CHAPTER 109
Finger Dislocation
(PIP Joint)
Presentation
The patient will have jammed his finger, causing a hyperextension injury that forces the middle phalanx dorsally and proximally out of articulation with the distal end of the proximal phalanx. An obvious swollen, painful deformity of the proximal interphalangeal (PIP) joint will be present, unless the patient or a bystander has reduced the dislocation on his own.
There should be no sensory or vascular compromise.
What To Do:
 When a deformity is present, unless there is crepitus or bony instability and a shaft fracture is suspected, radiographs may be deferred, and joint reduction can be carried out first. If the nature of the injury is at all unclear, obtain radiographs before attempting a reduction.
When a deformity is present, unless there is crepitus or bony instability and a shaft fracture is suspected, radiographs may be deferred, and joint reduction can be carried out first. If the nature of the injury is at all unclear, obtain radiographs before attempting a reduction.
 If there has been significant delay in seeking help or if the patient is suffering considerable discomfort, a digital block over the proximal phalanx or, most effectively, 1% lidocaine injected directly into the joint will allow a more comfortable reduction. The patient may be allowed the choice of whether to use this anesthesia or not.
If there has been significant delay in seeking help or if the patient is suffering considerable discomfort, a digital block over the proximal phalanx or, most effectively, 1% lidocaine injected directly into the joint will allow a more comfortable reduction. The patient may be allowed the choice of whether to use this anesthesia or not.
 To reduce a dorsal dislocation, do not just pull on the fingertip; instead, with the joint slightly extended, push the base of the middle phalanx distally using your thumb while holding the patient’s distal phalanx with your other thumb and index finger. Then, apply traction and gently flex the middle phalanx until it slides smoothly into its natural anatomic position (Figure 109-1).
To reduce a dorsal dislocation, do not just pull on the fingertip; instead, with the joint slightly extended, push the base of the middle phalanx distally using your thumb while holding the patient’s distal phalanx with your other thumb and index finger. Then, apply traction and gently flex the middle phalanx until it slides smoothly into its natural anatomic position (Figure 109-1).
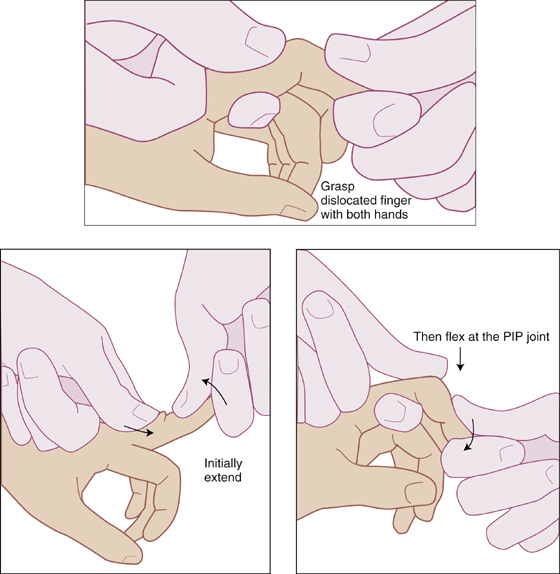
Figure 109-1 Proximal interphalangeal joint reduction for dorsal dislocation.
 Lateral PIP dislocations are dramatic in appearance (pointing laterally at a very unnatural angle), and often they have been self-reduced. When this type of dislocation requires reduction, grasp the end of the affected finger between your thumb and index finger and apply steady traction along the long axis. Bring the middle phalanx into line with the proximal phalanx and squeeze the sides of the PIP joint to correct any residual lateral displacement. A collateral ligament rupture with resultant ulnar or radial joint instability generally accompanies these dislocations.
Lateral PIP dislocations are dramatic in appearance (pointing laterally at a very unnatural angle), and often they have been self-reduced. When this type of dislocation requires reduction, grasp the end of the affected finger between your thumb and index finger and apply steady traction along the long axis. Bring the middle phalanx into line with the proximal phalanx and squeeze the sides of the PIP joint to correct any residual lateral displacement. A collateral ligament rupture with resultant ulnar or radial joint instability generally accompanies these dislocations.
 Volar PIP dislocations are uncommon but are almost always accompanied by an injury to the central slip of the extensor tendon, which can lead to a disabling boutonnière deformity if not properly treated (see Chapter 99). These dislocations can be reduced by applying the same principles used for the dorsal dislocation but in reverse. With mild flexion, push the proximal end of the middle phalanx distally with one thumb, while applying traction on the distal phalanx held between your other thumb and index finger until finally pushing and pulling the middle phalanx dorsally into its normal position.
Volar PIP dislocations are uncommon but are almost always accompanied by an injury to the central slip of the extensor tendon, which can lead to a disabling boutonnière deformity if not properly treated (see Chapter 99). These dislocations can be reduced by applying the same principles used for the dorsal dislocation but in reverse. With mild flexion, push the proximal end of the middle phalanx distally with one thumb, while applying traction on the distal phalanx held between your other thumb and index finger until finally pushing and pulling the middle phalanx dorsally into its normal position.
 Irreducible dislocations may be caused by avulsion and entrapment of the volar plate in the joint, entrapment of the long flexor tendon in the joint, or entrapment of an osteochondral fragment. These and all open dislocations necessitate immediate consultation with an orthopedist or hand surgeon. Surgical repair will also be required if there is an avulsion fracture of more than 33% of the articular surface area.
Irreducible dislocations may be caused by avulsion and entrapment of the volar plate in the joint, entrapment of the long flexor tendon in the joint, or entrapment of an osteochondral fragment. These and all open dislocations necessitate immediate consultation with an orthopedist or hand surgeon. Surgical repair will also be required if there is an avulsion fracture of more than 33% of the articular surface area.
 When the joint is reduced, test the PIP joint for collateral ligament instability by applying varus and valgus stress in full extension and 20 degrees of flexion. A partial ligament tear allows no laxity, but there is little or no resistance to stress if the collateral ligament tear is complete. Test for avulsion of the central extensor tendon slip by having the patient attempt to extend the middle phalanx against resistance (see Chapter 99). If the patient cannot extend his finger at the PIP joint, a central slip extensor injury should be suspected. Testing for avulsion of the volar carpal plate, you will be able to hyperextend the PIP joint more than that of the same finger on the uninjured hand if a disruption is present. Delayed diagnosis of volar plate disruption may lead to chronic pseudoboutonnière deformity (see Chapter 99). If any of these associated injuries exist, orthopedic consultation should be sought, and prolonged splinting and rehabilitation may be required.
When the joint is reduced, test the PIP joint for collateral ligament instability by applying varus and valgus stress in full extension and 20 degrees of flexion. A partial ligament tear allows no laxity, but there is little or no resistance to stress if the collateral ligament tear is complete. Test for avulsion of the central extensor tendon slip by having the patient attempt to extend the middle phalanx against resistance (see Chapter 99). If the patient cannot extend his finger at the PIP joint, a central slip extensor injury should be suspected. Testing for avulsion of the volar carpal plate, you will be able to hyperextend the PIP joint more than that of the same finger on the uninjured hand if a disruption is present. Delayed diagnosis of volar plate disruption may lead to chronic pseudoboutonnière deformity (see Chapter 99). If any of these associated injuries exist, orthopedic consultation should be sought, and prolonged splinting and rehabilitation may be required.
 Postreduction radiographs should be taken. “Chip fractures” may represent tendon or ligament avulsions. Radiographs will also allow you to detect an incomplete reduction. The true lateral view is most helpful in detecting subtle subluxation and small avulsion fractures on the volar surface. In an unsatisfactory reduction, the joint’s surfaces will be misaligned.
Postreduction radiographs should be taken. “Chip fractures” may represent tendon or ligament avulsions. Radiographs will also allow you to detect an incomplete reduction. The true lateral view is most helpful in detecting subtle subluxation and small avulsion fractures on the volar surface. In an unsatisfactory reduction, the joint’s surfaces will be misaligned.
 If the joint feels unstable with a tendency to dislocate when extended, or there are minor fractures present, then splint the finger 20 to 30 degrees short of full extension with a padded dorsal splint for 3 to 4 weeks (Figure 109-2). Follow up the splinting with buddy taping (Figure 109-3) to the adjacent finger for another 2 to 4 weeks, and provide follow-up for active range-of-motion exercises to restore normal joint mobility. When collateral ligament instability is present, buddy tape the affected finger to the finger adjacent to the ruptured ligament.
If the joint feels unstable with a tendency to dislocate when extended, or there are minor fractures present, then splint the finger 20 to 30 degrees short of full extension with a padded dorsal splint for 3 to 4 weeks (Figure 109-2). Follow up the splinting with buddy taping (Figure 109-3) to the adjacent finger for another 2 to 4 weeks, and provide follow-up for active range-of-motion exercises to restore normal joint mobility. When collateral ligament instability is present, buddy tape the affected finger to the finger adjacent to the ruptured ligament.
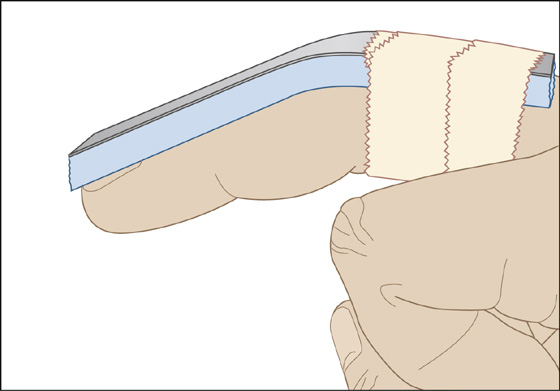
Figure 109-2 Dorsal extension block splint for proximal interphalangeal dislocation.
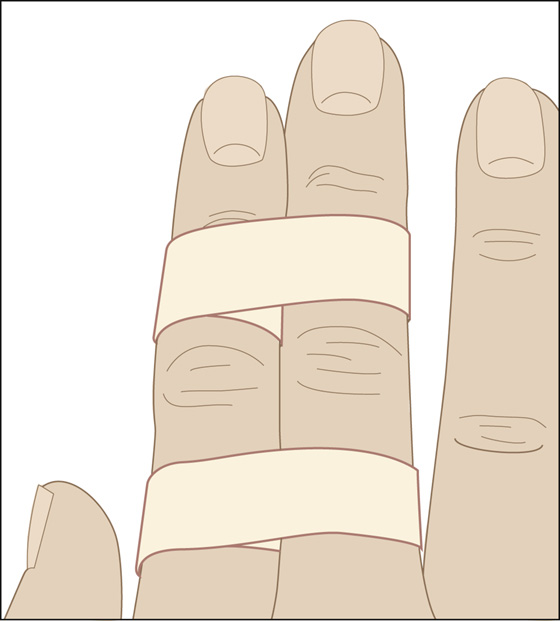
Figure 109-3 Buddy taping.
 When a central extensor tendon slip injury is suspected, splint the PIP joint in full extension without immobilizing the distal interphalangeal or metacarpophalangeal joints (see Chapter 99).
When a central extensor tendon slip injury is suspected, splint the PIP joint in full extension without immobilizing the distal interphalangeal or metacarpophalangeal joints (see Chapter 99).
 If the joint feels stable, “buddy taping” to adjacent digits for 7 to 10 days is an acceptable immobilization technique (see Figure 109-3). The tape should be removed at night or if the skin becomes wet (to prevent skin maceration). Have the patient dry the skin thoroughly prior to re-taping. Cotton padding placed between fingers can also be used to prevent skin breakdown.
If the joint feels stable, “buddy taping” to adjacent digits for 7 to 10 days is an acceptable immobilization technique (see Figure 109-3). The tape should be removed at night or if the skin becomes wet (to prevent skin maceration). Have the patient dry the skin thoroughly prior to re-taping. Cotton padding placed between fingers can also be used to prevent skin breakdown.
 Inform the patient that joint swelling and stiffness with loss of motion may persist for several months after the initial injury. Prophylactic nighttime PIP extension splinting can be used to prevent the mild PIP joint flexion contractures that are common consequences of these injuries. Active range-of-motion exercises performed by squeezing a soft foam ball can be helpful.
Inform the patient that joint swelling and stiffness with loss of motion may persist for several months after the initial injury. Prophylactic nighttime PIP extension splinting can be used to prevent the mild PIP joint flexion contractures that are common consequences of these injuries. Active range-of-motion exercises performed by squeezing a soft foam ball can be helpful.
 Remind the patient to keep the injured finger elevated. If it provides comfort, you can recommend ice application for 20 minutes three to four times over the next 24 hours and acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) for pain.
Remind the patient to keep the injured finger elevated. If it provides comfort, you can recommend ice application for 20 minutes three to four times over the next 24 hours and acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) for pain.
What Not To Do:
 Do not immobilize the PIP joints by taping over them when buddy taping. Early mobilization of this joint is an important benefit.
Do not immobilize the PIP joints by taping over them when buddy taping. Early mobilization of this joint is an important benefit.
Discussion
Proximal interphalangeal dislocations are often simple and easily reduced. However, they may also lead to severely restricted hand function. Most are dorsal dislocations, with the middle phalanx dislocating dorsally, and involve disruption of the volar plate. Often, an athlete reduces the finger himself, or a coach does it (hence the term “coach’s finger”).
Early recognition of instability—either dorsal, volar, or lateral—offers the best possibility of closed treatment leading to satisfactory functional healing. The main goals are to enable volar plate, collateral ligament, or central slip healing, and to restore normal joint function.
Fracture dislocation is the most disabling PIP joint injury and can result in both dorsal and volar instability (Figure 109-4).

Full access? Get Clinical Tree


