Flexible Endoscopic Intubation
Michael F. Murphy
Peter M.C. DeBlieux
DESCRIPTION
Tracheal intubation over a flexible endoscope is an invaluable technique in airway management, particularly in patients for whom standard laryngoscopy and orotracheal intubation have failed, or are anticipated to be difficult or impossible. Endoscopic devices are used both for diagnostic evaluation of the upper airway and for tracheal intubation.
INDICATIONS AND CONTRAINDICATIONS
Indications for endoscopic intubation in emergency airway management generally are identified during the LEMON evaluation for the difficult airway (see Chapter 2) and include the following:
The patient with distorted upper airway anatomy, such as angioedema, oropharyngeal abscess, hematoma (or other trauma), or Ludwig’s angina, or those with slowly progressive laryngeal lesions, such as lingual and laryngeal cancers.
The patient with laryngeal trauma or tracheal disruption. In these cases, intubation with continuous visualization is recommended. The endoscope meets this indication.
The patient for whom cervical spine immobility is required, particularly if the airway is predicted to be difficult.
The patient who fails the 3-3-2 rule (restricted mouth opening, small mandible, or high larynx) or has a grade 4 Mallampati score.
The patient with morbid obesity.
Failed intubation in the “can’t intubate, can oxygenate” scenario, when continuing deterioration of the airway is not anticipated.
Contraindications to endoscopic intubation are mostly relative and may include the following:
Excessive blood and secretions in the upper airway, which have the great potential to obscure the view and reduce the success rate with the endoscopic technique. Some experienced bronchoscopists use the endoscope to transilluminate their way into the trachea, only then looking through the scope to verify the position of the endoscope in the trachea, but this is highly operator dependent.
High-grade upper airway obstruction (resulting from foreign bodies or other lesions), where the procedure may precipitate total airway obstruction. If a patient has a high-grade supraglottic airway obstruction, with impending complete airway closure, the delays and risks of precipitating complete airway obstruction or laryngospasm argue strongly against endoscopic intubation and in favor of cricothyrotomy.
Inadequate oxygenation by bag and mask does not permit endoscopic intubation because of the time required (can’t intubate, can’t oxygenate).
TECHNIQUE
Overview
Endoscopic intubation is a technical challenge that requires initial training, and then skill maintenance activities to maintain speed and success. Manual dexterity in manipulating the endoscope is essential to performing endoscopic intubation in a timely fashion. This skill is best learned by attending endoscopic intubation workshops with expert instruction, and then practicing on intubation manikins or high-fidelity human patient simulators before one attempts to intubate a patient. This is particularly true in patients with difficult airways. The manufacturers of endoscopes can usually provide training videos, product support personnel, and manikins to support this endeavor.
The requisite psychomotor skills cannot be developed without dedicated practice, and lack of training, practice, and experience constitute the most common cause of failed endoscopic intubation. A reasonable level of dexterity in bronchoscopic manipulation can be achieved within 3 to 4 hours of independent practice using an intubation model. Recent studies have shown that the technique can also be learned in real-life situations by the performance of upper airway endoscopy when diagnostic opportunities, such as searching for foreign bodies and evaluating the causes of hoarseness, severe sore throat, and other upper airway conditions, present themselves. As is the case with many of the specialized airway techniques, the patient who requires semi-emergent, but controlled, intubation, such as an overdose victim without an anticipated difficult airway and patients who are easily ventilated with normal oxygen saturation, may be appropriate candidates for endoscopic intubation. Because success depends on familiarity and skill in using the device, gaining experience in routine cases is invaluable before one is required to perform a difficult endoscopic intubation in a crisis.
Preparation
Although the emergency difficult or failed airway situation often does not permit lengthy preparation and a methodical approach, maximal success with this technique requires both psychological
and pharmacologic patient preparation. When the procedure is to be done “awake” (see Chapter 23), optimizing the chances for success includes the following:
and pharmacologic patient preparation. When the procedure is to be done “awake” (see Chapter 23), optimizing the chances for success includes the following:
Explain to the patient what to expect.
Administer an antisialogogue, such as glycopyrrolate 0.01 mg per kg IM or IV, at least 10 minutes (20 minutes if possible) in advance of the procedure to reduce secretions, enhancing both the visualization and the effect of topically applied local anesthesia.
Achieve profound local anesthesia of the airway. An endoscopic intubation may require as much sedation and topical anesthesia as is necessary for awake direct laryngoscopy.
Administer adequate sedation (see Chapter 23).
Scope Selection
Instrument selection for the emergency department (ED) is an important issue. Affordable and durable scopes are easily available from a variety of manufacturers. Selection of a manufacturer may be guided by existing service contracts in your specific institution. These instruments, although expensive, find several uses in the ED to justify such an expenditure:
Tracheal intubation, both nasal and oral.
Diagnostic laryngoscopy.
Oropharyngeal foreign body location and extraction.
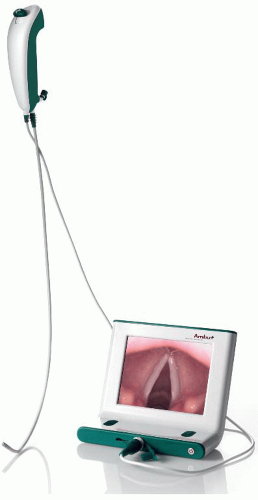
Recently, at least one manufacturer has introduced a single-use flexible endoscope, using complementary metal-oxide semiconductor (CMOS) video, making flexible endoscopy much less expensive. (Fig. 15-1)
The scope should be of sufficient caliber and stiffness to guide the passage of an endotracheal tube (ETT) over itself through the angles of the airway without kinking and resist being flipped out of the trachea, while maintaining flexibility and ease of manipulation. Most endoscope manufacturers produce intubation-specific devices that have the added stiffness of the fiber bundle to allow ETTs to be guided into the trachea over the scope. This feature allows scopes that are small enough (3- to 4-mm tip diameter) to be painlessly and atraumatically passed through a topically anesthetized nose for diagnostic work also to be used for endoscopic intubation. Neonatal and pediatric endoscopes (2- to 3-mm tip diameter) are also available.
The endoscopic bundle should be long enough (600 mm) to allow bronchoscopy and airway toilet in the ED. Standard bronchoscopes are 600 mm in length. Some manufacturers produce 400-mm intubating endoscopes that are not long enough for pulmonary care if this is planned. A separate channel for the injection of local anesthetic or saline and suctioning is essential, although the smaller neonatal and pediatric endoscopes may not have them owing to their small size. A formerly recommended practice, the insufflation of oxygen through the suction working channel to maintain saturations and blow secretions out of the way, is now contraindicated following several cases of gastric insufflation, perforation, and death. Endoscopes with battery-powered, portable, self-contained light sources are compact and may be preferable for ED applications.
Care of the Instrument
Some general precautions are necessary to prevent damage to the relatively delicate fiberoptic bundles in a fiberoptic scope and similar precautions are prudent even with the less damage-prone video endoscopes:
Do not drop the scope.
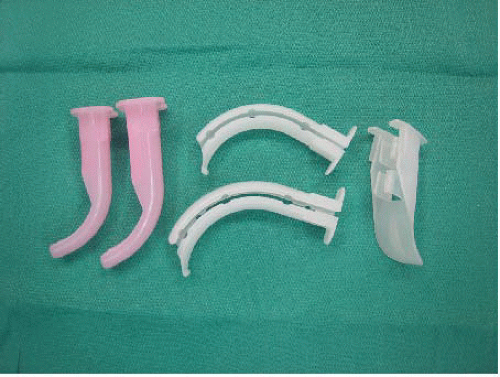
Use a bite-block (e.g., oral airway) to protect the scope. Most oral endoscopic intubation guides incorporate this feature (e.g., the Berman intubating/pharyngeal airway, also called the “Berman breakaway airway”) and are invaluable aids to successful oral endoscopic intubation (Fig. 15-2). The Rapid Oral Tracheal Intubation Guidance System (ROTIGS) airway has the advantage of keeping one above the tongue and away from the gag-producing glossopharyngeal nerve territory (Fig. 15-3).
Avoid acute bending or kinking of the endoscope, especially when advancing the ETT over the scope into the trachea.
If rotation of the ETT during intubation is necessary, rotate both the ETT and the scope to avoid damage to the fibers.
Lubricate the ETT by spraying local anesthetic agent or other water-soluble material down the tube to allow easy removal of the scope after the ETT is in place. Lubricating the scope makes it slippery and difficult to manipulate.
Clean the device, including the working channel, immediately after use. The best routine is to suction 1 L of saline through the device immediately after use. Manufacturers and endoscopy units will provide instructions for acceptable cleaning routines.
Do not flex the tip against undue resistance to manipulate the direction of an ETT or use it to move tissue out of the way.