata of recent hemorrhage known to correlate well with an increased risk for rebleeding and thus a need for endoscopic therapy. Rates of rebleeding with these specific endoscopic findings are summarized in Table 76.5.47 Table 76.5 Stigmata of Ulcer Hemorrhage and Risk for Recurrent Bleeding without Endoscopic Therapy From ASGE Standards of Practice Committee: ASGE guideline: The role of endoscopy in acute nonvariceal upper GI-hemorrhage. Gastrointest Endosc 1999;49:145-152; and from ASGE Standards of Practice Committee: ASGE guideline: The role of endoscopy in acute nonvariceal upper GI-hemorrhage. Gastrointest Endosc 1999;49:145-152. Treatment with PPI before the performance of upper endoscopy has been shown to down-stage the endoscopic lesion and decrease the need for endoscopic intervention.11 However, a meta-analysis including studies assessing oral, intravenous, and high-dose PPI failed to show significant differences in rates of mortality, rebleeding, or surgery between, the pre-endoscopic PPI therapy and control groups.48 Once endoscopy is performed, the role of PPI therapy becomes more obvious. In patients found to have high-risk lesions treated endoscopically, an intravenous bolus followed by continuous-infusion PPI therapy is indicated.11 The use of a continuous infusion is supported by data showing that maintenance of intragastric pH at greater than 6 after endoscopic hemostasis is associated with the lowest rebleeding rates and that this goal can be achieved only by bolus administration of a PPI followed by a constant infusion.49 Strong data from several studies showed significant benefit in rebleeding, surgery, and mortality rates with high-dose intravenous PPI therapy after endoscopic treatment.50 Other reports suggest similar benefits from low-dose intravenous and high-dose oral PPI therapy but these remain to be confirmed in larger studies. Other agents with different mechanisms of action have been studied in patients with upper GI bleeding. A reduction in splanchnic blood flow with somatostatin and its analogs (such as octreotide) is an attractive measure in patients with upper GI bleeding and has been the subject of several trials, with conflicting results.51–53 To date, the available data are not convincingly in favor of using these agents in patients with nonvariceal upper GI bleeding, even though some authors find them useful in patients who are bleeding uncontrollably while awaiting endoscopy or surgery or in whom surgery is contraindicated.51
Gastrointestinal Bleeding
Clinical Presentation
Initial Evaluation and Resuscitation
Hemodynamics and Vital Signs
% Blood Loss (Fraction of Intravascular Volume)
Bleeding Type
Shock (resting hypotension)
20-25
Massive
Postural (orthostatic tachycardia or hypotension)
10-20
Moderate
Normal
<10
Minor
Admission Parameter
Score Value
Urea (mg/dL)
≥6.5 to <8.0
2
≥8 to <10
3
≥10 to <25
4
≥25
6
Hemoglobin (g/dL)
Men
≥12 to <13
1
≥10 to <12
3
<10
6
Women
≥10 to <12
1
<10
6
Systolic blood pressure (mm Hg)
100 to 109
1
90 to 99
3
<90
3
Other parameters
Pulse >100
1
Melena at presentation
1
Syncope
2
Hepatic disease
2
Cardiac failure
2
History and Clinical Findings
Diagnostic Tests
Upper Gastrointestinal Bleeding
Differential Diagnosis
Nonvariceal Bleeding
Diagnosis
Incidence (%)
Peptic ulcer
30-50
Mallory-Weiss tear
15-20
Erosive gastritis or duodenitis
10-15
Esophagitis
5-10
Malignancy
1-2
Angiodysplasia or vascular malformations
5
Other
5
Peptic Ulcer Disease
Other Sources of Nonvariceal Upper Gastrointestinal Bleeding
Bleeding Secondary to Portal Hypertension
Esophageal Varices
Gastric Varices
Diagnostic Evaluation
Endoscopic Examination
Endoscopic Finding
Risk for Recurrent Bleeding without Therapy
Active arterial (spurting) bleeding
Approaches 100%
Nonbleeding visible vessel (“pigmented protuberance”)
Up to 50%
Nonbleeding adherent clot
30-35%
Ulcer oozing (without other stigmata)
10-27%
Flat spots
<8%
Clean-based ulcers
<3%
Therapeutic Alternatives
Nonvariceal Bleeding
Pharmacotherapy

Full access? Get Clinical Tree


Gastrointestinal Bleeding