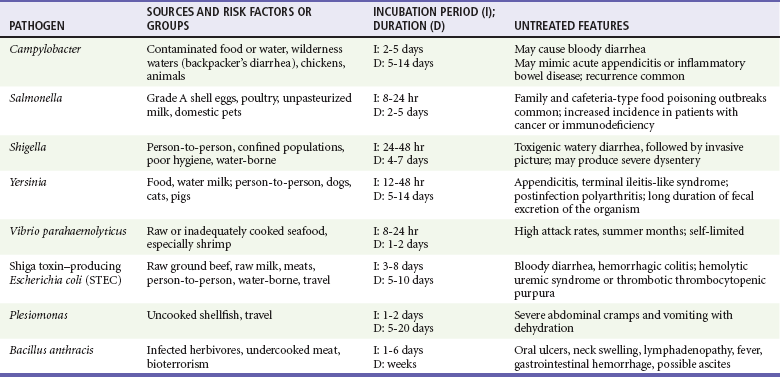
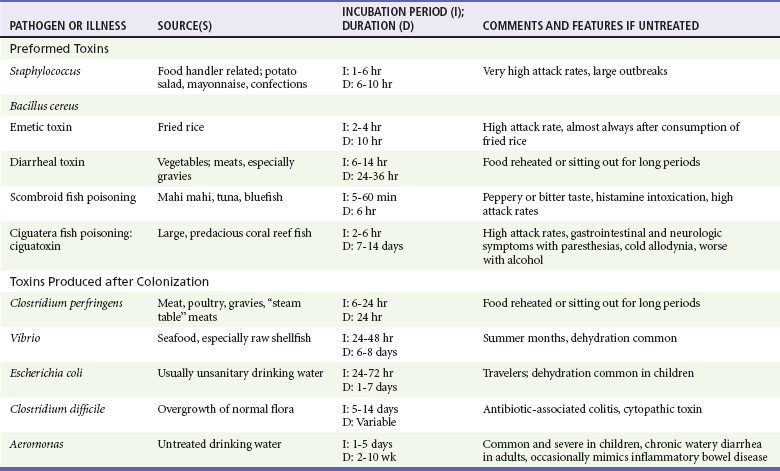
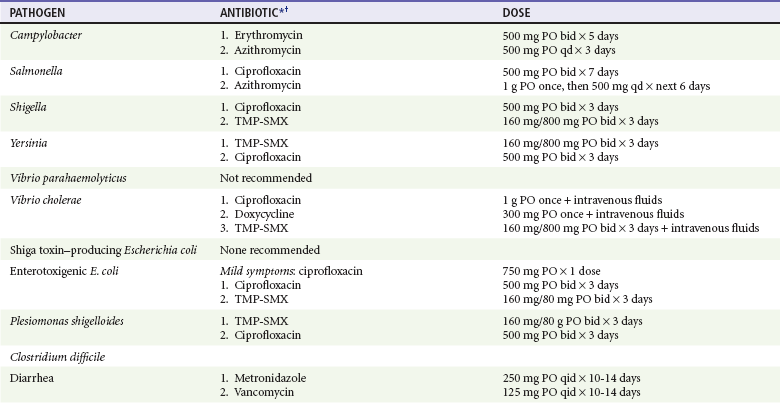
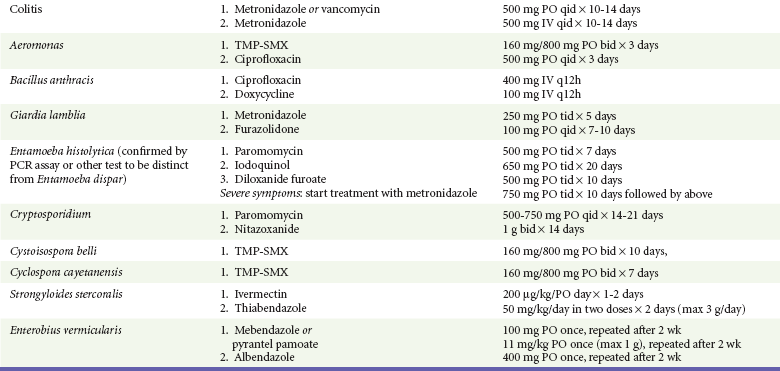
Chapter 94 Gastroenteritis is defined as an inflammation of the stomach or intestines resulting in some combination of nausea, vomiting, and diarrhea. Although most affected patients will prove to have an infectious cause for their symptoms, the clinician also should consider noninfectious causes of vomiting and diarrhea, which are considered in detail in Chapters 29 and 31, respectively. Infectious gastroenteritis is associated with dozens of causative pathogens. Most of these organisms cause benign and self-limited illness, but in a few cases the morbidity may be significant, necessitating prompt diagnosis and treatment. Diagnostic testing should be targeted to those patients who have clinically significant illness or suspected reportable disease. It is neither feasible nor necessary to identify the specific pathogen during the emergency department (ED) evaluation. Instead, the clinician should classify the gastroenteritis as acute or chronic and invasive or noninvasive, based on readily available clinical information. This classification narrows the differential diagnosis considerably and is a valuable guide to further testing. Potential pathogens in acute invasive bacterial enteritis are summarized in Table 94-1. Campylobacter is the most common documented cause of bacterial enteritis in developed countries. In a Swedish study of 100,000 persons, Campylobacter was isolated in 56% of cases of enteritis. Worldwide, Campylobacter accounts for up to 14% of cases of acute infectious diarrhea.1 In the United States, the Foodborne Diseases Active Surveillance Network (FoodNet) estimated the 2009 incidence to be 13 cases per 100,000 population.2 Most cases occur in children younger than 5 years or in male patients aged 20 to 29 years, but people of all ages are affected. The disease is more common during the summer months. Campylobacter species are a common cause of “backpacker’s diarrhea,” along with Giardia, both of which are frequently acquired by drinking from wilderness water sources. Campylobacter organisms are small, spiral-shaped gram-negative bacteria. The most common species isolated are Campylobacter jejuni (94%), Campylobacter coli (1%), and Campylobacter fetus.1 Campylobacter species produce disease primarily by direct invasion of the colonic epithelium and may induce inflammatory changes that are endoscopically indistinguishable from inflammatory bowel disease. Most infections are acquired by handling raw poultry or eating raw or undercooked poultry meat. The primary reservoirs for Campylobacter organisms are chickens, with more than one half of U.S. flocks silently infected and approximately one half of the chicken in U.S. supermarkets contaminated.2 Other causes include consumption of tainted beef, pork, raw milk, or untreated water and contact with infected pets (particularly cats and puppies) and farm animals.2 The incubation period for Campylobacter enteritis is approximately 2 to 5 days. Disease onset usually is rapid, with signs and symptoms of fever, cramping abdominal pain, and diarrhea. Constitutional symptoms of anorexia, malaise, myalgias, and headache are the rule, and some patients experience backache, arthralgias, and vomiting. The clinical picture can mimic that in acute appendicitis. Onset of diarrhea often lags 24 to 48 hours after the onset of fever and abdominal pain. Typically the stools are loose and bile-colored but then become watery, grossly bloody, or melanotic approximately 40% of the time. Either gross or occult blood is found in the stool of 60 to 90% of patients with Campylobacter gastroenteritis. At the height of the illness, patients usually pass 8 to 10 stools or more per day.3 Most patients are well within a week or less; however, diarrhea can persist for weeks. Relapses are common, although generally milder than the original episode. Fatalities are rare; the Centers for Disease Control and Prevention (CDC) estimates 124 fatal cases in the United States each year.2 Because the clinical presentation is similar to that with other invasive bacterial pathogens, the diagnosis of campylobacteriosis cannot be made on the basis of clinical presentation alone. Identification of the pathogen will require stool culture or real-time polymerase chain reaction (PCR); specimens should be obtained from patients with acute enteritis associated with fever, abdominal pain, occult blood, or hematochezia. In borderline cases, stool methylene blue stain for fecal leukocytes is readily available and may help identify those patients who are likely to harbor an invasive pathogen. One study of outpatients with acute diarrhea found that the presence of fecal leukocytes (more than five white blood cells per high-power field) was associated with a likelihood ratio (LR) of 5.0 for the presence of an invasive pathogen (95% confidence interval [CI], 2.9 to 8.6).4 Blood culture results are rarely positive, so these studies are not routinely indicated. Sigmoidoscopy reveals a nonspecific inflammatory colitis, and Campylobacter infection should be considered before a new diagnosis of inflammatory bowel disease is made. Empirical antibiotic therapy is not recommended for otherwise healthy patients with acute invasive diarrhea. (Travel-related diarrhea is an exception; see later). Initial treatment of invasive diarrhea should focus on rehydration, and the decision to initiate antibiotic therapy should be deferred pending identification of a specific organism via stool studies. Treatment with antibiotics is not needed for patients who demonstrate clinical improvement by the time results become available. For those who are not improving, antibiotic therapy shortens the duration of campylobacteriosis by approximately 1.3 days.5 Erythromycin 500 mg twice a day for 5 days is the recommended first-line therapeutic regimen. Azithromycin 500 mg daily for 3 days is acceptable as well. Ciprofloxacin 500 mg twice a day can be used and was previously the treatment of choice, but alarming resistance to the fluoroquinolones has emerged, thought to be mainly a result of antibiotic use in the poultry industry, which was halted by the U.S. Food and Drug Administration (FDA) in 2005. Roughly 20% of Campylobacter strains are now resistant in the United States, and resistance of more than 80% has been documented in Thailand. Campylobacter organisms generally also are resistant to trimethoprim-sulfamethoxazole (TMP-SMX). Suggested antibiotic regimens for treatment of diarrhea are listed in Table 94-2. Relapses can occur, but the likelihood is decreased with appropriate antibiotic treatment.3 Because Campylobacter infection causes an invasive enteritis, antimotility agents are not recommended unless treatment with antibiotics also is given. Table 94-2 Antibiotic Therapy for Diarrhea in Immunocompetent Adults PCR, polymerase chain reaction; PO, orally; TMP-SMX, trimethoprim-sulfamethoxazole. *Another quinolone agent, norfloxacin, can be substituted for ciprofloxacin in the treatment of diarrheas. The equivalent dosage is 400 mg bid. †Listed drugs are numbered in order of preference: 1 indicates the drug of first choice; 2 and 3 indicate alternative drugs. Complications of Campylobacter infection are rare. Cholecystitis, pancreatitis, and massive gastrointestinal bleeding all have been documented, as have meningitis, endocarditis, and osteomyelitis. In addition, a definite association has been made with Guillain-Barré syndrome. Guillain-Barré syndrome associated with Campylobacter infection tends to be more severe than Guillain-Barré syndrome from other triggers and can occur even with asymptomatic infections. Luckily, the incidence is estimated at less than 1 per 1000 cases.2 Salmonella is the most common cause of documented bacterial enteritis in the United States, with approximately 40,000 documented cases reported to the CDC per year and an estimated 15 cases per 100,000 population.6 U.S. surveillance systems found a 12% decrease in documented Salmonella infections in 2005 compared with 1995. Enteritis caused by this organism affects people of all age groups but particularly children, with those younger than 5 years accounting for 20% of cases.7 Almost all Salmonella infections are acquired from ingestion of contaminated food or drink. Direct person-to-person transmission can occur, but most human infections are related to the vast reservoir of salmonellae in lower-order animals. Poultry products and beef constitute the most common sources of Salmonella. Unpasteurized milk, eggs, fish, and domestic pets are other sources. Outbreaks also have been associated with consumption of fruits, vegetables, baked goods, rattlesnake meat, and medicinal preparations. Approximately 10% of household dogs and cats excrete salmonellae, and pet reptiles, such as turtles, snakes, and iguanas, have been responsible for outbreaks of salmonellosis.7 Cooking contaminated foods decreases the possibility of infection but does not eliminate it. Salmonellae can survive cooking deep inside certain foods, where temperatures may not reach the lethal range. Very large outbreaks of Salmonella infection have been traced to contaminated, unbroken, grade A eggs.7 Although the organism is present in the uncracked egg, thorough cooking usually eradicates or reduces the inoculum to clinically insignificant levels. Common raw egg–based sources of Salmonella infections include homemade hollandaise sauce, eggnog, Caesar salad dressing, ice cream, mayonnaise, tiramisu, cookie dough (often consumed unbaked), frosting, and French toast mix.7 Salmonella enterica subsp. enterica serovar Enteritidis (i.e., “S. Enteritidis”) is the species universally associated with egg-related infections. Patients convalescing from Salmonella-related enterocolitis and persons with asymptomatic infection may continue to excrete Salmonella organisms for weeks or months, thus serving as ongoing sources of infection.7 Approximately 2000 Salmonella serotypes are known to cause human illness. Based on 2010 U.S. surveillance figures, the most common isolates are the S. enterica serovars Typhimurium, Enteritidis, and Newport, which together account for approximately half of culture confirmed serotypes.7 Different Salmonella serotypes show marked variations in invasive potential and are associated with particular presentations: S. enterica serovar Typhi with enteric fever (typhoid fever), S. enterica serovar Choleraesuis with septicemia, S. enterica serovar Typhimurium with acute gastroenteritis, and S. enterica serovar Enteritidis infections from grade A shell eggs.7 Rates of invasive infection and disease severity are increased in infants, elders, and people with hemoglobinopathies such as sickle cell anemia, malignant neoplasms, or acquired immunodeficiency syndrome (AIDS).7 The CDC estimates that more than 400 fatal cases occur each year.7 Family outbreaks and sporadic cases are more common than large epidemics. Ingested salmonellae penetrate the intestinal mucosal cells and lodge in the lamina propria. After an incubation period of 8 to 48 hours, the typical patient with Salmonella gastroenteritis develops fever, colicky abdominal pain, and loose, watery stools, occasionally containing mucus and blood. Nausea and vomiting are common but rarely are severe or protracted. Mild to moderate diffuse abdominal tenderness can be elicited in most patients, but severe tenderness and even rebound tenderness may occasionally be noted. Symptoms usually abate within 2 to 5 days, and recovery typically is uneventful. Sustained or intermittent bacteremia may occur, especially in those with sickle cell anemia, malignancy, or AIDS. Focal infections are identified in 10% of those with Salmonella bacteremia.8 Empirical antibiotic therapy is not recommended for otherwise healthy patients with suspected Salmonella enteritis. Antibiotic therapy does not shorten the duration of the disease and may prolong the duration of the carrier state. Although its effectiveness is unproven, antibiotic therapy is recommended for patients with severe colitis and for infants younger than 3 months, adults older than 50 years, and individuals at risk for severe disease including the immunocompromised, those with sickle cell disease, and those with prosthetic grafts. Persons who represent a public health risk also should be treated in an attempt to eradicate the carrier state and prevent spread of the organism.3,7 The choice of antibiotic should be based on sensitivities of the isolate. Any of the following antibiotic regimens typically is effective for outpatient management of Salmonella gastroenteritis: ciprofloxacin 500 mg twice a day for 5 to 7 days, norfloxacin 400 mg twice a day for 5 to 7 days, or azithromycin 1 g by mouth and then 500 mg a day for the next 6 days.3 TMP-SMX also can be used if the organism is susceptible. Ciprofloxacin is effective in the treatment of chronic S. Typhi carriers. However, treatment with fluoroquinolones can actually prolong shedding of non-Typhi organisms. Patients requiring hospitalization are best treated with intravenous ceftriaxone until results of sensitivity studies become available.3 Prevention of salmonellosis depends on adequate cooking and minimizing the time that foods are allowed to stand at room temperature to reduce the chance of bacterial growth to an infectious inoculum. Careful personal hygiene, including handwashing, also is important. Salmonella infection is a nationally notifiable disease (Box 94-1). Although most patients recover fully without long-term sequelae, up to 30% (primarily adults) will experience transient reactive arthritis. Reiter’s syndrome, consisting of reactive arthritis, conjunctivitis, and urethritis, is a well-known complication and occurs in approximately 2% of patients.8 Shigellosis, or bacillary dysentery, is worldwide in distribution and particularly common in countries lacking effective sanitation. In the United States, approximately 14,000 laboratory-confirmed cases occur annually, representing an estimated rate of 44 cases per 100,000 population.6,9 The CDC estimates that there are actually approximately 450,000 cases each year.10 Shigella sonnei is responsible for approximately 75% of the infections occurring in the United States. Shigella flexneri causes most of the remaining cases, with Shigella boydii and Shigella dysenteriae responsible for less than 4% of cases.11 Shigella infections are common in confined populations, such as those in mental or penal institutions, in nursing homes or daycare centers, or on Native American Indian reservations. Children younger than 5 years account for 30% of cases. An increased incidence has been documented among men who have sex with men and in the AIDS population.9 Spread is by the fecal-oral route, and humans are the only natural hosts. Shigellae can be found in large numbers around the base of toilets used by infected persons, and the organism readily passes through toilet tissue onto the fingers. Shigellae can be recovered in cultures of samples taken as long as 3 hours after contamination. In the last few years, a number of large outbreaks have been associated with recreational water venues such as swimming pools, water parks, fountains, hot tubs, and spas.10 Clinical presentation varies among Shigella species. S. sonnei typically causes high-volume, watery diarrhea with relatively few systemic signs. Infection with S. flexneri, S. dysenteriae, or S. boydii typically causes low-volume bloody diarrhea and more severe systemic symptoms.11 The usual incubation period is 24 to 48 hours, and the clinical manifestations vary considerably, often appearing in a bimodal fashion. Mild, watery diarrhea with few if any constitutional symptoms or asymptomatic infection occurs in a significant proportion of infected persons. It is estimated that fever occurs in 58% to 100%, abdominal pain in 75% to 100%, tenesmus in 55% to 96%, bloody stool in 46% to 73%, and nausea or vomiting in 63% to 100%.3 Fecal white blood cells are present, usually in large numbers, in 85 to 95% of the cases, regardless of the gross appearance of the stool.3 Thus, finding leukocytes in watery stools can help identify shigellosis even in the absence of classic dysenteric stools. Occult blood usually is present in the stools of infected patients. Blood leukocytosis is common, and a significant leftward shift in the differential count is almost always seen. Results of blood cultures for Shigella are rarely positive. Sigmoidoscopic examination reveals diffuse mucosal inflammation, often with multiple ulcerations. A definitive diagnosis of shigellosis is made with stool culture or real-time PCR. Stool culture results are positive in more than 90% of cases when samples are obtained during the first 3 days of illness; however, results are positive in only approximately 75% if samples are obtained more than 1 week after the onset of diarrhea.11,12 Treatment primarily involves the correction of fluid and electrolyte abnormalities. If S. sonnei or S. flexneri is cultured from the stool, the decision to administer antibiotics is based on the patient’s clinical condition and the feasibility of sanitary control. Asymptomatic or recovering patients do not need to be treated with antibiotics unless treatment is necessary for public health measures. Patients whose condition is not improving and those who are immunocompromised should be treated. Antibiotics shorten the clinical course and eradicate the pathogen from the stool, often within 48 hours.11,12 Whenever S. dysenteriae is isolated, the patient should be treated to prevent outbreaks of dysentery, even if the patient is asymptomatic when the culture result returns from the laboratory. In the United States, more than 80% of Shigella organisms are resistant to ampicillin, and 47% are resistant to TMP-SMX.7,11 Significant resistance has not yet been found to the quinolone agents ciprofloxacin and norfloxacin, and one of these should be considered the drug of choice unless sensitivity studies demonstrate that the organism is sensitive to either ampicillin or TMP-SMX. Treatment is required for only 3 days in immunocompetent patients but should be extended to 7 to 10 days in the immunocompromised.3 Complications are rare and include bacteremia, Reiter’s syndrome (after S. flexneri infection), HUS (after S. dysenteriae infection), toxic megacolon, colonic perforation, seizures, and toxic encephalopathy.11 Y. enterocolitica, a gram-negative facultatively anaerobic bacterium, is a member of the family Enterobacteriaceae. Y. enterocolitica is a relatively infrequent cause of enteritis in the United States, with FoodNet surveillance systems documenting approximately one case of culture-verified yersiniosis per 100,000 population.13 Y. enterocolitica infections are the third most common notifiable bacterial zoonoses throughout Scandinavia and Europe behind campylobacteriosis and salmonellosis. Between 2002 and 2008 the annual number of confirmed cases of yersiniosis fell from 9.2 to 5.3 cases per 100,000 population Germany.14 Yersiniosis is more prevalent in children and is fairly evenly distributed throughout the calendar year. After oral ingestion, the bacterium invades the intestinal epithelium and localizes to lymphoid tissue of the intestinal mucosa, particularly Peyer’s patches. It then invades the regional mesenteric lymph nodes. Invasive enteritis is the clinical presentation in approximately two thirds of patients. Pseudoappendicitis and mesenteric adenitis account for the remainder of presentations. Infection originates from contaminated food or drink. The consumption of contaminated milk or contaminated raw pork has accounted for sporadic cases and several large outbreaks. Fecal-oral transmission to humans from a variety of animals, particularly dogs, cats, and pigs, and direct person-to-person spread probably occur, but communicability appears to be low.13 The clinical picture with Yersinia enterocolitis often resembles that with infection by other invasive intestinal organisms: fever (68%); colicky abdominal pain (65%); watery, greenish, and sometimes bloody (26%) diarrhea; and constitutional symptoms of anorexia, vomiting (39%), and malaise.3 However, in cases of Y. enterocolitica gastroenteritis, the abdominal pain and diarrhea usually persist for 10 to 14 days or longer. In a substantial number of patients with yersiniosis, particularly adolescents and young adults, an ileocecitis may develop. In these cases, lower abdominal pain with little or no diarrhea is the predominant symptom, and the clinical presentation may perfectly mimic that of acute appendicitis. Historically, large outbreaks have been traced to contaminated milk, largely because in the relevant series, physicians noticed an extraordinary rise in the number of negative appendectomies. With modern food processing techniques, almost all cases are now reported as isolated events.13,14 Postinfection manifestations, such as erythema nodosum or a persistent polyarthritis, occur in 2 to 5% of patients, mainly adults. Other presentations include sacroiliitis, ankylosing spondylitis, Reiter’s syndrome, exudative pharyngitis, pneumonia, empyema, and lung abscess. Y. enterocolitica septicemia is rare but is known to occur, most often in patients with diabetes mellitus, severe anemia, hemochromatosis, cirrhosis, or malignancy.15 Approximately 70% of patients with Y. enterocolitica infection have signs and symptoms of invasive enteritis. The diagnosis of yersiniosis cannot be made on the basis of clinical presentation; a positive stool culture or real-time PCR is required. Methylene blue staining of stool for fecal leukocytes yields a positive result in approximately 48% of cases of yersiniosis.3 Most laboratories do not routinely include Y. enterocolitica in the standard stool testing; Yersinia identification can be done by special request if clinically indicated (e.g., by history of Yersinia exposure, prolonged invasive enteritis despite a negative result on standard stool culture, or right lower quadrant pain with a normal appendix on imaging studies). Treatment with antibiotics has not been proved to be essential or efficacious in the management of uncomplicated Yersinia enterocolitis or in the pseudoappendicitis syndrome. However, because Yersinia organisms take a long time to grow on culture, in most studies the duration of illness before antibiotics were started was 1 to 2 weeks. Yersinia organisms usually are susceptible to TMP-SMX, which is the agent of choice when antibiotic therapy is indicated.3 Drug treatment does decrease the fecal shedding of the organism. Doxycycline in combination with an aminoglycoside is an alternative regimen, as is single-agent therapy with a quinolone.3 In immunocompetent adults, a 3-day course is sufficient; the course is extended to 7 to 10 days if the patient is immunocompromised. Treatment should be considered in patients who are still significantly ill at the time stool results return, particularly if the patients are immunocompromised or have a significant underlying medical illness, or in cases in which the fecal shedding could represent a public health hazard. In patients who interact with potentially susceptible persons, appropriate steps should be taken to ensure that they do not spread their infection. V. parahaemolyticus is a halophilic (salt-requiring) gram-negative bacillus found naturally in warm marine environments such as the coastal seawaters of Japan, the United States, and other temperate-zone nations. In Japan, V. parahaemolyticus is the most common cause of bacterial enteritis, being responsible for approximately 70% of cases. The typical source is raw fish. In the United States, V. parahaemolyticus disease is much less common, though it has increased approximately 85% over the past 10 years to approximately 215 documented cases annually, or 0.35 per 100,000 population. The CDC estimates that approximately 4500 cases, 30 hospitalizations, and 1 or 2 deaths occur each year. Cases in the United States typically are related to consumption of raw or undercooked shellfish, especially oysters (49%), although clams (38%), shrimp, lobsters, mussels, cockles, crabs, and scallops all have been implicated. Many cases occur as outbreaks on cruise ships or in persons who have patronized a common restaurant or seafood market. V. parahaemolyticus enteritis is much more common in the summer months, with 70% of cases occurring in the months of May to October, when warm seawater temperatures favor replication of the organism.16 At such times, 100% of oysters in local beds have been shown to harbor the organism. Attack rates from a common-source exposure are fairly high, but little evidence is available for human-to-human spread among family members of infected patients.16 The mechanism by which V. parahaemolyticus causes human enteritis is incompletely understood but seems to be related to production of two thermostable direct hemolysin (TDH) virulence factors. Serotypes that produce one or both virulence factors attach to the colonic epithelium and induce a secretory diarrhea as well as local cell lysis. An infectious dose of V. parahaemolyticus is thought to be 100,000 colony-forming units (CFUs) or more. Still, transmission has occurred from oyster beds in which the colony count was less than 200 CFUs per gram of oyster meat.17 Although enteritis is the most common clinical presentation, accounting for 60 to 80% of cases, V. parahaemolyticus infections also manifest as wound infections (34%) and septicemia (5%).6,18,20 Serious wound infections and septicemia occur primarily in persons with underlying liver disease, alcoholism, or diabetes mellitus.15,17 Signs and symptoms usually appear 8 to 12 hours after the ingestion of contaminated food, but the incubation period can range from 4 to 48 hours. The predominant manifestation is acute diarrhea, but the volume of fluid lost generally is not large. Moderately severe abdominal cramps occur in 88%, nausea in 52%, vomiting in 39%, and fever in 33%. Vomiting generally is not prominent. The illness is almost invariably self-limited and seldom lasts longer than 24 to 48 hours.17 As with other types of acute invasive enteritis, the diagnosis of V. parahaemolyticus cannot be made on the basis of clinical presentation alone. The diagnosis is made by stool culture or real-time PCR. Although blood agar and other nonselective media support the growth of this species, isolation from the stool usually requires the use of a selective medium containing thiosulfate, citrate, bile salts, and sucrose (TCBS agar). This selective culture procedure is not part of the standard stool culture in most U.S. hospitals but can be obtained by special request in cases of outbreaks related to consumption of raw or undercooked shellfish, especially in coastal areas of the United States.16,17 Because the disease is self-limited, most patients require no therapy. Although data on efficacy of antibiotic therapy are lacking, patients who still have diarrhea when culture results become available may benefit from treatment with tetracycline, fluoroquinolones, or ceftriaxone or another antibiotic as guided by susceptibility testing.15,17 An occasional patient may require fluid replacement. Antimotility agents are not indicated. Enterohemorrhagic E. coli was first recognized as a human pathogen in 1982 after two outbreaks of hemorrhagic colitis were traced to undercooked ground beef contaminated with E. coli serotype O157 : H7 and distributed at a fast food restaurant chain. It is now recognized that E. coli O157 : H7 is one of more than 30 serotypes of E. coli known to produce Shigella-like toxins and that these STEC serotypes as a group constitute a major cause of hemorrhagic colitis, HUS, and thrombotic thrombocytopenic purpura (TTP) in humans.15 The CDC estimates 110,000 cases and 3200 hospitalizations per year in the United States and reports a 41% decrease in the incidence from 1998 to 2009, probably a result of improvements in food safety protocols.18–20 STEC infections have been documented in more than 30 countries on six continents. Children younger than 10 years are at greatest risk for serious STEC infection. Approximately 15% of children with STEC diarrhea develop HUS.20 Inadequately cooked hamburger has caused many large outbreaks.15,18 STEC, present in the intestines of healthy cattle, contaminates the meat during slaughter, and the grinding process then transfers the organisms from the surface of the meat to the interior. The infectious dose is low, approximately 100 bacteria. U.S. Department of Agriculture food safety regulations now require that hamburger be cooked to an internal temperature of 70° C (160° F) to effectively kill E. coli organisms. Outbreaks also have occurred from consumption of venison, salami, pepperoni, cured mutton sausage, cheese curds, apple cider, raw milk, uncooked cookie dough, and fruits and vegetables; from contamination of municipal water supplies; from animal contact in petting zoos; and from person-to-person spread in daycare centers.8,20 Food handlers with STEC-related diarrhea have contaminated meals, causing institutional outbreaks. STEC enteritis is more common in the summer months. Ingested STEC multiply in competition with normal bacterial enteric flora, adhere to the intestinal epithelial cells, and elaborate Shiga toxin. Toxins bind to absorptive enterocytes on the luminal surface of the small and large intestine, enter the cell, and irreversibly inhibit protein synthesis, resulting in death of enterocytes. Shiga toxins can then enter the bloodstream via damaged intestinal epithelium and cause death of vascular endothelial cells by the same mechanism. Endothelial cell lysis is accompanied by platelet activation and aggregation, cytokine secretion, vascular constriction contributing to fibrin deposition, and clot formation within the capillary lumen. Microangiopathy propagates distally as the toxins are carried to the kidneys, causing the clinical syndrome of hematuria and renal failure (HUS).20 The development of HUS is associated primarily with serotypes that produce Shiga toxin 2. The CDC estimates that 90% of U.S. cases of HUS are caused by E. coli O157 : H7. After an incubation period of 3 to 4 days, patients initially produce watery diarrhea that becomes bloody hours to days later. Approximately 90% of patients report bloody stools.20 The amount of blood varies, but stools passed may appear to consist wholly of blood, and the infection may masquerade as gastrointestinal bleeding from noninfectious causes. The bloody diarrhea typically is accompanied by severe abdominal cramps, pain, and often vomiting. Fever is a feature in fewer than one third of cases and, if present, usually is low grade.8 This helps differentiate STEC infection from infection with other invasive organisms. Fecal leukocytes are found in approximately 50% of cases, but in small numbers, in contrast with the sheets of white blood cells seen in Shigella dysentery.3 Endoscopic, histologic, and radiographic studies demonstrate only nonspecific changes consistent with an inflammatory hemorrhagic colitis and do not accurately distinguish STEC infection from other causes of colitis.20 STEC colitis has been associated with two serious complications: HUS and TTP. These clinically similar disorders share the following features: microangiopathic hemolytic anemia, thrombocytopenia, fever, neurologic deficits, and renal dysfunction. In TTP, neurologic findings predominate, and renal dysfunction is unusual. The opposite is seen with HUS, which is more common in children, especially those younger than 4 years, occurring in approximately 15% of cases.8,18,20 Of these, approximately 5% are fatal.18 Approximately 22 to 40% of elders in nursing home outbreaks acquire HUS, and 50 to 80% of these patients die. TTP is seen in 2 to 3% of cases, most often in immunosuppressed patients. HUS and TTP typically appear 5 to 20 days after the onset of infection, and the diarrhea can be totally resolved and forgotten by the time a diagnosis is established. Death from STEC colitis alone or from one of the complications occurs primarily among elders.15 The CDC recommends that all stools submitted for routine testing from patients with acute community-acquired diarrhea (regardless of age, season, or presence or absence of blood in the stool) be simultaneously cultured for E. coli O157 : H7 and tested with an assay that detects Shiga toxins to detect non-O157 STEC.21 Culture-based diagnosis requires specific stool culture techniques. In addition to the routine battery of media, specimens should be plated onto sorbitol-MacConkey (SMAC) medium. The O157 : H7 strains of E. coli are sorbitol negative at 18 to 24 hours of growth on this medium and can be rapidly identified with various serologic tests, such as latex agglutination or fluorescent antibody testing. A commercial Shiga toxin enzyme immunoassay (EIA) was introduced in 1995 to assist clinical laboratories in identifying non-O157 Shiga toxin–producing strains of E. coli. The CDC now recommends that all stools submitted for culture also be tested for STEC-associated verotoxin with use of commercially available immunoassays, and that non-O157 STEC be sent to the CDC for typing. Antibiotic therapy does not shorten the clinical course or eradicate the organism. Moreover, treatment with antibiotics to which the organism is resistant may increase the risk for HUS by eliminating competing bowel flora. However, the degree to which antibiotic treatment truly increases the risk for HUS remains controversial.3,8,18 Retrospective studies in adults suggest an association between antibiotic use and the development of HUS but may have been biased by preferential use of antibiotics in the more serious cases. Because antibiotic treatment is of no clinical benefit and may increase the risk of HUS, it is not recommended for patients with known infection with E. coli O157 : H7. Aeromonas organisms are gram-negative, facultatively anaerobic, rod-shaped bacteria of the family Aeromonadaceae. Aeromonas species are ubiquitous worldwide in fresh and brackish water and also contaminate the food and water supply.15,22 Aeromonas organisms grow at a range of temperatures but are isolated with increased frequency in summer months. Aeromonas infection is not a reportable condition in the United States or most other countries worldwide. No figures are available on the incidence of Aeromonas gastroenteritis in the United States. An association with human enteritis is difficult to confirm for several reasons. No major clonally related outbreaks have been linked to Aeromonas species, and the organism often is found in the feces of asymptomatic persons. In addition, a number of “suspected” Aeromonas outbreaks related to seafood (prawns, oysters, shrimp, and sashimi) and fish have been associated with incubation periods of less than 24 hours, which is not characteristic of Aeromonas. Despite many attempts, Aeromonas has failed to fulfill Henle-Koch requirements for a human pathogen—that the pathogen be fully isolated from the body, grown in pure culture, and capable of inducing disease when reintroduced to the human body.22 Still, several small outbreaks have been documented in travelers and by case-control studies; it is thought that certain serotypes do cause gastroenteritis in humans.22,23 Drinking untreated water, usually from private wells or springs, is thought to cause most cases of diarrhea from Aeromonas bacteria.22 Although bivalves such as oysters and mussels concentrate Aeromonas in their meats during the filter-feeding process, Aeromonas infection has not been definitively associated with consumption of shellfish. Aeromonas hydrophila causes wound infection; septicemia occurs in persons of advanced age or with underlying gastrointestinal disease such as colon cancer, cirrhosis, or hepatobiliary or inflammatory bowel disease or history of recent hospitalization or antibiotic treatment. In some published series, Aeromonas infection causes 2 to 10% of all cases of diarrhea in children.22,23 Aeromonas enteritis is thought to have five distinct clinical presentations. By far the most common, occurring in approximately 75 to 89% of cases, is as a secretory (watery) diarrheal syndrome. A more severe form can be accompanied by bloody stools, similar to infection with the invasive pathogens mentioned earlier. Aeromonas infection also manifests as traveler’s diarrhea or, rarely, a cholera-like syndrome with loss of 10 or more L of diarrheal fluid per day. Subacute and chronic enteritis syndromes have also been described, with symptoms lasting from months to years.22 Stool should be examined for the presence of Aeromonas infection before a diagnosis of inflammatory bowel disease is established. No controlled trials have been conducted that clearly demonstrate a benefit to antibiotic therapy. In most patients, Aeromonas enteritis is mild and self-limited, and antibiotic therapy probably is not warranted. In the case of severe disease, prolonged diarrhea, or an immunocompromised host, susceptibility testing supports the use of quinolones, aminoglycosides, carbapenems, cephalosporins, macrolides, nitrofurans, or tetracycline.22 P. shigelloides is a gram-negative, facultatively anaerobic bacterium of the family Enterobacteriaceae. The organism is found in a variety of settings, including animals, soil, and freshwater and dilute saltwater bodies, including the Gulf of Mexico. Humans usually are infected by contaminated food or water or after contact with colonized animals. Worldwide, P. shigelloides enteritis is well documented in the tropical and subtropical areas of Africa, Asia, and Australia. In the United States and Europe, most cases occur after travel to tropical areas or after consumption of raw shellfish, especially oysters.15 Sporadic diarrheal illness occurs in both normal and immunocompromised hosts. Large outbreaks have occurred, usually resulting from oyster consumption.15 The incubation period is only 1 to 2 days. The infectious dose is thought to be high, over 1 million organisms. Abdominal pain is noted in 72% of patients. Diarrhea is watery in 73% of patients and grossly bloody in 24%. Occult blood is noted in 44%, emesis in 38%, and fever in 51%.24 Symptoms resolve after 1 to 3 days in most cases but occasionally may persist for up to 8 weeks. The duration of illness usually is shorter in children. Antibiotic therapy usually is not necessary for P. shigelloides enteritis because of the brief duration of illness. In patients who are immunocompromised and those with severe or prolonged symptoms, antibiotic treatment may be of benefit. P. shigelloides usually is resistant to ampicillin but susceptible to TMP-SMX, quinolones, cephalosporins, and chloramphenicol. The current recommended treatment regimen is TMP-SMX 160 mg/800 mg twice daily for 3 days; ciprofloxacin 500 mg twice daily; or norfloxacin 400 mg twice daily for 3 days.3 Follow-up evaluation is not necessary unless the patient is immunodeficient or does not respond clinically. Although gastrointestinal anthrax is rare in developed countries, large outbreaks still occur in agricultural regions throughout the world. Anthrax also has been used as a weapon of bioterrorism in regions not normally susceptible to the disease. As early as the 1930s, groups experimented with anthrax-impregnated chocolate as a weapon against their enemies. Awareness of the spectrum of clinical presentations of gastrointestinal anthrax is important not only for the welfare of the patient but for prompt recognition of potential terrorist activity.25 Traditionally, gastrointestinal infection has been estimated at less than 1% of all human anthrax cases. It was thought that 95% of cases involved cutaneous symptoms and 5% were limited to the respiratory tract. However, because gastrointestinal anthrax can cause only mild and self-limited symptoms and occurs in underserved areas, many persons with the gastrointestinal form may not seek medical treatment. Studies of several large outbreaks in Uganda and Thailand suggest that the gastrointestinal form is observed in 74 to 92% of patients who contract anthrax after having eaten the meat of infected herbivores.25 Areas endemic for anthrax exist in all continents containing tropical and subtemperate regions. Thailand, India, Iran, Gambia, and Uganda all have reported deaths from gastrointestinal anthrax.25 Within the United States, naturally occurring anthrax exposure has been documented in several areas, including Minnesota.25 Although no predilection for time of year in endemic areas has been documented, the disease is more common in animals after substantial rainfall following a period of drought, a pattern known as “anthrax weather.”26 In the United States, gastrointestinal anthrax has not been reported, although cutaneous anthrax is reported once or twice each year.27 Populations at risk for naturally occurring anthrax are persons living in rural, agricultural areas who have ingested undercooked meat contaminated with anthrax spores. As with many other organisms, the pediatric population seems to be at greatest risk for serious or fatal illness. When swallowed, anthrax spores stick to the gastrointestinal epithelium, where they germinate and create multiple superficial ulcerations. Lesions have been identified from the oral cavity to the cecum.25 The vegetative cells may at times migrate into the bloodstream, where they rapidly multiply and can cause septicemia. B. anthracis protects itself with an antiphagocytic capsule and produces two exotoxins, lethal and edema toxins.25 A minority of patients who ingest anthrax spores remain asymptomatic, and in endemic areas, adults often are thought to have some natural immunity acquired through previous exposure. Of those in whom symptoms do develop, presentation can vary widely, ranging from mild watery diarrhea to fulminant upper and lower gastrointestinal bleeding, septicemia, and death. The incubation period for gastrointestinal symptoms ranges from 1 to 6 days, developing earlier with larger inocula and more severe disease. For disease confined to the oropharynx, patients usually have complaints of sore throat, fever, dysphagia, hoarseness, and painful neck swelling. The swelling results from marked lymphadenopathy and tissue edema and can become severe enough to compromise breathing.27 Much information concerning intestinal anthrax has been derived from two large outbreaks in Uganda and Thailand.25 A majority of the patients had isolated diarrhea. Nausea, vomiting, and severe abdominal pain with distention also developed in a minority of the patients. Most patients were febrile, with temperatures above 39° C (102° F) and blood in both the vomitus and diarrheal stool was common. In cases of primary gastrointestinal anthrax, the superficial mucosa is always involved, with ulcerations visible on endoscopic examination. These findings are in contrast to those with disseminated infection from pulmonary anthrax, in which the lesions begin submucosally as a result of seeding from the bloodstream. These lesions can then secondarily ulcerate to the surface of the gastrointestinal tract epithelium. Untreated, gastrointestinal anthrax may last weeks and is fatal in over 50% of patients. Appropriate treatment results in a mortality rate less than 40%.27 Diagnosis of the gastrointestinal variant of anthrax relies more on identifying B. anthracis DNA by PCR assay and cultures of blood and, if possible, ascitic fluid. Stool or rectal swab should be obtained for culture and PCR as well.28 Traditionally, penicillin has been used to treat gastrointestinal anthrax. Cases of penicillin resistance have been documented, however, and a logical assumption is that a resistant strain would be chosen for use as a weapon of bioterrorism. Therefore, current recommendations from the CDC are to treat gastrointestinal cases in the same manner as cases of respiratory anthrax, with ciprofloxacin 400 mg intravenously (IV) every 12 hours or doxycycline 100 mg IV every 12 hours. Cephalosporins should not be used. Even with aggressive antibiotic therapy, the disease carries a 25 to 60% mortality rate, depending on treatment, host factors, and the size of the inoculum.28 Pathogens associated with toxin-induced bacterial enteritis are summarized in Table 94-3. In general, gastroenteritis caused by toxin-forming bacteria and viral agents will manifest as an acute noninvasive enteritis, with watery diarrhea, minimal fever, little or no abdominal cramping, and absence of fecal leukocytes and erythrocytes. Treatment is primarily supportive, and diagnostic testing generally is not indicated in otherwise healthy patients. A specific diagnosis may be of help in attempting to identify a common source during large outbreaks. Staphylococcus-related food poisoning occurs after multiplication of an enterotoxin-forming strain of Staphylococcus that is present in the food before ingestion. Food contamination with Staphylococcus is extremely common because the organism is ubiquitous in the environment. It can be isolated from the skin, hair, throat, and nasal passages of approximately 50% of persons in the general population. Most protein-rich foods support the growth of staphylococci, especially ham, eggs (even hard boiled), custard-filled pastries, mayonnaise, milk, and salads such as egg, tuna, chicken, potato, and macaroni.29 Foods that require considerable handling during preparation and are then kept slightly warm after preparation are frequent offenders. Temperatures of 45 to 140° F for only a few hours will allow proliferation of the organism in contaminated food and production of sufficient enterotoxin to cause disease. Foods containing sufficient enterotoxin to produce violent illness usually are normal in appearance, odor, and taste. Large outbreaks are common worldwide, particularly in institutions such as school or hospital cafeterias, military bases, airlines, and restaurants.29 Although the bacterium itself is killed by cooking at temperatures above 140° F, Staphylococcus enterotoxin is heat stable. Thus once it is present in food, reheating or even boiling will not prevent illness. The toxin has no local effect on the digestive tract. It is a potent stimulator of T lymphocytes in the host, stimulating their proliferation and the release of various cytokines. The gastrointestinal effects are believed to be mediated by the release of interleukin 2, tumor necrosis factor beta, and interferon from mast cells.30 Stool, vomitus and blood can be tested for the presence of the enterotoxin, but this is typically done by local health departments or the CDC during large outbreaks and rarely done in clinical laboratories.31 The illness has an explosive onset, beginning 1 to 6 hours after ingestion of the contaminated food. Cramping and abdominal pain, with violent and often-repeated retching and vomiting, are the predominant symptoms. Diarrhea is a variable feature; it usually is mild, occasionally absent entirely, and infrequently profuse. Fever occasionally is present. Staphylococcal food poisoning is short-lived, usually subsiding in 6 to 8 hours and rarely lasting as long as 24 hours. Patients often are recovering by the time they seek medical attention. Attack rates are very high, often greater than 75% of the population at risk.29 The short incubation period and multiple cases among persons eating the same meal are highly suggestive of this disease. Examination of the stool is noncontributory, and no practical laboratory test is clinically available to confirm the diagnosis. The epidemiologic circumstances, however, usually provide adequate suggestive evidence.
Gastroenteritis
Background
Acute Invasive Bacterial Enteritis
Campylobacter Enteritis
Pathophysiology
Clinical Presentation
Diagnostic Strategies
Management
Salmonellosis
Pathophysiology
Clinical Presentation
Management
Shigellosis
Pathophysiology
Clinical Presentation
Diagnostic Strategies
Management
Yersinia enterocolitica Gastroenteritis
Pathophysiology
Clinical Presentation
Diagnostic Strategies
Management
Vibrio parahaemolyticus Gastroenteritis
Pathophysiology
Clinical Presentation
Diagnostic Strategies
Management
Enterohemorrhagic (Shiga Toxin–Producing) Escherichia coli Gastroenteritis
Pathophysiology
Clinical Presentation
Complications
Diagnostic Strategies
Management
Aeromonas Gastroenteritis
Clinical Presentation
Management
Plesiomonas shigelloides Gastroenteritis
Clinical Presentation
Management
Bacillus anthracis Infection
Pathophysiology
Clinical Presentation
Diagnostic Strategies
Management
Toxin-Induced Bacterial Gastroenteritis
Staphylococcal Food Poisoning
Pathophysiology
Clinical Presentation

Full access? Get Clinical Tree


Gastroenteritis
Only gold members can continue reading. Log In or Register to continue