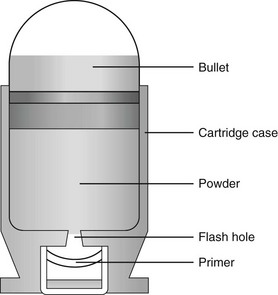
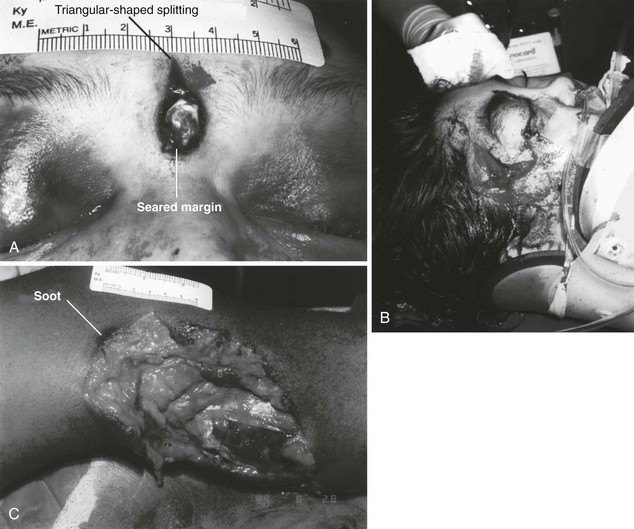
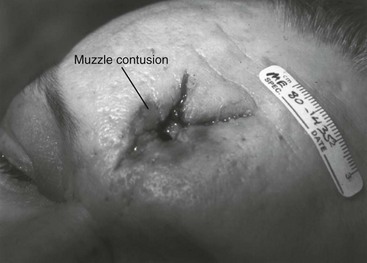
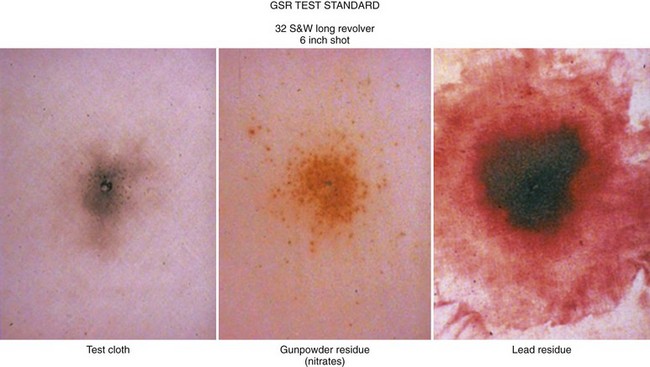
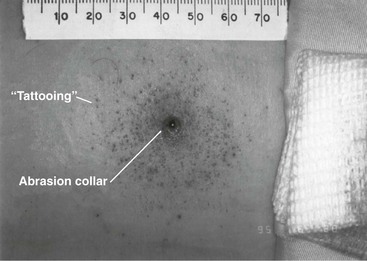
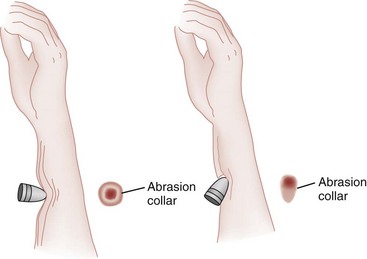
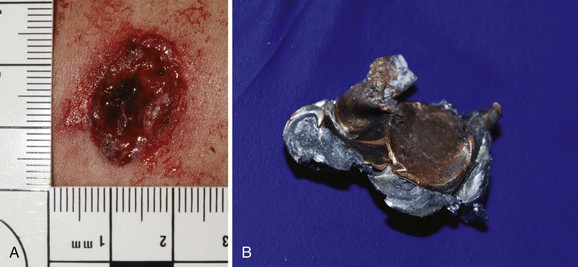
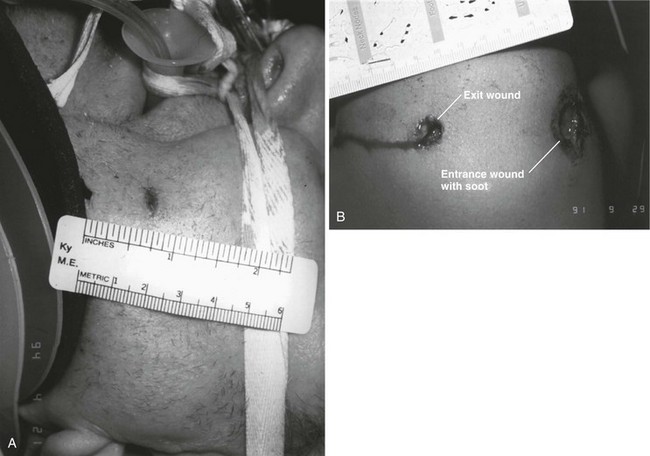
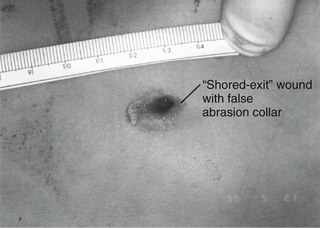
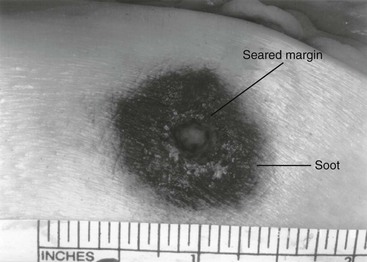
Chapter 65 Clinical forensic medicine is the application of forensic medical knowledge and techniques to live patients in a clinical setting. European, Australian, and British physicians—known as police surgeons, forensic physicians, forensic medical examiners, or forensic medical officers1,2—have a long history of performing clinical forensic examinations,3 including evaluations of prisoners and victims of physical and sexual assault.4,5 All patients who are victims of physical or sexual assault, abuse, or trauma have forensic needs. When treating injuries without consideration of their forensic significance, physicians may misinterpret wounds, fail to recognize victims of abuse or domestic violence, and inadequately describe the physical appearance of the wounds. During the provision of patient care, evidence that can be of critical significance to criminal or civil proceedings can be lost, discarded, or inadvertently washed away,6–20 despite requirements by The Joint Commission (TJC) to “preserve evidentiary materials and support future legal actions.”21 Emergency medicine programs have identified and described the need for forensic training in their residency curricula.9,10,14,22 In 1991 the Department of Emergency Medicine at the University of Louisville School of Medicine collaborated with the Kentucky Medical Examiner’s Office and established the first clinical forensic medicine training and consultative program in the United States.9,13,19,20 In 2006, the American College of Emergency Physicians established the Forensic Medicine Section to provide emergency physicians with additional forensic resources and training.23 In 2010 the Louisville Police Department created a full-time clinical forensic medicine consultation service to provide forensic evaluations for living victims of crimes, staffed by a forensic emergency physician and three part-time forensic nurse examiners. Forensic examinations are conducted with the consent of the patient, legal guardian, or court, or by implied consent. The evaluation includes a history and physical examination, photographs, and anatomic diagrams.22 Evidentiary material, including clothing, hair, blood, saliva, bullets, bomb fragments, and the like, are collected when indicated or when ordered by the court.24 If a patient has been admitted from the emergency department (ED) to surgery, an evaluation is done in the operating suite in conjunction with the trauma surgeons.25 In 2006 the British Royal College of Physicians established the Faculty of Forensic and Legal Medicine (FFLM) as the authoritative body on clinical forensic medicine in the United Kingdom.26 The FFLM has created training and certification programs and board-type certification examinations after 2 years of forensic practice for British physicians.26 Evaluations of gunshot and stab wounds, physical or sexual abuse, domestic violence, and motor vehicle–related trauma should be adequately documented for possible use in future legal proceedings. Documentation should include digital photographs as well as a narrative and diagrams.7–13,17–2225 However, in one trauma center, 70% of cases had improper or inadequate documentation, and 38% of cases had potential evidence improperly secured, incorrectly documented, or inadvertently discarded.8 When physical injuries are misinterpreted and these misinterpretations become the medical record or when valuable evidence is lost or destroyed in the process of providing patient care, there are consequences for the legal proceedings that may follow.3,6–20,26–30 These acts of omission or commission may deny patients their deserved redress in the justice system. To protect the interests of patients, EDs should implement protocols for wound documentation and evidence collection.11,12 Firearms continue to be the second leading cause of injury-related deaths in the United States—30,913 firearm-related deaths in 2009—after motor vehicle trauma.31 Emergency physicians treat more than 115,000 victims of gunshot wounds, principally from handguns, each year.32 The direct and indirect costs associated with gunshot wounds total $36 billion annually.33 The emergency physician is in the ideal position to evaluate and document the state of a gunshot wound because he or she sees and explores it before it is disturbed, distorted, or destroyed by surgical intervention.6–14,27,30 Documentation of gunshot wounds should include the anatomic location of the wound as well as its, size, shape, and distinguishing characteristics, and digital photographs of the wound should be taken. Wounds should be described according to the standard anatomic position with the arms to the sides and palms up. Clinicians should not describe wounds as “entrance” or “exit” but should document, using appropriate forensic terminology, a detailed description of the wound, including its appearance, characteristics, and location without attempting to interpret the wound type or bullet caliber.27,34–39 Exit wounds are not always larger than entrance wounds, and wound size does not consistently correspond to bullet caliber.18,27,36–42 The size of any wound (entrance or exit) is determined by five factors: the size, shape, configuration or angle, and velocity of the projectile at the instant of impact with tissue and the physical characteristics of the impacted tissue itself. If the projectile is slowed and its shape unchanged on exiting the skin, the exit wound may be the same size as or smaller than the corresponding entrance wound.34,41,42 If the projectile increases its surface area by fragmenting or changing its configuration while maintaining a substantial velocity, the exit wound may be significantly larger than the entrance wound.34,36–42 If the bullet strikes bone, fragments may extrude from the exit wound and contribute to the size and shape of the wound. Tissue elasticity also affects the wound size so that entrance or exit wounds may be smaller, equal to, or larger than the projectile that caused them.40–42 Wounds on the palm or sole may appear as slits and can be easily mistaken for stab wounds.34,41,42 Inappropriate terminology should be avoided.8,37,41,42 One example of inappropriate terminology is the use of the obsolete term powder burns, rather than soot, to describe the carbonaceous material associated with close-range wounds.34,35,41,42 Powder burns are literally the thermal injuries associated with flaming black powder used in muzzle loaders, antique weapons, and blank cartridges. These injuries do not occur with the smokeless powder used in modern ammunition. A treating physician may be requested to render factual testimony, expert testimony, or both in a criminal case. Expert forensic testimony rendered without an appropriate forensic examination or adequate forensic training may mislead participants in the criminal justice system (e.g., “the exit wound is always larger than the entrance wound”). Opinions related to entrance versus exit wounds or the range of fire can affect the determination of innocence or guilt.* The perennial speculation about entrance and exit wounds in the assassination of President Kennedy is one example of the significance of a forensic evaluation.29,30,44 The cartridge, or round, is composed of the primer, the cartridge case, the powder, and the bullet (Fig. 65-1). The bullet is the projectile that is propelled out of the muzzle. The primer is a small explosive charge in the base of the cartridge that ignites the gunpowder. The primer may contain lead, barium, or antimony. These materials may be deposited on the hands of the shooter, on the victim of a close-range assault, or on objects within a room in which the weapon was discharged.41 The cartridge case is typically made of brass, although other materials may be used. The function of the cartridge case is to slightly expand, sealing the chamber against the escaping gases and propelling the bullet down the barrel.41 On detonation, a cartridge case is imprinted with unique microscopic marks that are valuable evidence and should be preserved for law enforcement. The gunpowder found in all commercial cartridges except blanks is smokeless powder made with a single base (nitrocellulose) or a double base (nitrocellulose and nitroglycerine).41 When a weapon is discharged, not all of the gunpowder is consumed. A percentage of the unburned or partially burned gunpowder will travel out of the end of the muzzle for a short distance (<48 inches). The distance depends on the physical characteristics and shape of the powder and the weapon’s barrel length. Wound ballistics is the study of the effects of penetrating projectiles on the body.39,45–50 Tissue disruption (wound severity) is directly related to the amount of kinetic energy ( The principal mechanism for tissue damage by bullets is crushing. A bullet traveling through tissue generates two cavities, one permanent and the other temporary. The temporary cavity, a result of tissue stretching, lasts 5 to 10 msec from its generation until its collapse and leaves behind the permanently crushed tissue and the permanent cavity.39,41,45 The size of the permanent cavity varies with the size, shape, and configuration of the bullet. A hollow-point bullet that mushrooms can increase its diameter 2.5 times on impact and will increase the area of tissue crush 6.25 times compared with a nondeformed bullet.41 Range of fire is the distance from the muzzle to the victim and can be divided into four general categories: contact, near-contact or close range, intermediate or medium range, and indeterminate or distant range (Table 65-1). The size of the entrance wound does not correlate with the caliber of the bullet41 because the entrance wounds over elastic tissue will contract around the tissue defect and have a diameter much less than the caliber of the bullet.34,41 Table 65-1 Contact Wounds.: There are three subcategories of contact wounds: (1) tight contact, in which the muzzle is pushed hard against the skin; (2) loose contact, in which the muzzle is incompletely or loosely held against the skin; and 3) contact through clothing. In a tight contact wound, all material—the bullet, gases, soot, the incompletely burned pieces of gunpowder, and metal fragments—is driven into the wound. These wounds can vary from a small hole with seared blackened edges from the discharge of hot gases and an actual flame to a gaping stellate wound (Fig. 65-2). Large wounds occur when the wound is inflicted over thin, inelastic or bony tissue, and the injected hot gases cause the skin to expand until it stretches and tears. These tears will have a triangular shape, with the base of the triangle overlying the entrance wound. Tears are generally associated with .32 caliber or greater, or magnum loads. Large stellate contact wounds are easily misinterpreted as exit wounds if the determination is based solely on their size (see Fig. 65-2B).34,41 Stellate tears are not pathognomonic for contact wounds, however. Tangential wounds, ricochet or tumbling bullets, and some exit wounds may also be stellate. These wounds’ appearance differs from a tight contact wound’s by the absence of soot and powder within the wound and a lack of seared wound margins.34,41,42 In some tight contact wounds, expanding skin is forced back against the muzzle of the gun, leaving a characteristic muzzle abrasion or muzzle contusion (Fig. 65-3).34,41,42 Patterns such as these should be documented before wound débridement or surgery because they are helpful in determining the type of weapon used (revolver vs. semiautomatic).25,41 Discharge of a weapon in contact with clothing results in the gases and soot being deposited between the garment and the skin. This results in a diffuse pattern of soot surrounding a wound with seared margins (see Fig. 65-2C). Close-Range Wounds.: Close range is the maximum range at which soot is deposited on the wound or clothing. The muzzle-to-target distance is usually less than 6 inches but may be as much as 12 inches.40–42 Beyond 6 inches, most of the soot usually falls away and does not reach the skin or clothing. The concentration of the soot varies inversely with the muzzle-to-target distance and is influenced by the type of gunpowder and ammunition used, the length of the weapon’s barrel, and the caliber and type of weapon itself (Fig. 65-4). Figure 65-4 Close-range wound with soot deposition. Soot is associated with a range of fire of 6 inches or less. A precise range of fire (e.g., 2 inches vs. 5 inches) cannot be determined from examination of the wound alone. A forensic firearms examiner can attempt to reproduce the patient’s soot pattern on a target by test-firing the offending weapon at different ranges using ammunition similar to the ammunition that caused the wound (Fig. 65-5). The validation of this test and the determination of a range of fire depend on the accuracy and detail in the physician’s report regarding the size of the soot pattern. Because soot can be removed with débridement or wound cleansing, its presence and configuration around the wound should be noted and photographed before débridement unless the patient’s clinical condition precludes this attention to detail.25 Intermediate-Range Wounds.: Tattooing, or stippling, is pathognomonic for an intermediate-range gunshot wound. Tattooing appears as punctate abrasions and is caused by contact with partially burned and wholly unburned pieces of gunpowder (Fig. 65-6). Tattooing or stippling cannot be wiped away. Tattooing rarely occurs on the palms of hands or soles of feet because of the thickness of the epithelium.41 Tattooing may occur as close as 1 cm to and as far away as 1.3 m from the weapon but is generally found at distances of 60 cm or less.40–42,51 The density of the tattooing and the associated pattern depend on the length of the barrel, the muzzle-to-skin distance, the type of gunpowder, the presence of intermediate objects, and the caliber and type of ammunition. Clothing, hair, or other barriers may prevent tattooing from occurring. The presence of partially or entirely unburned pieces of gunpowder and gunpowder residues on clothing or skin aids in determining the range of fire. On rare occasion, pieces of gunpowder can penetrate thin clothing and leave punctate abrasions (Fig. 65-7). Long-Range Wounds.: The distant or long-range wound is inflicted from far enough away that only the bullet makes contact with the skin. There is no tattooing or soot. As the bullet penetrates the skin, the skin is indented, resulting in the creation of an abrasion collar, also called an abrasion margin, abrasion rim, or abrasion ring (Fig. 65-8).41,42 This collar is an abraded area of tissue that surrounds an entry wound as the result of friction between the bullet and the epithelium. The width of the abrasion collar varies with the angle of impact. Most entrance wounds will have an abrasion collar. Entrance wounds on the palms and soles are exceptions. These usually appear slitlike.41 Determining the range of fire may be complicated when clothing prevents the deposition of soot and powder on the skin. Without the overlying clothing or without information regarding the crime scene, the wound may appear to be from a distant range of fire. In reality, the range may have been close or intermediate. Conversely, a projectile discharged from a distant range of fire may mimic an intermediate range if it strikes an object, such as glass, that fragments. As with unburned gunpowder, when the glass fragments strike the skin, they may also cause punctate abrasions, resulting in pseudotattooing (Fig. 65-9).41,52 Atypical Entrance Wounds.: Atypical entrance wounds occur when a bullet encounters an intermediate object, such as a window, wall, or door, before striking the victim. The intermediate object may change the bullet’s size, shape, or path. Such changes can result in entrance wounds with large stellate configurations that mimic close-range or contact wounds (Fig. 65-10).53,54 Ricochet bullets may also cause atypical entrance wounds. Graze wounds are atypical wounds from tangential contact with a passing bullet. Directionality of the bullet may be determined from a close examination of the wound.41,55,56 The bullet produces a trough with the formation of skin tags on the lateral wound margins that point toward the weapon and away from the direction in which the bullet was traveling (Fig. 65-11).55 The size of the exit wound is determined by the energy transferred from the bullet to underlying tissue and by the bullet’s size and configuration as it exits the skin (Fig. 65-12).41,42 When a bullet enters the skin, its configuration may change from its usual nose-first attitude owing to tumbling and yaw. A bullet that exits the skin sideways, or one that has increased its surface area by mushrooming or transferring its energy to underlying bone, will have an exit wound larger than its entrance wound.34,41 Atypical Exit Wounds.: A shored-exit wound is a wound that has an associated false abrasion collar. If the skin is pressed against or supported by a firm object or surface at the moment the bullet exits, the skin can be compressed between the exiting bullet and the supporting surface (Fig. 65-13).41,42,57 Examples of supporting structures include belts, floors, walls, doors, chairs, and mattresses.
Forensic Emergency Medicine
Perspective
Forensic Aspects of Gunshot Wounds
Errors of Interpretation and Terminology
Forensic Aspects of Handguns
Handgun Ammunition
Handgun Wound Ballistics
 ) transferred to it, not to the total amount of kinetic energy possessed by the bullet.39,41,45 Bullets fired from rifles generally have a higher velocity (1500 to 4000 ft/s) than do those fired from handguns (700 to 1600 ft/s). Rifle bullets have more kinetic energy and therefore a theoretically higher wounding potential, but wound severity is the result of multiple variables, the most important of which are bullet type (weight, deforming type, fragmenting type), bullet velocity, and the characteristics, location, and nature of the impacted tissue itself (tissue over bone or tissue over organs).39,41,46–50
) transferred to it, not to the total amount of kinetic energy possessed by the bullet.39,41,45 Bullets fired from rifles generally have a higher velocity (1500 to 4000 ft/s) than do those fired from handguns (700 to 1600 ft/s). Rifle bullets have more kinetic energy and therefore a theoretically higher wounding potential, but wound severity is the result of multiple variables, the most important of which are bullet type (weight, deforming type, fragmenting type), bullet velocity, and the characteristics, location, and nature of the impacted tissue itself (tissue over bone or tissue over organs).39,41,46–50
Forensic Evaluation of Handgun Wounds
RANGE
INCHES (BARREL TO SKIN)
PHYSICAL PROPERTIES
Contact
0
Soot, seared skin, triangular tears
Close
0-6
Soot, abrasion collar (abrasion collar may be obscured by soot)
Intermediate
<48
Tattooing, abrasion collar
Distant or indeterminate
Any distance
Abrasion collar (intermediate objects will prevent soot and gunpowder from contacting the skin)
Exit Wounds
< div class='tao-gold-member'>

Full access? Get Clinical Tree


Forensic Emergency Medicine
Only gold members can continue reading. Log In or Register to continue