FIGURE 1 Increasing weight and repetitions for quadriceps exercise.
However, rest must occur initially on a nearly continuous schedule; a brief rest follows when each quota is met, even should the patient indicate a desire to proceed immediately to the next exercise. That kind of eagerness can be dealt with by keeping the interim rest brief. To ensure continuous and immediate reinforcement with rest, it is essential that the therapist be present during early treatment trials. The therapist’s presence also ensures immediate delivery of the second reinforcer, attention, also on an initially nearly continuous schedule. Therapists must therefore avoid double scheduling during early phases of treatment. Therapists must be available and militantly ready to deliver the essential reinforcement. Most patients who show consistent treatment progress soon come to the point where they will rest automatically after completing a quota and recording its performance. Once treatment momentum is achieved, as with all thoughtful reinforcement regimens, therapist attention can become intermittent and on a diminishing schedule. A patient can be left increasingly to work somewhat on his or her own, with only periodic checks and attentive responses from the therapist during the course of each session. Even then, however, it is important to ensure that the end of the session is duly noted by the therapist and that consistent attention and encouragement are then delivered.
In the early phases of treatment, exercise sessions themselves need to be spaced through the day to provide sufficient between-session rest periods. In the inpatient setting, occupational and physical therapy sessions need to be separated in time to provide ample rest. Later on, as quotas expand and the work load on the patient increases, less and less rest is likely to be required, relative to the amount of activity or exercise accomplished. Treatment sessions become longer and closer together. The treatment day moves in the direction of a full day’s work
There is no essential difference in the exercise format when treatment is on an outpatient basis. The major difference is that a spouse, other family member, or some other designated treatment observer fills the role of the physical or occupational therapist. The procedures remain the same. Observer presence, undivided attention, and militant surveillance and reinforcement are essential during early trials. It is perhaps more risky to anticipate that the amount of observer involvement and judicious observation can be reduced in outpatient treatment. There are usually fewer collateral cues and reinforcers encouraging full performance at home than in the hospital setting. Accordingly, treatment should be planned in anticipation of the observer needing to be present virtually throughout the treatment program. That constraint may be eased in later phases, if circumstances indicate that the patient is judicious in performing, recording, and spacing of exercise to permit appropriate rest intervals and is deriving sufficient sustaining reinforcement from rest and indications of progress not to require the additional support of observer attention.
Outpatient performance receives additional surveillance and reinforcement from the periodic clinic visits with their exercise sessions under professional observation. The frequency of clinic visits may also be systematically faded according to the situation. A patient whose reliability is subject to doubt or one who has questionable observers as noted previously, may require clinic visits one to three times per week at the outset. Those visits bolster patient and observer performance and provide earlier detection of noncompliance with the regimen. The frequency of clinic visits may be faded as confidence indicates. Interim phone calls from office personnel may provide additional bolstering.
Management of Quota Failures
The contingent reinforcers for exercise or activity are rest and attention. That means they are delivered when performance occurs and that they are not delivered when there is nonperformance.
Most patients sooner or later will fail one or more quotas, although the rate of quota failure tends to be surprisingly low, perhaps as little as 10% or less. Failure to meet a quota may occur for any number of reasons. It may be that the quotas for the exercise have reached and exceeded a practical maximum for that patient or that insufficient rest is being provided between exercises. It may be that on that particular day the patient is simply tired or, for whatever reason, less ready than usual to strive to meet quotas. It may be that the patient is testing whether attention or rest continues to be work contingent or have reverted to the typical pretreatment pain contingent pattern. The possibilities are endless.
The procedure to follow will usually permit one soon to distinguish quota failures representing respondent pain and the patient’s having reached a temporary or more permanent practical maximum for the exercise in question, from random failure or failure indicative of ineffective or inappropriate reinforcement. As will be spelled out immediately following, repeated trials in subsequent sessions will provide opportunity to discard random or daily variability as a factor and to check on the adequacy of the scheduling and delivery of reinforcement.
The procedure is straightforward. First, the therapist militantly avoids encouraging or exhorting the patient to try further. Attention is contingent on performance, not nonperformance. With a shrug of the shoulders or some other noncommittal response, the therapist records the amount done and sees to it that the patient does the same. If additional exercises are yet to be accomplished in the session, he or she may say something on the order of, “I’ll check back with you in a moment and we’ll start the next exercise,” and leaves briefly, if only to get a drink of water. She then returns and cues the patient to begin the next exercise, again without comment or encouragement about the importance of meeting the quota for that exercise. Alternatively, she may simply stand by quietly until the patient is ready to proceed with the next exercise. If the next quota is met, it is duly recorded, the rest interval is provided and she makes some attentive or praising comment, although without referring to the previously failed quota. If the second quota is also failed, she repeats the process just described.
If a quota is failed for the final scheduled exercise, the therapist, as before, gives a shrug of the shoulders noncommittally, records the amount done, and says, “I’ll see you (at the time of the next scheduled session).” The patient is then instructed to return to his room (or wherever he or she is next scheduled to be), and nothing more is said about the matter.
Sometimes a patient will indicate before beginning a session or an exercise that he or she cannot meet the quota or, perhaps, that it is doubtful the quota can be met. The therapist response is to avoid special encouragement. He or she might say, “Well, that is up to you, but why don’t you go ahead and see what you can do?” If the patient begins to perform, the therapist might make a special effort to remain close by and to maintain casual conversation so long as performance continues, thereby momentarily enriching the amount of professional attention contingent on patient effort. If the patient stops before the quota is reached, that therapist attention is withdrawn in the manner described above. When this kind of additional therapist attention results in increased performance, the evidence is clear that social attention is both potent and essential at this stage of treatment. It should continue to be available until patient progress gains additional momentum.
From the preceding examples, let it be assumed that one or more quotas were not met. Performance may have been partial or not even attempted. At the time of the next session, mindful of the preceding quota failure(s), the therapist is geared to be available. When the patient appears, the session progresses as if there had been no quota failure. There is no exhortation or special encouragement. The quota is as it would have been had there been no failure. The quota is not reduced nor held the same; it continues to advance at the previously determined rate. This is illustrated in Figure 3–8. The procedure remains as before. If quotas are met, they receive the same consequences as before. If they are not met, the procedures just set forth are again followed.
It is important, in the sessions during or immediately after quota failure episodes, that each exercise in the set be presented. In the extreme case, for example, a patient may appear and announce that he or she is unable to perform any repetitions of any of the prescribed exercises. If at all possible the therapist is to endeavor to get the patient at least to set up to try each exercise. There is a fine line here. The therapist should, at this moment, see the objective as one of letting the patient demonstrate nonperformance of each exercise in turn. He or she is neither trying to encourage and promote performance nor to punish nonperformance by compelling the patient arbitrarily to go through a ritual of refusal for each element of the exercise set. Instead, the therapist is providing opportunity for rest and for his or her attention to be applied contingently to each exercise. By requesting the patient to set up at least to approach each exercise, the therapist is also helping to delay rest and time out from exercise so that those reinforcers do not become available so soon after failure to perform. He or she can properly comment to the patient that she understands that there are times when one simply does not feel up to an exercise task. On the other hand, one’s feelings are sometimes deceptive, and it may be that the patient may find more can be accomplished than is anticipated. At any rate, it is important to determine that, “ … and so what I want you to do is to give it a try and let’s see what happens. It is up to you as to when you stop, but at least get in position to start each exercise.” Partial performance or even simply positioning to begin an exercise is not lavishly praised or socially reinforced. In matter-of-fact style, the therapist stands by while the patient prepares to begin each exercise. Any performance short of meeting the full quota is, as above, responded to in matter-of-fact fashion. The amount accomplished is recorded, and the next exercise is presented. Success at meeting a quota receives special praise: “That’s great! Rest a moment and then let’s see what you can do with this one.”
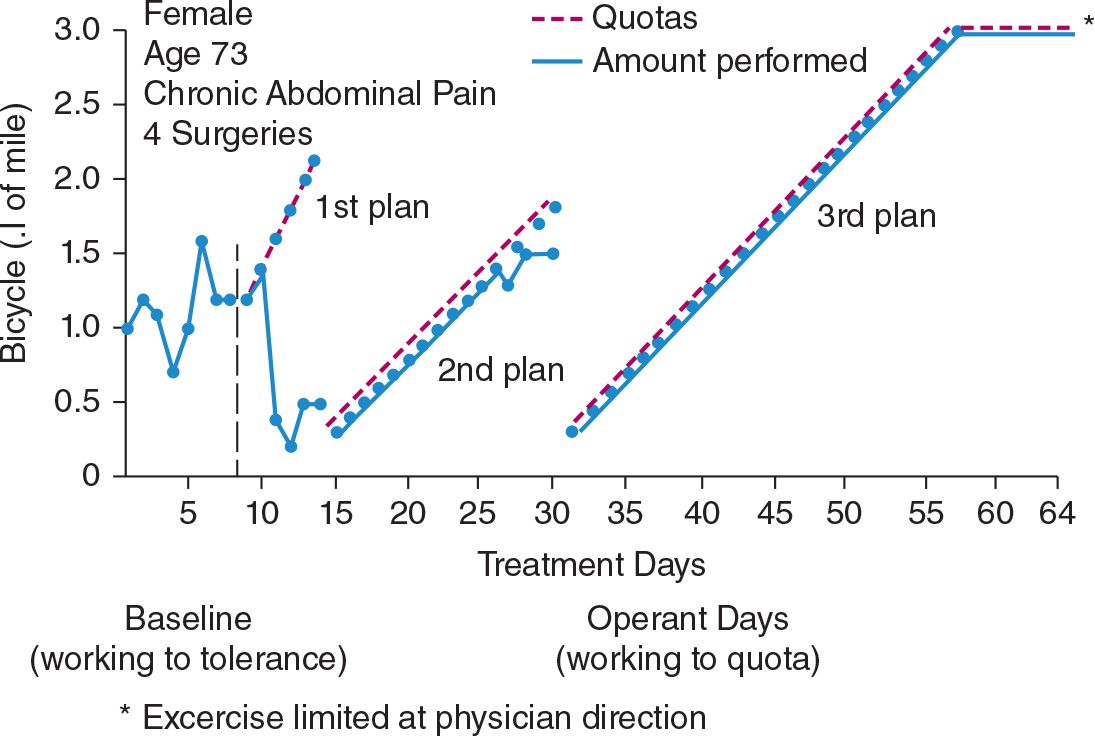
If there is success at meeting a quota after one or more failures, the quota increment pattern continues without alteration. Performance graphs (Chapter 12) for the exercise will show a gap or temporary drop, but the subsequent resumption of the upward climb (Fig. 3–8) shows an example of this. The program proceeds as previously scheduled. Figure 2 illustrates by case example how quotas continue to increase when isolated failures occur. This was also shown in Figure 3–8.
Let it now be supposed that the quota for one or more exercises is failed on several successive trials. The number is arbitrary, but three successive failures seems a reasonable reference point. After three successive failures, the quota is deliberately dropped back to a point previously consistently surpassed by the patient. If, for example, baseline data led to an initial quota of eight repetitions of an exercise, to be raised one each 2 days, and the patient had progressed to fifteen repetitions before quota failure began, the newly adjusted quota could well be twelve, with an increment of one each 3 days. It is not always necessary to reduce the increment rate. If clinical judgment raises doubts as to sure patient success, that is a further option by which to provide additional successful exercise trials before the level at which quota failures began is again approached.
When there have been quota failures on more than one exercise, the same procedure is followed with each. The amount by which quotas are lowered and, if done at all, increment rates are reduced, can be orchestrated according to clinical judgment. It need not be the same or even proportional for each exercise with which the difficulties are occurring. The guiding principle is that the patient is being returned to a level at which, by his or her own recent performance, it has been demonstrated that success is assured. From that level the patient resumes working toward higher activity levels.
All of this should be explained to the patient in matter-of-fact terms. Repeated trials of successful exercise sessions, with rest and social response occurring contingent on that success, do permit learning or conditioning. A recycling to lower quota levels is simply a convenient way further to facilitate that. The essential elements to the process remain the same: rest and social response are programmed systematically. Working to tolerance is avoided.
When recycling of quotas to lower levels has occurred, eventually the performance barrier previously encountered will again be reached. No special preparation for that point need be made beyond that already carried out. Patients usually move past the barrier uneventfully. If they do not and repeated quota failures occur at or close to the original failure point, a second recycling should be carried out in the same manner as just described. Unless there is some correctable artifact in the situation, the correction of which promises further treatment progress, consistent quota failure at a given performance level strongly suggest that the patient has reached his or her ceiling for that exercise. If it is decided that the exercise should be continued for an indefinite period, for whatever reason, the quota should be lowered slightly to a level of sure success and kept at that level. Alternatively, the exercise may be discontinued.
The more likely correctable artifacts to check for include therapist nonperformance, family failure to reinforce properly, and some other temporary illness event. It may be a physiological limitation that additional rehearsal can be expected to overcome. In the latter case, the quota may be held constant at a level slightly lower than the failure point for a preset period such as a week. The patient having been informed of this at the start of the hold period, the quota can then resume climbing, although the increment rate may be reduced.
The process of adjusting quotas to deal with quota failures is illustrated by the case example material reported in Figure 2. The patient is the same person described in Chapter 5 in relation to the reduction of moaning behavior. It was necessary to adjust bicycle riding quota plans twice, as shown in Figure 2. The first quota began at a high level and had too rapid a rate of increase, 0.2 mile/day. After two successful days, the patient began to fail. Performance fell well below baseline levels. Quotas were then reset to begin below the level achieved when she was failing. The new increment rate was also reduced to 0.1. mile/day. This second quota plan was effective for 12 days. It brought her above her baseline average without a quota failure before she again began to fail to reach quotas. This time, as Figure 2 shows, failures were just below quota levels. When the patient had failed three consecutive trials, quotas were again reset. The therapist was conservative, probably more so than was necessary. She lowered quotas to the beginning point of the second quota plan (0.3 mile) and resumed the 0.1 mile/day increment rate from that point. A starting point of 1.0 might have worked as well, although, when in doubt, it is better to err on the conservative side. At any rate this second recycling of quotas was successful. The patient climbed to a level of 3.0 mile/day, a value more than double her baseline tolerance for the exercise, even while previously high medications were gradually being reduced to near-zero levels. When the 3.0 level was achieved, no additional increments were desired. The exercise was held at that level until completion of the program.
Pervasive and persistent failure to meet a spectrum of quotas may indicate that either a temporary or a more permanent performance plateau has been reached. The plateau may reflect the temporary influence of another illness event. Procedures for responding to that will be discussed. The temporary plateau may reflect an adverse balance between reinforcement for progress and activity versus reinforcement for pain behavior and continued functional impairment. A review of the progress of family retraining and of practicality of treatment goals should then be made. There is always the possibility, as well, that some change in the patient-therapist interaction accounts for the pause in treatment progress. For example, there may have been a reassignment of therapists or a reduction in therapist attention through double scheduling.
Extensive and persisting quota failures, particularly when judged as clinically to be premature, may, however, indicate that the treatment program is unable to arrange sufficiently effective reinforcement in a contingent manner. Reinforcers available for programming within the treatment setting may be insufficient. Sources of reinforcement previously sustaining operant pain behavior may not be sufficiently accessible for adequate change. The prospects to the patient for adequate posttreatment reinforcement may be too dim. Any mix of these may exist and render contingency management treatment inadequate to the task. When that happens, it usually means that there were some miscalculations or estimates in evaluation. Whatever the reason, it is prudent and appropriate to discuss the situation candidly with patient and spouse and to indicate that there is no point in proceeding further unless some change occurs. Treatment should then terminate unless they jointly and voluntarily express interest in an additional trial at treatment. Such a trial can be attempted, but criteria of progress should be specified. Unless certain mileposts are reached at agreed-on times, treatment should be discontinued. These criteria or mileposts must be stated in performance terms, not in subjective judgments by the patient or by professionals as to how the patient feels or how well he or she is progressing. Quotas are met without interruptions or they are not. The criteria or mileposts should represent an extension of the previous treatment plan, although with perhaps a mild lessening of increment rates.
Pervasive quota failures may indicate that the patient has reached an energy expenditure ceiling. That, in turn, may reflect a realistic physiological limit for that person. Occasionally, however, it suggests that antidepressant medications in the cocktail have been reduced too rapidly, resulting in a hopefully temporary limitation in the energy pool, which can be offset by reinstituting a higher level of the appropriate cocktail ingredient.
To summarize the issue of quota failures and what to do in response to them, there needs to be a weighing of several factors: physiological constraints, the adequacy of pacing and reinforcement within the exercise sessions themselves, and the degree to which the increased exercise and activity level achieved is in fact bringing the patient closer to effective posttreatrnent reinforcement. Some trial and error is often necessary to make these determinations. Trial-and-error explorations should continue to provide for periods of exercise-contingent rest and attention to permit testing the question of whether the problem is better characterized as operant or respondent.
Quota Ceilings and Movement Toward Other Forms of Activity
Ultimately, of course, all exercises will have a ceiling. In all cases, physiological constraints and medical prudence will impose upper limits. Those limits take precedence. So far as possible they should be estimated and defined at the outset of treatment. When they are approached as treatment progresses, ceilings should automatically be imposed. The exercise for which the ceiling has been set may then be discontinued or continued at a constant level.
Within those physiological and medical limits, there are several other factors to consider, A major objective of treatment is to bring each patient to a level of activity that permits entry into the activities or well behaviors expected in the posttreatment period. The exercise program has been a preparation for that and not an end in itself. As target levels of exercise and activity are approached, the program should begin to shift the content of activity. The shift is toward approximations of what the patient is expected to be doing after treatment. This is part of the process of generalization. Details as to its implementation will be reserved for Chapter 13, where other dimensions to the problem can also be brought into the picture. The issue for the moment is to anticipate that exercises will reach ceilings and, in most cases, will also be shifted into different forms to facilitate the maintenance of treatment gains.
Patients expected to have limited posttreatment social or vocational involvement (for example, those in the legitimated retirement group) often profit from an indefinite continuation of exercises. In those cases, prescribed exercise becomes a partial substitute for employment as a sustaining and contingently reinforced activity. In such cases, it becomes a matter of judgment as to whether to keep each exercise at a plateau, to provide for continuing increases in quotas, or even gradually to diminish them. Where exercises should continue to increase, increment rates probably should be extremely slow, such as one additional repetition beginning the first of each month. That sort of arrangement, when monitored by periodic clinic visits and/or by periodic return of diary and performance records for treatment staff review, provides continuing social reinforcement for persistent effort and for the signs of progress inherent in gradually increasing quotas.
Care must be exercised in prescribing posttreatment exercise to take into account the other demands being placed on the patient in the posttreatment environment. The combination of daily activity and prescribed exercise should be held to appropriate totals.
Quota Adjustments for Other Illness Events
Illness events will first be considered that are clearly separate from the pain problem, although they may involve pain as well, for example, influenza, a toothache, an ankle sprain, or whatever.
These kinds of problems present for the patient, as well as treatment staff, a task in discrimination learning, such as discriminating the ache of influenza from back pain or the pain of a toothache from joint pain. The discrimination is virtually always easy for both patient and staff. Complications to an operant conditioning program from these other illness events, aside from whatever temporary constraints are imposed on patient activity and participation in elements of the treatment process, usually arise from the medical and social responses they may precipitate. Those responses unfortunately risk being on a pain-contingent or illness-contingent basis. Medications and attention may again become enriched, illness-contingent consequences. Alternatively, the medical response can be matter-of-fact in style, without sacrificing thoroughness. Special procedures, examination or therapeutic, should first be explained carefully as relating specifically to the different or potentially different problem. They should then be carried out so far as possible within a time-contingent mode. (For example, “I am going to do this kind of examination, and if the findings are such and such, we will do this. If the findings are such and so we will do that.” The decision derived from the examination is not pain contingent.)
Treatment, particularly analgesics or narcotics, should be on a preset and predisclosed time-contingent basis. (For example, “For this toothache, we will administer such and such medication. You will receive it each 4 hours for x days after extraction of the tooth.”) Other examination or treatment procedures obviously widely separate from the pain problem can be carried out routinely with little likelihood that they will influence significantly the course of the operant program.
Curtailed activity resulting from other illness events may require the operant program to hold at a given level or even to retreat to an earlier level. If the interruption is brief, activity can probably pick up where it left off. When in doubt, after resolution of the interrupting problem, go back to a lower level. The guiding principle continues to be never to ask a patient to do something he or she cannot do. Stated another way, demands on the patient must surely be within reach.
Illness or pain events that may relate to or cannot be readily discriminated from the referring pain problem may be more difficult to handle. The patient referred with back pain, who announces one morning that the back pain is too severe to permit arising to go for treatment, is a case in point. There is always the question of whether the reported pain is the product of some new or altered state in the original pain problem, results from the onset of a new problem at a contiguous site, or is an expression of operant pain. Medical prudence and judgment are again the overriding factors. Further examinations may be carried out in the manner just described. That is, care is exercised to avoid letting especially solicitous attention serve as special encouragement for the patient to proceed with treatment, or to avoid it. Examinations are done matter-of-factly. The findings are then reported matter-of-factly. “The evidence indicates that there is (or may be) an additional problem for which (the following steps) will be carried out.” Alternatively, “The evidence indicates that there is not an additional problem about which we must be concerned. There is no need to postpone or alter treatment. We will proceed as scheduled.” In this connection, it is often useful, if supported by the available evidence, to remind the patient that it is often difficult to differentiate between pain as a feeling or distress from pain as an indicator that something adverse will happen if activity continues. The problem at hand is one that clearly will not result in further body damage if the prescribed exercise regimen is followed.
Programming Pain-Related Treatment Procedures
The issues and methods with pain-related treatment procedures are essentially the same as those described in dealing with noncocktail medications and the like in the preceding chapter. Like ethyl chloride spray or nerve blocks, heat, massage, transcutaneous stimulation, autogenic training, biofeedback-based muscle relaxant training, or other procedures may be used. Most of those procedures are simpler, less costly, and less time consuming than a fully programmed contingency management approach. If they offer promise of resolving the problem, they should probably receive a trial before embarking on an operant conditioning program. If they solve the problem, so much the better. If they do not, they can be abandoned. If they provide significant help but not as much as is hoped for, they may be woven into an operant program and continued, if programmed properly.
The underlying principle remains the same: specialized attention and procedures should not become systematically pain contingent. The procedures listed above, and others like them, used separately or concomitantly, should first receive baseline trials to estimate whether they have any helpful effect. If the evidence is promising, they can then move to a time-contingent schedule. The frequency and duration of the procedure is, from a learning viewpoint, of lesser importance. It can be dictated by the nature of the procedure and its observed or anticipated effects. What is important is that use of the procedure occurs on a preset schedule and not according to whether the patient feels a need for it.
The scheduling format may also be designed to strive for reduced utilization, that is, to work toward fading. The pain cocktail format can serve as a model. Initial sessions with the procedure can occur slightly more frequently than patient distress dictates. Between-session intervals can then gradually be increased on a predetermined schedule. For example, transcutaneous stimulation might have an aggregate daily use quota of x hours, which is to be reduced by 30-minute increments on a weekly basis.
REDUCING EXCESSIVE ACTIVITY LEVELS (THE PACER REGIMEN)
Some patients find relief from pain by movement or activity but in fact overdo, thereby aggravating the problem. Some of these patients with respondent pain problems experience pain and distress beginning only several hours after exercise. The delay of the aversive effects to exercise makes it more difficult to learn precisely how much one can do and still avoid severe pain. But ultimately, virtually every patient does learn that. Among those who experience pain on a delayed basis are some people who are particularly restless and active, perhaps a bit hyperactive. The combination of the lessened inhibitory power of delayed pain on activity and the strongly reinforcing characteristics of exercise and movement may lead to bursts of activity, which significantly worsen the pain problem. One possible objective of treatment with such patients is to develop more effective restraint or self-control in regard to a harmful exercise or to bursts of excessive activity.
There is a second type of pain problem that has features in common with the preceding example, Tense, restless, hyperactive people may develop muscle tension pain or spasm or both. Emotional tension or the manner in which activity is carried out may directly produce pain or conditions leading to it. Such people often have insufficient ability to achieve meaningful levels of muscle relaxation. If they could relax more effectively, they might ease or rid themselves of the pain problem.
Patients with either of these kinds of pain problems may profit from reduced activity level or its approximate reciprocal, increased effective relaxation. The kinds of problems referred to here were discussed in Chapter 3. The patients were characterized as pacers, that is, people who relieve pain by movement, not rest. They are to be differentiated from recliners, who rest to ease pain. The former group have high uptime values in their diary data and tend not to find rest reinforcing. Activity, even though it may lead eventually to pain, is potently reinforcing. If it were not reinforcing, they would not do it so much. In contrast recliners have low uptime values in their diary data (less than 80 hours/week), find rest reinforcing, and tend to realize less reinforcement from activity and exercise.
These kinds of problems were also touched on in the context of treatment goals (p. 182). It was pointed out there that relaxation training often has a role to play in treatment of pain. It was also noted at that point that biofeedback methods provide a direct approach to helping patients to achieve more effective and selective muscle relaxation. Generalized relaxation training, with or without use of hypnosis, may also prove helpful. Regardless of whether anyone or more of those approaches is helpful for a given patient, sometimes a problem of consistent or episodic excessive activity remains, or the reinforcers by which to keep the patient at the task of mastering deeper relaxation prove insufficient. What remains, in behavioral terms, is the desirability of selectively reducing and controlling activity and of increasing rest and relaxation. A regimen for working toward those treatment objectives will be outlined. It is a regimen that has received only limited clinical use. Little is known about how long the few successful trials with it have persisted. It is offered here with the suggestion that it be used only if the alternatives noted above have failed. It is more costly and time consuming for patient and professional, as well as having a limited clinical experience base.
Procedure for Reducing Excessive Activity
Target Behavior
Clinical experience suggests that the target behavior is more often a reduction of overall or general activity level than curtailment of a specific exercise or form of movement. However, either may occur, separately or together. Evaluation makes that determination. These two possibilities will be discussed in parallel here.
Baseline
For baseline information, two or more weeks of diary data identify the overall activity level and the average daily and weekly amounts spent reclining and sitting.
Diary data will serve also as the source of information about how much time is spent in the one or more activities specifically maintaining or aggravating the pain problem. It may be necessary to instruct the patient to record that activity in more detail than other elements of diary recording.
Contingency Management Program
Stated in the broadest possible terms, the contingency management program for increasing activity and decreasing rest, as outlined in the preceding section of this chapter, arranged things such that rest was earned by activity. Rest, observed to be a high-strength behavior from pretreatment diary data, became, in line with the Premack principle, the reinforcer by which to increase the lower-strength behavior, activity. That process is now to be reversed. Activity, demonstrated by diary data to be a high-strength behavior for the patient, is to he programmed to become contingent on increased amounts of the currently low strength target behavior, rest and relaxation.
Quotas should be set, based on baseline observations. The quotas are for uninterrupted periods of reclining or sitting (as may be indicated) before unrestricted activity, or access to the particular activity which is contributing to the problem, is permitted. Quota time amounts initially are within the range of quiet sitting or reclining demonstrated in baseline diary data. Quotas may then he raised at a preset rate.
It will be noted that rest or relaxation is almost impossible to measure in movement cycle terms, since, in this instance, it involves doing approximately nothing. It usually suffices in this case to rely on time measures.
Rest and relaxation periods may be enhanced or intensified in their effect by training the patient in relaxation skills and providing that the patient accrue x number of minutes of relaxation at a subjectively estimated level of depth, after which the reinforcer of activity becomes available. For example, a 10-point subjective scale may be developed with the patient. The high point, 10, represents maximum tension, and 1 becomes relaxation so low that it is achieved only by deep sleep. Intermediate points are then defined by the patient. The number 3 may, for example, be designated as a restful and relaxed level at which no muscle tension is felt. Given such a scale, baseline trials of relaxation periods are carried out. At fixed intervals (for example, each 60 seconds) the patient reports the level reached: 8, 6, 3, or whatever. That drill trains the patient to identify levels of relaxation. Subsequently, quotas are set such that, for example, a relaxation period is not to end until there have been a minimum of 10 minutes at level 6 or below. The next quota might be instituted a week later and require 10 minutes of level 5 or below, and so on.
The mechanics of quota setting and increment rates have already been described and should require no further elaboration here.
As intervals of relaxation increase, the undesired activity becomes less and less available. It sometimes happens that a patient may then engage in a furious burst of the undesired activity, using the lessened time available for it but producing as much or more of the disadvantageous effects. That immoderation becomes, however, a self-liquidating problem if the regimen is followed. The immoderation will interfere with reaching the required levels of relaxation during rest. Further extension of relaxation periods will then be required. The patient is forced by his or her own immoderation to pay a higher and higher price in terms of increasing rest and inactivity quotas. If, instead, the patient exercises with prudence during the unrestrained intervals, the success plateau is reached, and it is not necessary to increase further the time spent in rest and inactivity.
Commentary: Behaving Well: Motivating Patients to Increase Activity
In Chapter 10, Fordyce describes how to develop and supervise a treatment protocol for helping individuals with chronic pain increase their exercise and activity. As he points out in the beginning of the chapter, and as subsequent research has demonstrated [e.g., 3,5,7–9,17,47] exercise and activity play important roles in chronic pain management. When people are motivated to behave as if they are healthy – for example, by engaging in regular vigorous exercise – they view themselves and are treated by others differently than are individuals who behave as if they are disabled. People who view themselves and are treated by others as if they are well tend to maintain wellness. Moreover, people who maintain an appropriate level of exercise and activity are more likely to have the physical capability to engage in activities that are important to them, which provides them more opportunities for reinforcement and pleasure.
Fordyce notes that how people behave depends in large part on their past and current learning environment. Operant theory provides the principals needed to create a learning environment that motivates patients to change behavior; and Fordyce provides an eloquent description of the operationalization of those principals into clinical practice. This commentary focuses on what I view as a critical idea underlying the procedures Fordyce describes in Chapter 10: that the primary task of the pain clinician is not to provide knowledge or teach specific (pain or thought management) skills, but to motivate patients to change behavior. This idea continues to hold sway among many experts in the field [10,20,21,43]. As Fordyce often told patients, how well they manage pain depends much more on what they themselves do, than on what is done to them. The clinician’s role is to act in ways that will to make it easier for patients to behave well.
When “Behavioral Methods…” was written, the primary strategy clinicians used to motivate patients to change behavior was operant therapy. In the last 40 years or so, clinicians and scientists have made significant gains in the development of additional motivational strategies that can be used in conjunction with operant treatment. In this commentary, I review these newer approaches and the state of evidence regarding their efficacy, and discuss some specific motivational strategies that can be used as agents for positive change and patient wellness.
MOTIVATIONAL INTERVIEWING, GOAL PURSUIT INTERVENTIONS, AND FOCUSING ON VALUES-BASED GOALS
Seven years after Fordyce published Behavioral Methods for Chronic Pain and Illness, William Miller published an article describing a treatment approach based on what at the time was a controversial idea, but one completely consistent with an operant model [32]. This treatment, which he labeled Motivational Interviewing, was based on the idea that how a clinician communicates with patients can have a significant influence on whether or not that patient will change his or her behavior. “Motivation” does not lie only within the patient, but depends in large part on the patient/environment interaction. The impetus for the study and development of Motivational Interviewing came from Miller’s research on interventions to address problem drinking. He found that (1) participants in the control conditions who received minimal therapist attention and encouragement, along with a self-help book, evidenced significant improvement that was comparable to participants who received much more intensive treatment with a therapist who taught specific self-control strategies [e.g., 37,38] and (2) in both treatment conditions, therapist behavior (e.g., frequency of reflective listening) accounted for very large amounts of the variance of outcome at 6 months and even up to 2 years after treatment [33].
These findings encouraged Miller and his colleagues to search the research literature and identify therapist behaviors that predicted clinical trial outcomes. A list of clinical strategies to use (i.e., clinician behaviors associated with positive outcomes) and to avoid (i.e., clinician behaviors associated with negative outcomes) were combined into a treatment package that was hypothesized to maximize the chances for positive patient behavior change [34].
The key Motivational Interviewing strategies Miller and colleagues identified included: (1) using a patient-centered approach – demonstrating an interest in understanding the problem from the patient’s point of view by asking open questions and listening carefully to the patient’s response; (2) expressing empathy and warmth; (3) enhancing patient awareness of discrepancies between behaviors thought to be contributing to the problem (e.g., problem drinking, smoking, and in the context of chronic pain, inactivity or over-activity) and the patient’s values; (4) enhancing confidence and self-efficacy for behavior change using open questions and reflective listening; and then, once the patient expresses a readiness to change, (5) developing a very specific action plan [35].
A great deal of research has examined the efficacy Motivational Interviewing. The approach has been applied to numerous problem behaviors and evidence supports the efficacy of Motivational Interviewing not only for reducing problem drinking [44], but also for reducing the frequency or severity of problem gambling [11], unprotected sexual acts [28], substance abuse in adolescents [19], problem eating [2], and smoking [18], and increasing exercise behavior [6].
In the last 2 years, controlled trial research on Motivational Interviewing has expanded to the area of chronic pain, with very promising results. For example, Vong and colleagues compared the efficacy of conventional physical therapy alone versus physical therapy plus motivational enhancement therapy (a manualized Motivational Interviewing approach) in 76 individuals with low back pain [46]. The investigators assessed motivation-enhancing factors (proxy efficacy, working alliance, and outcome expectancies), pain intensity, disability, lifting capacity and exercise compliance. They found that the group that received motivational enhancement therapy evidenced significantly larger improvements in the motivation-enhancing factors, lifting capacity, and exercise compliance than the group that received physical therapy alone. Trends were also found for greater improvement in the Motivational Interviewing conditions for pain intensity and disability.
Thomas and colleagues examined the efficacy of Motivational Interviewing and an education intervention targeting attitudinal barriers to cancer pain management, relative to standard care, in a sample of 318 adults with a variety of cancer diagnoses [40]. Although attitudinal barriers did not change significantly in participants assigned to any of the three conditions, only the participants randomized to the Motivational Interviewing condition reported significant improvements in pain interference, general health, vitality, and mental health.
Ang and colleagues randomly assigned 216 individuals with fibromyalgia to either 6 sessions of Motivational Interviewing targeting an increase in exercise and activity or 6 sessions of training in pain self-management strategies [1]. More of the participants who received Motivational Interviewing reported clinically meaningful improvements in physical activity at the 6-month follow-up point than the participants who received the control intervention. Moreover the participants who received Motivational Interviewing evidenced larger increases in the number of hours of physical activity immediately post-treatment, and reported greater pain reductions at post-treatment and at 3-month follow-up than those assigned to the control condition. Similarly, Tse and colleagues randomly assigned 56 older adults to 8 weeks of an integrated Motivational Interviewing and physical therapy treatment program or a control condition of regular physical therapy. They found significant pre- to post-treatment improvements in measures of pain intensity, pain self-efficacy, anxiety, happiness and mobility in the participants assigned to the Motivational Interviewing condition, and significant improvements only the happiness measure in the control condition participants [41].
In a study of martial interaction patterns, L. R. Miller and colleagues randomly assigned couples who had completed surveys about pain, mood, marital satisfaction, and empathy to either (1) a Motivational Interviewing tailored feedback session regarding their marriage and pain coping or (2) an education session about the gate control theory of pain [31]. Following the single-session interventions, all participants reported an increase in empathy toward their partner except for the spouses assigned to the control condition.
Not all published studies report significant benefits of Motivational Interviewing, however. Kerns and colleagues randomly assigned 161 veterans with low back pain either standard cognitive behavioral therapy or a tailored cognitive behavioral therapy intervention for pain management [23]. The tailored intervention incorporated patient preference for learning specific skills for pain management and also incorporated motivational interviewing strategies targeting treatment engagement and participation. However, participants in both conditions evidenced a very high level of treatment engagement throughout treatment; the tailored approach did not increase this any further.
Noting that Motivational Interviewing involves a number of therapist skills and techniques, Christiansen and colleagues sought to develop and test a brief (two 30-minute sessions) motivational treatment [10]. This treatment, labeled a “goal-pursuit” intervention, included a number of Motivation Interviewing strategies for increasing physical capacity in patients with chronic back pain. In the first session, patients were encouraged to identify and elaborate on both the benefits and barriers associated with implementing specific goals (e.g., exercise) related to exercising regularly. Consistent with Motivational Interviewing principals, the clinician’s role was to help focus and facilitate discussion towards a goal of increasing the patient’s commitment to improve physical capacity while ensuring that all of the ideas were elicited from rather than provided to the patient. In the second session, patients were encouraged to identify strategies – and then develop very specific plans (“implementation intentions”) – for dealing with barriers that might interfere with goal achievement. The study participants were assigned to receive standard treatment alone (6 hours of physical therapy per day for 3 weeks) or standard treatment plus the motivational intervention. Three weeks after treatment, participants in the treatment group had increased their physical capacity significantly more than participants in the control group on both observational/behavioral and self-report measures.
Finally, in the last several years, a group of cognitive-behavioral therapies has emerged that focus less on analyzing and problem solving as strategies to address problems – including pain – and more on experiential approaches that alter how one responds to symptoms and suffering [30]. Prominent among these is Acceptance and Commitment Therapy (ACT) [15,16], which includes as one of its core features an explicit focus on exercises that encourage movement towards highly valued goals, as opposed to exercises or techniques that seek to avoid something viewed as aversive [29]; for example, behaving in ways consistent with being a loving parent rather than engaging in activities that will reduce pain. ACT can therefore be viewed as having motivational components (although it might not necessarily be viewed by proponents as primarily a motivational intervention).
In sum, there has been continued and growing interest in the field regarding the critical role that patient motivation plays in successful pain management. Experts emphasize the fact that clinicians influence patient motivation. Although operant strategies, as so clearly and elegantly described by Fordyce, can and should be used to help motivate patients to exercise and to regulate their activity appropriately (because there is now doubt that it is effective), clinicians need not limit themselves to using only operant treatment. The next section provides brief summary discussion regarding the strategies that appear central to contemporary motivational treatments.
INTEGRATING PATIENT-CENTERED AND VALUES-BASED MOTIVATIONAL APPROACHES INTO OPERANT TREATMENT
There is not adequate space for this commentary to describe each values-based, patient-centered, and goal-pursuit strategy that clinicians could potentially use to enhance patient motivation for change. My hope is that this commentary, at least in part, encourages the reader to consider exploring the work of others who have written in more detail on this topic than is possible here [29,36]. However, there are some key strategies that are used by many motivational approaches that work well in conjunction with operant treatment. In fact, a number of these can be seen in the way that Fordyce describes his application of operant treatment in Chapter 10; and many who were lucky enough to observe Fordyce work clinically will recognize that he regularly used a number of these strategies himself in his clinical work, even if he did not explicitly write about them. These strategies include: (1) providing the patient with regular reinforcement in the form of praise and affirmations; (2) developing and maintaining a strong working alliance with the patient; (3) asking open questions to elicit the patient’s ideas and thoughts regarding treatment and behavior change – ideas and thoughts that can then be reinforced with reflection and praise; (4) avoiding the temptation to provide information by lecturing patients – instead clinicians can teach with stories and metaphors; and (5) linking treatment goals to what is most important to the patient.
REINFORCEMENT, PRAISE, AND AFFIRMATIONS
Reinforcement works. Research has confirmed that systematic reinforcement of both verbal and non-verbal pain-related behaviors increases patient ratings of pain intensity and neurophysiological correlates of pain (e.g., cortical pain responses) [4,13,22,25,26], and that reinforcement of wellness-related behaviors increases well behaviors and decreases pain reports [14,25]. This is the central rationale supporting operant treatment. Given the efficacy of reinforcement as a key motivating force, clinicians should pay very close attention to what the patient says and does, and apply verbal reinforcement and praise liberally as the patient takes steps towards goal attainment.
Providing praise in the form of affirmations is a core skill of Motivational Interviewing [36]. As Miller and Rollnick note, affirmations (which “… recognize and acknowledge that which is good including the individual’s inherent worth as a fellow human being”; page 64, [36]) can serve a number of important functions, each of which can enhance outcomes. The positive emotions that often result from effective affirmations tend to be reciprocal; clinicians who affirm patients are listened to and trusted more than clinicians who are less affirming. The impact of clinicians’ comments to patients is influenced, at least in part, by the number and quality of the affirmations they provide. Affirmations can therefore facilitate engagement and continued treatment participation.1
Affirmations can also reduce general defensiveness and thereby increase patient openness to new ideas and (to what might otherwise be considered) threatening information. Affirmations need not come only from clinicians, nor will those coming from clinicians always be the most effective. Clinicians can also encourage patients to affirm themselves by asking patients to describe their strengths and previous successes.
DEVELOP AND MAINTAIN A STRONG WORKING ALLIANCE
The research findings on the benefits of therapeutic alliance are consistent and clear; measures of therapeutic alliance during treatment predict subsequent outcomes following therapy [27]. Engaging the client in a collaborative working relationship is another core process in Motivational Interviewing. Perhaps the most important clinician skill related to building a strong working alliance is the clinician’s ability to listen to the patient; and not only just the words. Fordyce often noted both the “lyrics” and the “music” to what patients said.
Once the clinician has a sense of what the patient has communicated via words, voice tone, and non-verbal behaviors, the motivational clinician can reflect back what the patient might have meant. The real skill – and it is a skill that increases with practice – is determining which of the many (sometimes contradictory) ideas, thoughts, and feelings to reflect [36]. Simply repeating back exactly what a patient says or parroting the patient is rarely helpful, and does not usually contribute to forward movement. But jumping too far ahead too soon can backfire and create resistance.
The most effective reflection is usually a statement indicating a sort of “next step” towards the adaptive goal. A patient says, “I am thinking I should start getting serious about exercising.” A parroting response would be, “You are thinking about starting an exercise program.” More helpful reflections to keep the patient on track while eliciting for moving forward might include, “You now feel ready to design an exercise program you can commit to,” or “You have some specific ideas about how much you want to exercise and when.”
ASK OPEN QUESTIONS AND REFLECT RESPONSES
Motivation theories hypothesize that two elements mush be in place before an individual will choose to engage in a behavior: he or she must view the behavior change as important, and must believe that the behavior change will contribute to some valued outcome [20]. Therefore, a motivational clinician seeks to enhance both the confidence in and importance of an adaptive behavior change at every opportunity [36]. One effective way to achieve these goals is to listen carefully to what patients tell us about importance and confidence, and then encourage discussion of those ideas that reflect higher levels of both importance and confidence, given that people are much more likely to believe what they themselves say than what is said to them [12].
In order to be able to reflect expressed thoughts regarding either or both importance and confidence, the clinician needs to encourage the patient to talk. Open questions – questions that elicit a sentence or paragraph rather than a single 1-word yes or no response – are excellent for encouraging patients to talk about different topics. The motivational clinician will have a number of these open questions ready and on hand when working with patients. These include questions such as, “What are the things you have done in the past to start and maybe even maintain an exercise program?”, or “I’d be interested to know what benefits you yourself see in walking for at least a mile almost every day?”, or even, “You told me you were thinking about exercising more. What would it take for you to change from thinking about this to taking some steps to successfully do this?”
The key here is to elicit from the patient his or her own ideas and thoughts about the benefits of behavior change and the factors that will make it possible in his or her life situation. Once these ideas are expressed, the clinician can reflect them back (which communicates to the patient that the clinician is paying attention, and therefore that the patient is valued), and encourage more discussion; “You told me that you think that if you walk every day or almost every day you’ll have more energy and feel more confident. What might be some of the effects of this on other parts of your life?”
TEACH WITH STORIES AND METAPHORS
Fordyce liked to say that “information is to behavior change as spaghetti is to brick.” He noted that millions of smokers know that smoking is dangerous for their health; this information alone is not enough to motivate many of them to stop smoking. He knew that lecturing patients, in the guise of “providing information” tended to have little impact on behavior.
On the other hand, Fordyce was a master at communicating via stories and metaphors. Two of his favorites for communicating (1) the importance of focusing on behavior change over pain reduction and (2) for the need to change behavior when the problem is not resolving were to tell patients that “Focusing on pain reduction before you get back to [gardening, work, dancing] is putting the cart before the horse”, and, “You know the rule of holes? If you find yourself in a hole, stop digging.” He would often tell stories from his life or from interactions with previous patients, “You know, I worked with a patient once who had a problem much like yours….” He viewed these as a way to provide behavioral modeling (an environmental factor known to influence patient behavior), and give patients ideas for expanding their behavioral repertoire in adaptive ways.
Metaphors and metaphoric language are a key component of ACT treatment [16]. Like some of the key Motivational Interviewing skills, metaphors provide ideas for behavioral change without being explicitly proscriptive. They are only stories; hardly even suggestions. Moreover, as Hayes and colleagues point out, metaphors tend not to reflect linear logic, but are more like verbal pictures [16]. As such, they provide an opportunity for the patient to experience a new idea directly, as opposed to logically considering it. Finally, metaphors can be easily remembered, and are therefore useful across many situations, or for addressing the situation or issue over time. As non-linear verbal communications, metaphors are also often used in hypnosis and hypnotic language [45,48], and there is some evidence that metaphors are more effective in promoting behavior change than direct (linear, logical) suggestions [39]. While I am aware of no evidence that the use of metaphorical language will necessarily improve outcomes beyond the benefits of communications that do not contain metaphors, the fact that cognitive behavioral therapy with hypnosis is more effective than cognitive behavioral therapy without hypnosis [24] and that ACT theory argues for the beneficial roles for metaphors [16] provide at least some preliminary support for their benefits. In addition, they provide the opportunity for clinicians to use additional creative skills, which can make the therapeutic process more interesting (and perhaps more fun) for clinicians and patients alike.
LINK TREATMENT GOALS TO PATIENT VALUES
A final motivational strategy that I would like to emphasize is that of linking treatment goals to what is most important to the patient. Fordyce hinted at this when he mentioned that increases in exercise and general activity are a part of patients getting back to activities such as “gardening and dancing” in Chapter 10.
Values-based treatment is central to both Motivational Interviewing and ACT. In Motivational Interviewing, Miller and Rollnick note that a person’s values are the central key to what motivates them. Importantly, and based on Festinger’s cognitive dissonance theory [12], people are strongly motivated to change attitudes or behavior in order to reduce the perceived discrepancies between their current actions and values and their beliefs regarding the consequences of those actions. For example, parents place a great deal of value on their children’s health. When this value is discussed in the same conversation as the impact of second hand smoke, it will increase the probability that the parent either quit smoking, or at least smoke outside of the home. Thus, not only does the motivational clinician seek to understand the patient’s most important values, but that clinician also invites patients to consider and discuss the implications of their behavior (exercise, eating, drinking, and smoking habits, etc.) with respect to their most deeply held values [36]. In ACT and Contextual Cognitive-Behavioral Therapy, the patient’s values also play a central role in guiding treatment goals [16,29].
CONCLUSIONS AND SUMMARY
As Fordyce knew, people with chronic pain do much better when they behave well. But behavior change is difficult. Mark Twain wrote, “…the only way to keep your health is to eat what you don’t want, drink what you don’t like, and do what you’d rather not” (p. 291, [42]).
Operant theory provides very clear guidance regarding how to develop a treatment program to make behavior change easier for patients. In the past four decades, clinicians who also focus on patient motivation as key to behavior change have developed additional strategies for influencing behavior change. Although evidence supports the efficacy of operant treatment of pain [4,13,14,22,25,26], evidence also supports the efficacy of these new approaches [1,2,6,10,11,18,19,23,28,31,40,41,44,46].
To the extent that a clinician wishes to enhance patient motivation, he or she would do well to: (1) provide steady and consistent reinforcement for successful steps towards behavioral change (as Bill Miller once told me, “Come unglued with praise”); (2) seek to maintain a strong working alliance with the patient; (3) ask open questions and reinforce those ideas and thoughts that are consistent with confidence and importance of the goal; (4) provide new ideas using stories and metaphors instead of lecturing; and (5) become aware of the patient’s most valued goals, and use these to inform treatment.
Motivation to change is not just something that lies inside the patient. It is strongly influenced by the actions of clinicians. Our task is to use our knowledge about what facilitates change to create an environment in which patient behavior change is more likely. As we adjust our behavior, we will see our patient’s behavior change as well.
REFERENCES
1. Ang DC, Kaleth AS, Bigatti S, Mazzuca SA, Jensen MP, Hilligoss J, Slaven J, Saha C. Research to encourage exercise for fibromyalgia (REEF): use of motivational interviewing, outcomes from a randomized-controlled trial. Clin J Pain 2013;29:296–304.
2. Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev 2011;12:709–23.
3. Bartels EM, Lund H, Hagen KB, Dagfinrud H, Christensen R, Danneskiold-Samsoe B. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev 2007(4):CD005523.
4. Becker S, Kleinbohl D, Klossika I, Holzl R. Operant conditioning of enhanced pain sensitivity by heat-pain titration. Pain 2008;140:104–14.
5. Bertozzi L, Gardenghi I, Turoni F, Villafane JH, Capra F, Guccione AA, Pillastrini P. Effect of therapeutic exercise on pain and disability in the management of chronic nonspecific neck pain: systematic review and meta-analysis of randomized trials. Phys Ther 2013;93:1026–36.
6. Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol 2003;71:843–61.
7. Busch AJ, Schachter CL, Overend TJ, Peloso PM, Barber KA. Exercise for fibromyalgia: a systematic review. J Rheumatol 2008;35:1130–44.
8. Bystrom MG, Rasmussen-Barr E, Grooten WJ. Motor control exercises reduces pain and disability in chronic and recurrent low back pain: a meta-analysis. Spine (Phila Pa 1976) 2013;38:E350–8.
9. Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med 2007;147:492–504.
10. Christiansen S, Oettingen G, Dahme B, Klinger R. A short goal-pursuit intervention to improve physical capacity: a randomized clinical trial in chronic back pain patients. Pain 2010;149:444–52.
11. Cowlishaw S, Merkouris S, Dowling N, Anderson C, Jackson A, Thomas S. Psychological therapies for pathological and problem gambling. Cochrane Database Syst Rev 2012;11:CD008937.
12. Festinger L. A theory of cognitive dissonance. Evanston, Ill.: Row; 1957.
13. Flor H, Knost B, Birbaumer N. The role of operant conditioning in chronic pain: an experimental investigation. Pain 2002;95:111–8.
14. Fordyce WE, Fowler RS, DeLateur B. An application of behavior modification technique to a problem of chronic pain. Behav Res Ther 1968;:105–7.
15. Hayes SC. Acceptance and Commitment Therapy, Relational Frame Theory, and the third wave of behavioral and cognitive therapies. Behav Ther 2004;35:639–64.
16. Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experitiential approach to behavior change. New York: Guilford Press; 1999.
17. Henschke N, Ostelo RW, van Tulder MW, Vlaeyen JW, Morley S, Assendelft WJ, Main CJ. Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev 2010(7):CD002014.
18. Hettema JE, Hendricks PS. Motivational interviewing for smoking cessation: a meta-analytic review. J Consult Clin Psychol 2010;78:868–84.
19. Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: a meta-analytic review. J Consult Clin Psychol 2011;79:433–40.
20. Jensen M, Nielson WR, Kerns RD. Toward the development of a motivational model of pain self-management. J Pain 2003;4:477–92.
21. Jensen MP. Enhancing motivation to change in pain treatment. In: Turk DC, Gatchel RJ, editors. Psychological treatment for pain: A practitioner’s handbook. New York: Guilford Press; 1996. p. 78–111.
22. Jolliffe CD, Nicholas MK. Verbally reinforcing pain reports: an experimental test of the operant model of chronic pain. Pain 2004;107:167–75.
23. Kerns RD, Burns JW, Shulman M, Jensen MP, Nielson WR, Czlapinski R, Dallas MI, Chatkoff D, Sellinger J, Heapy A, Rosenberger P. Can We Improve Cognitive-Behavioral Therapy for Chronic Back Pain Treatment Engagement and Adherence? A Controlled Trial of Tailored Versus Standard Therapy. Health Psychol 2013. In Press.
24. Kirsch I, Montgomery G, Sapirstein G. Hypnosis as an adjunct to cognitive-behavioral psychotherapy: a meta-analysis. J Consult Clin Psychol 1995;63:214–20.
25. Linton SJ, Gotestam KG. Controlling pain reports through operant conditioning: a laboratory demonstration. Percept Mot Skills 1985;60:427–37.
26. Lousberg R, Groenman NH, Schmidt AJ, Gielen AA. Operant conditioning of the pain experience. Percept Mot Skills 1996;83(3 Pt 1):883–900.
27. Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. J Consult Clin Psychol 2000;68:438–50.
28. Mbuagbaw L, Ye C, Thabane L. Motivational interviewing for improving outcomes in youth living with HIV. Cochrane Database Syst Rev 2012;9:CD009748.
29. McCracken LM. Contextual cognitive-behavioral therapy for chronic pain. Seattle: ISAP Press; 2005.
30. McCracken LM, Vowels KE. Acceptance and Commitment Therapy and mindfulness for chronic pain: Model, process, and progress. American Psychologist in press.
31. Miller LR, Cano A, Wurm LH. A motivational therapeutic assessment improves pain, mood, and relationship satisfaction in couples with chronic pain. J Pain 2013;14:525–37.
32. Miller WR. Motivational interviewing with problem drinkers. Behavioural Psychotherapy 1983;11:147–172.
33. Miller WR, Baca LM. Two-year follow-up of bibliotherapy and therapist-directed controlled drinking training for problem drinkers. Behav Ther 1983;14:441–8.
34. Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. J Consult Clin Psychol 1993;61(3):455–61.
35. Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991.
36. Miller WR, Rollnick S. Motivational interviewing: helping people change. New York, NY: Guilford Press; 2013.
37. Miller WR, Taylor CA. Relative effectiveness of bibliotherapy, individual and group self-control training in the treatment of problem drinkers. Addictive Behaviors 1980;5:13–24.
38. Miller WR, Taylor CA, West JC. Focused versus broad spectrum behavior therapy for problem drinkers. J Consult Clin Psychol 1980;48:590–601.
39. Santarpia A, Blanchet A, Mininni G, Andrasik F, Kwiatkowski F, Lambert JF. Effects of weight-related literal and metaphorical suggestions about the forearms during hypnosis. Int J Clin Exp Hypn 2010;58:350–65.
40. Thomas ML, Elliott JE, Rao SM, Fahey KF, Paul SM, Miaskowski C. A randomized, clinical trial of education or motivational-interviewing-based coaching compared to usual care to improve cancer pain management. Oncol Nurs Forum 2012;39:39–49.
41. Tse MM, Vong SK, Tang SK. Motivational interviewing and exercise programme for community-dwelling older persons with chronic pain: a randomised controlled study. J Clin Nurs 2013;22:1843–56.
42. Twain M. Following the equator. Washington, DC: National Geographic Society, 2005.
43. Van Damme S, Crombez G, Eccleston C. Coping with pain: a motivational perspective. Pain 2008;139:1–4.
44. Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol 2006;41:328–35.
45. Vlieger AM, Menko-Frankenhuis C, Wolfkamp SC, Tromp E, Benninga MA. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology 2007;133:1430–36.
46. Vong SK, Cheing GL, Chan F, So EM, Chan CC. Motivational enhancement therapy in addition to physical therapy improves motivational factors and treatment outcomes in people with low back pain: a randomized controlled trial. Arch Phys Med Rehabil 2011;92:176–83.
47. Waller B, Lambeck J, Daly D. Therapeutic aquatic exercise in the treatment of low back pain: a systematic review. Clin Rehabil 2009;23:3–14.
48. Zimmerman J. Cleaning up the river: a metaphor for functional digestive disorders. Am J Clin Hypn 2003;45(4):353–9.
The so-called Operant Activity Training (OAT) program that Fordyce pioneered in Chapter 10 is one of the most widely used parts of his book and is a cornerstone in most pain rehabilitation programs today. In this commentary, I will attempt to cast the chapter in a fresh light in three ways. First, I will contend that modern conceptualizations of disability, based on the evidence, provide vital nuances concerning when, whom, and why the OAT program might best be employed. There is evidence that there are important subgroups of patients and that certain aspects of OAT, such as dealing with avoidance, may be more important than others. Second, new models have highlighted certain mechanisms that appear to be central for success. In a nutshell, I will assert that the essence of the treatment for “activity” should be some form of exposure. Third, when we consider subgroups and OAT, early, preventive interventions for chronic pain are possible. Even here, exposure is a key aspect for certain subgroups of patients who are worried, fearful or distressed.
In the other commentary for this chapter, Jensen convincingly speaks of promoting patient’s well behavior, i.e., that they “behave well.” In this commentary, I recommend also that clinicians learn to “expose well.” That is, we clinicians need to assist patients in learning to behave well, by systematically promoting exposure. We need to help them to overcome their fears and worries about usual physical activities. In this commentary we will examine these three contentions in more detail to see how they help to improve our understanding of OAT programs and how they may impact on intervention outcomes. First, however, I present a short recapitulation of the basic ideas in OAT.
BASIC TENETS OF OAT
One of the great contributions of Fordyce’s book is the development of the underlying conceptualization of chronic pain disability. This significantly changed how we think about chronic pain and thereby opened new doors for treatment. We cannot overestimate the importance of this. It catapulted us from a neurophysiological view of pain to a biopsychosocial one. The development of disability is eloquently described in the book and bears great relevance for Chapter 10 and this commentary. The description is based on learning theory according to which behavior is influenced by the environment and in particular by its consequences.
Fordyce highlights a combination of learning mechanisms as contributors, in whole or in part, to the development of disability. Briefly, he states that in the acute phase, normal activities may be punished since they sometimes provoke the pain. Further, he describes how rest and other behaviors that are incompatible with “usual” activities (these are often passive behaviors like reading, listening to the radio) may be positively reinforced by attention from others as well as by the enjoyment they provide. Thus, “rest” or “other activities” may take precedence over “usual” activities. Indeed, Fordyce described how pain may buy a “time-out” from ordinary boring or aversive things. Pain behaviors like grimacing or complaining about pain may also be reinforced by the sympathy, help, and treatment they procure. Finally, he describes how avoidance behaviors may develop, although he places less emphasis on these than on the aforementioned learning principles. In Fordyce’s description he speaks of various behaviors such as those associated with particular activities or movements which are implicated in or associated with pain avoidance. This is been a strong focus of research over the past few years [53]. Moreover, Fordyce’s description of how these may contribute to chronic pain over time is illuminating and persuasive.
From this basic analysis of the problem, the OAT program was shaped and developed. It aims to focus positive reinforcement on activities (not pain behaviors) and to utilize a systematic and gradual increase in goal-related activities to achieve normal function. Thus, activity training starts at current levels and gradually increases. Progress is carefully monitored and graphical feedback, verbal praise, and the satisfaction of participating in the activity (i.e. innate reinforcement) are used to reinforce improvements.
Although the activity program described by Fordyce in Chapter 10 appears simple, utilizing it fully is a challenge requiring considerable competence. In fact, the program employs a large number of sophisticated methods from a medical as well as a psychological perspective. Therefore, it is worth considering which professionals, with which competencies might adequately use the program. Unfortunately, no system to monitor or provide feedback has been developed as yet to maintain and enhance high quality implementation.
FROM INACTIVITY TO EMOTIONAL DISTRESS: SUBGROUPING
While the original OAT program was aimed at activity levels of severely disabled patients, there is reason to believe that its application today can benefit from a broader perspective that includes subgrouping based on emotional risk factors. This is especially relevant since the program has been expanded to include more heterogeneous populations that underscore an appreciation of subgroups. Reviews after the Fordyce book began to be implemented in the clinic showed that multidimensional or cognitive-behavioral treatment (CBT) programs, where OAT might be a cornerstone, indicated large increases in activity levels [9,10,11,20,24,25,38,50,51], but more recent systematic reviews report a negligible effect size on disability when behavioral or CBT is compared to active controls [57]. While explanations e.g., “drift” (i.e., gradual changes over time) in its application (or its elimination from pain programs altogether) warrant exploration, our knowledge about the actual effectiveness of OAT is in fact shockingly limited, because only a few studies have isolated it separately from other interventions included in a package treatment program. Similarly, the OAT program itself contains several components e.g., social reinforcement for activity, a quota system, graphical feedback, withholding social reinforcement for pain behavior, and goal setting. While all of these components warrant research, only a few studies have attempted to investigate them [33,34].
Over the past decades, negative emotions such as fear, worry and depression have been shown to be associated with the development of persistent pain as well as to poor treatment outcomes both as mediators and moderators. Indeed, extensive research boils down to some key psychological factors [40] that include catastrophizing, self-efficacy beliefs (e.g., low expectations for treatment success), fear, avoidance, coping strategies (e.g., problem solving, active confrontation, acceptance), and depression [6,26,29,37,40,42,43,48,49]. While the research identifies various types of psychological factors, a good proportion deal with emotion and taken together the research has stimulated helpful models of disability. Research over the past 30 years has focused on behavioral, cognitive, or emotional factors, but there has also been considerable theoretical interest in how these factors interact in various combinations.
One integrative model that has received considerable attention, is the Fear-Avoidance Model [53]. This model proposes that disability may be driven by a process where pain catastrophizing and fear play a major role. Namely, the model shows that pain may result in catastrophic worry [8] that is associated with fear which increases hypervigilance and leads to avoidance behavior. Movements believed to be a threat (e.g., a threat of injury) are avoided which in turn is related to disuse, depression, and disability. This process in turn increases the perception of pain thus creating a vicious circle. Research currently shows that the components in the model are related to a range of negative outcomes [1,12,23,58].
In light of the identified risk factors and the models available, it has become apparent that there are considerable individual differences in how people react to pain and the “one size fits all” approach to the treatment of disability is unlikely to optimize outcomes. For best results it would seem that the OAT program needs to be tailored to the existing subgroups of patients e.g., in terms of goals, the increments for increasing them, and the reinforcement provided. First, subgroups of patients respond more or less successfully to given treatments e.g., OAT. We have found for example, that patients with a profile of high levels of distress, fear and catastrophizing do poorly in operant activity programs conducted in primary care [56]. Likewise, depression that is not eliminated during rehabilitation has been shown to have a very negative effect on the outcome of pain rehabilitation programs that feature OAT [46,47]. Second, patient subgroups or profiles can be identified. Studies consistently classify groups of patients for example where avoidance is central [22,31] or where various combinations of catastrophizing and depression exist [3]. Moreover, without specific treatment these subgroups are at risk for poor outcomes. However, basing these subgroups or profiles primarily on self-reports, rather than behavior, may introduce variability and problems with reliability and validity. Third, new models suggest other psychological profiles of relevance. As an illustration, the Endurance Model was developed as an extension of the Fear-Avoidance model and highlights a subgroup of patients who persist (rather than avoid) in activities, despite pain, in order to maintain performance, but where this persistence instead disrupts healing and contributes to the development of chronic pain [15,16]. To date, the operational definition of “endurance” is also based on self-report with the inherent problems noted above. Thus, the literature points to the need to tailor operant treatment to certain subgroups based on the psychological mechanisms involved [45], as well as a need to be able to more objectively define them e.g., with observable behavior.
When patients show evidence of disability as measured by low activity levels the problem is often complicated by the co-occurrence of emotional problems. Persistent pain-related disability is often a bedfellow with anxiety, depression, worry, distress, anger, fear or frustration. Recently, it has been suggested that there may be psychological mechanisms associated with both the pain and the emotional problem [27]. For example, pain and depression may be maintained when normal flare-ups of pain stimulate catastrophic worry that in turn taxes the patient’s ability to regulate negative affect [29]. If emotion regulation skills (e.g., distraction, mindfulness, or problem solving) do not meet these demands then a vicious circle may be stimulated where the emotion causes more catastrophic worry and symptoms which in turn further tax the regulation of the emotions. As a result, emotions may be vitally associated with the pain and disability problem. Indeed emotional dysregulation has been identified as a possible core mechanism underpinning chronic pain (See the commentaries by Lumley and Main on Chapter 2.) This suggests that treatments will likely need to take this into consideration to be effective.
EXPOSING WELL: THE NEED FOR EXPOSURE
For many subgroups with co-occurring emotion and pain, exposure to various stimuli will be an important form of treatment. The Fear-Avoidance Model for example suggested that exposure to reduce “fear of movement” could be an effective treatment of activity disability for selected patients [54]. Exposure treatment is based on respondent learning and much like treatments for phobias involves the gradual (hierarchical) “exposure” to the feared object [54]. A key element is that exposure provokes fear and is maintained until the fear subsides, i.e., the fear is extinguished. As predicted, the exposure in-vivo method developed for painful movement has shown considerable promise in randomized controlled trials [1,35,54]. Thus, increasing activity levels is tied to discovering what is being avoided and then systematically applying exposure to extinguish the fear. In the clinic, this is often combined with elements of the OAT program to provide reinforcement for increases in goal-oriented activities. It is also tied to discovering the limits an ongoing disease process may or may not have on a particular activity. As an illustration, by reducing fear and anxiety about injury, patients suffering arthritis can evaluate the influence the activity has on, for example, their experienced pain, swelling, and well-being.
In light of research published since Fordyce’s book appeared in 1976, a key feature of current approaches to activity training is that it should invite exposure. Patients may “behave well” in Jensen’s terms by participating in activities they previously enjoyed and motivational processes such as goal orientation can clearly be utilized to enhance this also as outlined by Jensen in his commentary in this book. However, we clinicians similarly need to “expose well” to provide the best possible treatment for increasing activity and decreasing disability. When dealing with a subgroup fitting the fear-avoidance model, this would mean using the exposure protocol that focuses on fear of pain and painful movement [54].
Fear is not the only form of distress. The number of patients fulfilling the criteria for exposure focusing on fear of movement is not known. Using criteria of low levels of activities, and high levels of catastrophizing or fear of movement, we found that about one-third of those seeking help for persistent musculoskeletal pain fulfilled them [31]. Other forms of emotional distress are also prevalent. To deal with low levels of activity in patients with other types of distress e.g. depression, the OAT program may be applicable if tailored to the needs of the subgroup of patients in question. For example, the targets developed for OAT may vary between different subgroups.
Given the different subgroups mentioned above, one underlying goal in the assessment of avoidance is identifying the specific object of the fear [39]. Therefore, a typical challenge in the clinic is to identify the exact stimuli that provoke fear or distress and that should be the target for exposure [32]. Because OAT programs are not based strictly on avoidance, the clinician needs to work to “expose well” since we will need to identify what is being avoided, target it, and develop the exposure to it. While the current protocol for exposure assumes fear of movement, there nevertheless may be a host of other emotional triggers [36] or internal stimuli including the pain itself [7]. Guiding patients through exposure then can extinguish co-occurring emotional distress that interfere with increasing activities [32].
A couple of examples are offered as illustrations. First, it might be expected that patients seeking care and suffering disabling pain might also suffer strong negative affect such as shame and depression [27]. Passionate emotions may generate unhelpful avoidance behaviors that function to avoid this negative affect in the short term [8]. For example, rather than only avoiding movements, these patients may avoid a variety of personally relevant, emotional stimuli [36] which in turn impacts negatively on their activity level. To avoid the shame of questions (“When are you going back to work”), for example, a patient may avoid social activities. Exposure then might need to include such emotional stimuli that are barriers to activity training [8]. A single-subject study employing a hybrid exposure, i.e., en exposure training program that combines usual exposure techniques for fear of movement with exposure for distressing emotions that block activities has shown promise [32]. Second, consider patients who “endure” pain in the pursuit of being able to continue performing various activities [16]. According to the endurance model, these patients may use suppression or distraction to avoid feeling the pain and thus inadvertently exacerbate the physical injury. This fits well into the idea of “pacing” that Fordyce describes in Chapter 10 where it is used to reduce excessive or all-or-none activity patterns. Since suppression and distraction are used to avoid feeling sad and useless due to poor performance, exposure might focus on stimuli that provoke these feelings to thereby optimize the “pacing” program and bring activity levels into a normal level.
It is unlikely therefore, that activity training for patients suffering chronic pain will be “successful” unless the treatment includes a specific focus on “exposing well” i.e., by keenly observing avoidance, identifying the stimuli associated with it and developing exposure to treat it. For some subgroups, exposure will be the central key to successful activity enhancement.
EARLY APPLICATIONS TO PREVENT CHRONICITY
One of the most important aspects of the Fordyce behavioral approach may be in stimulating the application of OAT in the context of early intervention designed to prevent the development of pain-related disability. Such interventions are relevant potentially to people with a wide variety of pain problems. Briefly, since the theory behind OAT described the development of disability over time, it also suggests that methods that disrupt or counteract the learning mechanisms involved may prevent chronicity. Specifically, rather than allowing rest and alternative behaviors to become ingrained, maintaining or resuming normal activities as the injury heals could be helpful in preventing the development of persistent disability. Moreover, the OAT program offers an excellent method for assisting patients in resuming activities directly after an injury. By systematically increasing activity levels towards pre-injury levels, the patient regains confidence, strength and mobility. If the activity provokes pain, this can be evaluated and if necessary the rate of increasing the quota can be adjusted The idea has been so potent that virtually every guideline for dealing with back pain in primary care settings recommends advice to remain active (and OAT as a method) or to resume activities should they nevertheless be problematic [21].
“Exposing well” also can be a key to successful early preventive intervention, e.g., in primary care, for the subgroup of patients who already suffer excessive worry and fear about their injury. Typically, patients who develop persistent problems suffer a series of recurrent episodes in which each re-injury potentially may enhance the associated fear and catastrophizing. Indeed there is clear evidence that some patients applying for care demonstrate high levels of pain-related fear, fear-avoidance beliefs, and catastrophic worry already when seeking care at the primary care level [5,13,17,41,55]. When these psychological factors are present, basic techniques such as providing advice to remain active are not effective. As Fordyce asserted, simple instructions are a weak method for changing behavior. In fact, we found that very early on, a subgroup of patients who reported higher scores on variables like fear and distress were at an increased risk for future disability [5]. Compared to those without an elevated risk (the majority) where virtual no one developed long term work disability during the follow up, 35% of those with elevated fear scores and 62% of those with both elevated fear and distress scores did develop long-term disability. Consider another investigation of patients seeking care for the first time for an episode of back pain in primary care where the subgroup with comparatively high scores on measures of fear, catastrophic worry and distress also were found to have the poorest long-term outcomes [56]. In other words, for this subgroup, typical treatments e.g., advice to be active, reassurance, sick leave, and analgesics were not effective. Instead, these patients appear to benefit from exposure techniques that address their idiosyncratic fears and worries. Therefore, the OAT program might be considered at the time of first consultation and applying OAT with a specific focus on exposure may be particularly appropriate for the subgroup with higher levels of fear and avoidance.
Let us look at the empirical evidence on early interventions in primary care. Even though the precise role of OAT programs has not yet been identified, there is mounting evidence that early interventions that specifically address psychological factors and include activity training can be successful. A comprehensive review found somewhat mixed results for early interventions, but concluded that successful programs included two vital aspects [40]. First, they specifically assessed psychological risk factors such as fear and beliefs to isolate patients likely to develop persistent disability. Second, the interventions specifically targeted the psychological risk factors. Indeed, most of the studies include advice to remain active or offered a training program, similar to OAT, oriented toward resuming usual activities. However, the data suggest that mere advice, while helpful, is less effective than an actual OAT program. For instance, one early study showed that providing advice and instruction on resuming activities as compared to treatment as usual resulted in a significantly more patients returning to work with 68% vs 56% returning to work within a given time [14]. Others have found similar results [19,44]. Thus, encouraging patients to “behave well” as Jensen describes, is helpful. However, the results of trials where advice to remain active was a main ingredient can be compared with those where OAT has been systematically utilized. In one such study OAT under the supervision of trained personnel was combined with a problem-solving technique aimed at increasing participants ability to cope with problems in a flexible way where 85% returned to work suggesting that the systematic use of OAT may be central [52]. Exposing well may be the key for the subgroup of patients with risk factors e.g. fear and catastrophic worry [8]. Some early intervention packages include OAT that correspondingly feature exposure techniques for those patients in this subgroup [28,30]. There is reason to believe that “exposing well” is an integral part of a successful OAT program provided early on for patients in the subgroup with elevated levels of fear, fear-avoidance beliefs and catastrophic worry. Still, there is an urgent need to examine these ideas empirically in order to develop further early intervention programs that systematically include exposure techniques.
CONCLUSIONS
The OAT program described by Fordyce provides a systematic approach to resuming usual activities for patients suffering pain. This commentary has cast it in the light of research since the program’s inception in 1976 and suggests that “exposing well” is a key to success particularly for certain subgroups of patients. The co-occurrence of pain and various behavioral and emotional problems is common and makes each patient’s needs unique. This offers an opportunity to tailor the OAT intervention to the individual. A key part of this tailoring is determining what movements, activities, or situations may be a source of fear, worry, or other emotions being avoided so that they can be used for “exposing well”. Some subgroups may even require exposure to other stimuli e.g. emotional cues [27]. In a word, exposing well may be a key for successful application of the OAT program with patients suffering pain.
For early intervention it seems essential that the subgroups of patients with risk factors e.g. catastrophic worry, fear of movement, and distress be identified early and provided with a systematic OAT program that incorporates exposure. This is a difficult task that seems to require careful application and additional research is in order to develop the best method [2,4,18]. However, early intervention is imperative because even if the number of patients in this subgroup is relatively small, such patients are very likely to develop disability. Therefore, including a judiciously executed OAT early intervention program specifically including exposure techniques designed to reduce fear and worry should be employed.
Careful and considered application of the principles involved in the OAT program is necessary to ensure high standards and excellent success rates. However, the wide application of the program in different clinics, settings, patients and practitioners, carries the danger of substantial variation in implementation. Training of clinicians in the use of OAT is necessary in order to impart understanding of the underlying principles as well as to deal with the day to day issues that arise in the clinic Patients need to be thoroughly assessed, not only in terms of physical capacity, but also in terms of their psychological condition. Avoidance behaviors need to be identified and selected for a hierarchy of exposure. Exposing well also means developing a program for systematically assisting the patient in overcoming their fears and worries via exposure techniques. This systematic approach should enable enhanced clinical outcomes, a noble result for both the patient and the clinician.
Finally, I would like to call for a new program of research concerning OAT in view of the revitalized interest hopefully brought about by this book. Although the OAT program is a cornerstone of treatment firmly established in 1976, we know appallingly little about it. In fact, only a small number of studies have even systematically evaluated its effects in rehabilitation or as an early intervention. Further, even fewer investigations have attempted to study its components (e.g. how reinforcement is delivered, what activities are selected, how goals are determined, etc) or improve on the treatment components. It would appear that OAT might be tailored to meet better the needs of subgroups of patients. In addition to selection and targeting, there needs to be further research also into practical implementation and how the program is actually delivered. There should also be research into the effects of exposure on avoidance behavior just as there is a need for research on reinforcement of reactivation as emphasized by Fordyce. Since research highlighted above suggests that exposure to the avoidance behaviors may be crucial, there is in fact a need for a new research initiative to clarify many aspects of OAT, but in this endeavor in would appear that research specifically into exposure focused on avoidance behavior should be given a particularly high priority.
REFERENCES
1. Bailey KM, Carleton RN, Vlaeyen JWS, Asmundson GJG. Treatments addressing pain-related fear and anxiety in patients with chronic musculoskeletal pain: a preliminary review. Cognitive Behaviour Therapy 2010;39: 46–63.
2. Bergbom S, Boersma K, Linton SJ. When matching fails: Understanding the process of matching pain-disability treatment to risk profile. Submitted.
3. Bergbom S, Boersma K, Overmeer T, Linton SJ. Relationship among pain catastrophizing, depressed mood, and outcomes across physical therapy treatments. Physical Therapy 2011;91:754–64.
4. Bergbom S, Flink IK, Boersma K, Linton SJ. Early Psychologically Informed Interventions for Workers at Risk for Pain-Related Disability: Does Matching Treatment to Profile Improve Outcome? Journal of Occupational Rehabilitation 2014;24:446–457.
5. Boersma K, Linton S. Screening to identify patients at risk: profiles of psychological risk factors for early intervention. The Clinical Journal of Pain 2005;2:38–43.
6. Crook J, Milner R, Schultz IZ, Stringer B. Determinants of occupational disability following a low back injury: A critical review of the literature. J Occup Rehab 2002;12:277–95.
7. De Peuter S, Van Diest I, Vansteenwegen D, Van den Bergh O, Vlaeyen J. Understanding fear of pain in chronic pain: Interoceptive fear conditioning as a novel approach. Eur J Pain 2011;15:889–94.
8. Flink I, Boersma K, Linton SJ. Pain Catastrophizing as repetitive negative thinking: Development of the conceptualization. Cogn Behav Ther2013;42:215–23.
9. Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: A meta-analytic review. Pain 1992;49:221–30.
10. Fordyce WE. Behavioral methods for chronic pain and illness. St. Louis, Mo.: Mosby, 1976.
11. Fordyce WE, Brockway JA, Bergman JA, Spengler D. Acute back pain: A control-group comparison of behavioral vs traditional managment methods. J Behav Med 1986;9:127–140.
12. Gatzounis R, Schrooten MGS, Crombez G, Vlaeyen JWS. Operant learning theory in pain and chronic pain rehabilitation. Curr Pain Headache Rep 2012;16:117–26.
13. Grimmer-Somers K, Prior M, Robertson J. Yellow flag scores in a compensable New Zealand cohort suffering acute low back pain. J Pain Res 2008;1:15–25.
14. Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain? Spine 2000;25:1973–6.
15. Hasenbring M, Verbunt J. Fear-avoidance and endurance-related responses to pain: new models of behaviour and their consequences for clinical practice. Clin J Pain 2010;26:747–53.
16. Hasenbring MI, Hallner D, Rusu AC. Fear-avoidance and endurance-related responses to pain: Development and validation of the Avoidance-Endurance Questionnaire (AEQ). Eur J Pain 2009;13:620–8.
17. Hill JC, Dunn KM, Lewis M, Mullis R, Main CJ, Foster N, Hay EM. A primary care back pain screening tool: Identifying patient subgroups for initial treatment. Arth Rheum 2008;59:632–41.
18. Hill JC, Whitehurst DGT, Lewis M, Bryan S, Dunn KM, Foster NE, Konstantinou K, Main CJ, Mason E, Somerville S, Sowden S, Vohora K, Hay EM. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet 2011;378:1560 – 71.
19. Hlobil H, Uegaki K, Staal JG, de Bruyne MC, Smid T, Van Mechelen W. Substantial sick-leave costs savings due to a graded activity intervention for workers with non-specific sub-acute low back pain Eur Spine J 2007;16:919–24.
20. Keefe FJ, Dunsmore J, Burnett R. Behavioral and cognitive-behavioral approaches to chronic pain: Recent advances and future directions. J Consult Clin Psychol 1992;54:776–83.
21. Koes BW, van Tulder M, Lin CWC, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010:1–20.
22. Leeuw M, Goossens M, Van Breukelen G, De Jong J, Heuts PH, Smeets R. Exposure in vivo versus operant graded activity in chronic low back pain patients: Results of a randomized controlled trial. Pain 2008;138:192–207.
23. Leeuw M, Goossens MEJB, Linton SJ, Crombez G, Boersma K, Vlaeyen JWS. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med2007;30:77–94.
24. Linton SJ. A critical review of behavioural treatments for chronic pain other than headache. Brit J Clin Psychol 1982;21:321–37.
25. Linton SJ. A critical look at pain management programs: Current status and emerging directions. J Pain Soc 1993;11:9–16.
26. Linton SJ. A review of psychological risk factors in back and neck pain. Spine 2000;25:1148–56.
27. Linton SJ. A transdiagnostic approach to pain and emotion. J App Biobehav Res 2013;18:82–103.
28. Linton SJ, Andersson T. Can chronic disability be prevented? A randomized trial of a cognitive-behavior intervention and two forms of information for patients with spinal pain. Spine 2000;25:2825–31.
29. Linton SJ, Bergbom S. Understanding the link between depression and pain. Scand J Pain 2011;2:47–54.
30. Linton SJ, Boersma K, Janson M, Svärd L, Botvalde M. The effects of cognitive-behavioral and physical therapy preventive interventions on pain-related sick leave: A randomized controlled trial. Clin J Pain 2005;21:109–19.
31. Linton SJ, Boersma K, Jansson M, Overmeer T, Lindblom K, Vlaeyen JWS. A randomized controlled trial of exposure in vivo for patients with spinal pain reporting fear of work-related activities. Eur J Pain 2008;12:722–30.
32. Linton SJ, Fruzzetti A. A hybrid emotion-focused exposure treatment for chronic pain: A feasibility study. Scand J Pain 2014;5:151–158.
33. Linton SJ, Hellsing AL, Bergström G. Exercise for workers with musculoskeletal pain: Does enhancing compliance decrease pain? J Occup Rehab 1996;6:177–90.
34. Linton SJ, Jannert M, Overmeer T. Whose goals should guide? A comparison of two forms of goal formulation on operant activity training. J Occ Rehab 1999;9:97–105.
35. Lohnberg JA. A review of outcome studies on cognitive-behavioral therapy for reducing fear-avoidance beliefs among Individuals with chronic pain. J Clin Psychol Med Settings 2007;14:113–22.
36. Lumley MA, Cohen JL, Stout RL, Neely LC, Sander LM, Burger AJ. An emotional exposure-based treatment of traumatic stress for people with chronic pain: Preliminary results for fibromyalgia syndrome. Psychotherapy: Theory, Research, Practice, Training 2008;45:165–172.
37. Mallen C, Peat G, Thomas E, Dunn KM, Croft PR. Prognostic factors for musculosketal pain in primary care: a systematic review. Brit J Gen Pract 2007;57:655–61.
38. Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomised controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain 1999;80:1–13.
39. Morley SJ, Eccleston C. The object of fear in pain. In: GJ Asmundson, JWS Vlaeyen, G Crombez, editors. Understanding and treating fear of pain. Oxford: Oxford University Press, 2004. p. 163–188.
40. Nicholas MK, Linton SJ, Watson PJ, Main CJ. Early identification and management of psychosocial risk factors (“Yellow Flags”) in patients with low back pain: A reappraisal.. Phys Ther 2011;91:737–53.
41. Pearce G, McGarity A, Nicholas MK, Linton SJ, Peat JK. Better outcomes in worker’s compensation through very early selective intervention. Australasian Faculty of Occupational & Environmental Medicine and Australasian Faculty of Rehabilitation Medicine, Combined Annual Scientific Meeting. Adelaide, 2008.
42. Shaw WS, Linton SJ, Pransky G. Reducing sickness absence from work due to low back pain: How well do intervention strategies match modifiable risk factors? J Occ Rehab 2006;16:591–605.
43. Shaw WS, Pransky G, Fitzgerald TE. Early prognosis for low back disability: Intervention strategies for health care providers. Disab Rehab 2001;23:815–28.
44. Staal JB, Hlobil H, Köke AJA, Twisk JWR, Smid T, Van Mechelen W. Graded activity for workers with low back pain: Who benefits most and how does it work?. Arth Rheum 2008 59:642–49.
45. Sullivan M, Linton S, Shaw WS. Risk-factor-targeted psychological interventions for pain-related disability. In: H Flor, E Kalso, JO Dostrovsky, editors. Proceedings of the 11th World Congress on Pain. Seattle WA: IASP Press, 2006. p. 823–833.
46. Sullivan MJL, Adams H, Thibault P, Corbiére M, Stanish WD. Initial depression severity and the trajectory of recovery following cognitive-behavioral intervention for work disability. J Occup Rehab 2006;16:63–74.
47. Sullivan MJL, Adams H, Tripp D, Stanish WD. Stage of chronicity and treatment response in patients with musculoskeletal injuries and concurrent syptoms of depression. Pain 2008;135:151–9.
48. Sullivan MJL, Feuerstein M, Gatchel RJ, Linton SJ, Pransky G. Integrating psychosocial and behavioral interventions to achieve optimal rehabiliation outcomes. J Occ Rehab 2005;15:475–89.
49. Truchon M, Fillion L. Biopsychosical determinants of chronic disability and low-back pain: A review. J Occup Rehab 2000;10:117–42.
50. Turk DC. Efficacy of multidisciplinary pain centers in the treatment of chronic pain. In: MJM Cohen, JN Campbell, editors. Pain treatment centers at a crossroads: A practical and conceptual reappraisal, Vol. 7. Seattle: IASP Press, 1996. p. 257–273.
51. Turk DC. Clinical effectiveness and cost-effectiveness of treatments for patients with chronic pain. Clin J Pain 2002;18:355–65.
52. Van den Hout JHC, Vlaeyen JWS. Problem-solving therapy and behavioral graded activity in the prevention of chronic pain disability. In: Linton, SJ editor. New avenues for the prevention of chronic musculoskeletal pain and disability. New York: Elsevier, 2002. p. 293–303.
53. Vlaeyen JWS, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain 2012;153:1144–7.
54. Vlaeyen JWS, Morely SJ, Linton SJ, Boersma K, de Jong J. Pain-related fear: Exposure-based treatment for chronic pain. Seattle: IASP, 2012.
55. Westman A, Linton S, Öhrvik J, Wahlén P, Leppert J. Do psychosocial factors predict disability and health at a 3-year follow-up for patients with non-acute musculoskeletal pain? A validation of the Örebro Musculoskeletal Pain Screening Questionnaire. Eur J Pain 2008;12:641–9.
56. Westman AE, Boersma K, Leppert J, Linton SJ. Fear-avoidance beliefs, catastrophizing, and distress: A longitudinal subgroup analysis on patients with musculoskeletal pain. Clin J Pain 2011;27:567–77.
57. Williams A, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database of Systematic Reviews 2012;11: 1–82.
58. Zale EL, Lange KL, Fields SA, Ditre JW. The relation between pain-related fear and disability: a meta-analysis. J Pain 2013;14:1019–30.

Full access? Get Clinical Tree