Chapter 112 Evaluation, Stabilization, and Initial Management After Multiple Trauma
Trauma is the leading cause of death and acquired disability in children and adolescents, resulting in more deaths in children than all other causes combined.1,2 Because children with severe injuries can rapidly deteriorate, resources for rapidly identifying and treating injuries are needed immediately on arrival at the receiving hospital. The initial evaluation of injured children in the emergency department (“trauma resuscitation”) has two main goals: (1) identify and immediately treat potentially life-threatening injuries, and (2) determine disposition after the trauma resuscitation based on known or suspected injuries. The trauma team must stabilize the child, determine the extent of the injury, and develop an initial treatment plan for the child’s hospitalization.
Advanced Trauma Life Support (ATLS) is a protocol developed to standardize the initial evaluation and management of injured patients and avoid omission of potentially lifesaving interventions. The ATLS training program was initiated by an orthopedic surgeon in 1978 in response to suboptimal care that he and his family received in a rural hospital after an airplane crash in a Nebraska cornfield. After 30 years of refinement, ATLS serves as the standard for initial management of injured patients and is now taught to providers around the world.2 The impact of ATLS on reducing morbidity and mortality after injury has been affirmed in several studies.3,4 ATLS training is mainly focused on treating the injured adult, but includes modules that emphasis the anatomic, physiologic, and psychological features that make management of the injured child unique.
The initial management of injured adults has been the domain of trauma surgeons; however, the jurisdiction of care for the injured child is not as well defined at many centers. Frequently, pediatricians have an active role in the initial management and treatment of injured children.5 While formal ATLS training is not needed for most pediatric providers, this training should be mandatory for those actively involved in the initial evaluation of injured children. At the least, a working knowledge of the evaluation and management steps of ATLS is needed for pediatricians and pediatric specialists who encounter injured patients in an acute care setting. The goal of this chapter is to provide a focused introduction to the initial resuscitation of injured children. This chapter does not serve as a replacement for ATLS training but will instead highlight aspects of the resuscitation that are unique to injured children or may not be emphasized in the ATLS curriculum.
Prehospital Care and Trauma Team Activation
One approach that has been used in many centers to address the problem of overtriage is the use of a tiered team response in the emergency department.6 Based on prehospital criteria, patients who are identified as being most at risk for severe injury are met by a full team upon arrival, including a trauma surgeon, emergency department physicians, critical care physicians, anesthesiologists, nurses, and radiology technicians. Patients with a lower likelihood of severe injury are initially met by a smaller team with the option of summoning a larger team if the initial evaluation suggests a severe injury. Centers that have used this approach for team activation have significantly reduced the expenditure of resources on minimally injured patients without any impact on the care received for more severely injured patients.7
Trauma Resuscitation
Designating a specific room and team for trauma resuscitations helps ensure needed resources are immediately available. A single location ensures that supplies (e.g., emergency airway kits, chest tube and thoracotomy trays, and central or intraosseous vascular access kits) are available and that team members know to gather at a specific site. Physicians, nurses, radiography technicians, respiratory therapists, and other hospital personnel needed for trauma resuscitation are identified in advance as trauma team members and assemble and assume their roles in the resuscitation area upon arrival of the injured child (Figure 112-1). These seemingly simple preparations ensure that the arriving patient has the maximal resources available at the receiving hospital.
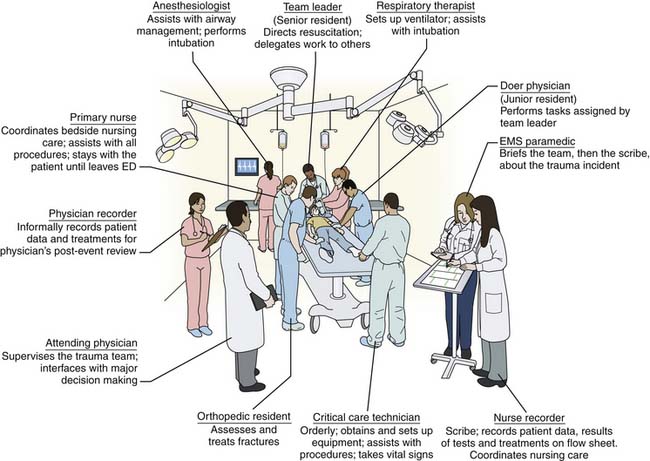
Figure 112–1 The trauma room and team.
(From Sacrevic A, et al: Quantifying adaptation parameters for information support of trauma teams. CHI 2008 Proceedings.)
Before arrival to the hospital, prehospital providers transmit information to hospital providers about the mechanism of injury, the status of the patient, and initial treatments given. This information can alert the team to prepare specific equipment or resources or to summon other essential personnel. Before the patient arrives, it is good practice for the team to review prehospital information to ensure all team members are aware of the patient’s status and anticipated needs. A “time out” or quiet period facilitates this information transfer. Upon arrival to the emergency department, an additional and final exchange of information between the prehospital providers and the trauma team occurs. Essential elements that should be obtained in this report include details about the injury event, vital signs obtained at the scene and during transport, pertinent physical findings, and the initial treatments administered and response to these treatments.8 Allowing the prehospital providers to give their report before starting the patient evaluation or even transferring the patient to the emergency department gurney improves information exchange and prevents repetitive questions later in the resuscitation. Obtaining a record of the prehospital event completes the formal information exchange between prehospital and in-hospital providers. These records can contain critical information for early in-hospital management but often are not immediately obtained because prehospital providers are moving on to their next assignment and the trauma team is focused on direct care of the patient.
The Primary Survey
Overview
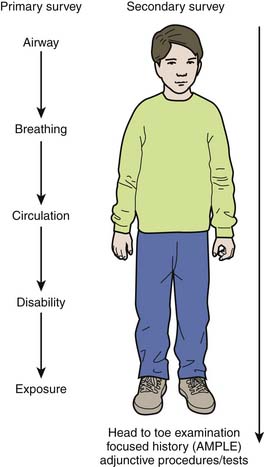
The primary survey, as defined by ATLS, is a prioritized evaluation and management protocol focused on identifying and treating the most life-threatening injuries first. This approach is different from the traditional initial evaluation in a patient where an extensive history and physical exam is performed before diagnosis and treatment. The steps of the primary survey are taught in the ATLS course as a sequence followed by one provider with one nurse assistant. In actual practice, most centers have a team of providers rather than only two, allowing the evaluation and management steps to proceed forward even if one step leads to a delay. For example, a relatively more time-consuming step such as placing an intravenous catheter can be performed by one team member while others move on to subsequent steps in the primary survey. The typical model used at many trauma centers is to have a single provider on the team perform and report the components of the primary survey, supported by other team members as it is conducted. A designated team leader stands at the foot of the bed, receives information reported by the team and provides higher level direction of the conduct of the resuscitation. While the steps of the primary survey provide the framework for the initial assessment, new information may be obtained in later phases, or a patient’s status may change, requiring iterative performance of each step. It is often a challenge to ensure the team retains its focus on the underlying prioritization scheme of the primary survey and does not omit or minimize steps in this process (Figure 112-2).2 When resuscitations are evaluated, compliance with ATLS protocols is often low, mandating continued training and retraining to ensure the well-established benefits of this protocol are realized.9
Establish an Airway with Cervical Spine Stabilization (A)
Establishment of a patent airway with cervical spine stabilization is the first step of the primary survey. All patients should immediately receive oxygen as the evaluation is begun. After oxygen is placed, evaluation of the airway can proceed. Injured children who present to the emergency department can be placed into three categories with respect to initial airway management: (1) those with a patent airway requiring no manipulation, (2) those who have undergone intervention in the field or at another hospital to establish a patent airway, and (3) those who will need an intervention to establish a patent airway. Most children evaluated by the trauma team are in the first group. For these patients, evaluation should include several simple steps including asking the patient’s name, inspection for craniofacial injuries, assessment for voice changes, and listening for obvious stridor. These steps can be performed easily and rapidly in most children. A simple statement that “the airway is patent” will communicate to the team these confirmatory steps have been accomplished. Because most injured children will not require any specific airway management, omission of elements of the airway assessment are common in pediatric trauma resuscitation. In a study of pediatric trauma resuscitations analyzed by video review, the most common omission in airway evaluation was not providing supplemental oxygen (omitted in 67% of resuscitations). Fewer than one quarter of resuscitations included a complete assessment of the airway along with assessment of ‘breathing,’ the second component of the primary survey.10 Although the patency of the airway may seem “obvious” in many patients, subtle and early signs of pending airway compromise will be missed if a formal airway evaluation is not completed (Table 112-1).
Table 112–1 Missed Components of the Primary and Secondary Survey in Pediatric Trauma Resuscitation: Management Errors Among All Patients (N = 90)
| Errors Identified | N (%) |
|---|---|
| AIRWAY AND BREATHING | |
| Delay in oxygen therapy | 60 (67) |
| Chest not auscultated | 40 (44) |
| Oxygen saturation not measured | 33 (37) |
| Neck not adequately examined | 71 (79) |
| CERVICAL SPINE | |
| No head stabilization on transfer | 18 (20) |
| CIRCULATION | |
| Inappropriate intravenous access | 18 (20) |
| Pulse not assessed | 37 (41) |
| Central capillary refill not assessed | 59 (66) |
| Blood pressure not measured | 28 (31) |
| Fluid bolus not warmed | 33 (89) |
| DISABILITY | |
| Pupils | 22 (25) |
| Posture | 22 (25) |
| SECONDARY SURVEY | |
| Perineum not examined | 41 (45) |
| Head not examined | 13 (15) |
| Ears not examined | 16 (18) |
| Mouth not examined | 41 (45) |
| Back not examined | 13 (15) |
| Chest not examined | 3 (3) |
| Abdomen not examined | 2 (2) |
Modified from Oakley E, Stocker S, Staubli G, et al: Using video recording to identify management errors in pediatric trauma resuscitation, Pediatrics 117:658-664, 2006.
The second category is children with an airway already established in the field or other hospital, usually by endotracheal intubation. Airway interventions performed prior to a patient’s arrival should not be interpreted as an adequate airway and additional steps should be performed to assess airway patency, especially in light of the relative tenuous nature of pediatric airways placed under emergency situations.11 The key steps to evaluating an endotracheal tube placed outside the emergency department are assessing the appropriateness of tube size, evaluating tube depth, assessing adequacy of ventilation by auscultation and inspection of the chest, measurement of end tidal CO2, and confirmation of tube position with a chest radiograph. The appropriate tube size can be evaluated using age-specific formulas and charts or by comparing the tube with the child’s fifth (little) finger. Deep placement of an endotracheal tube in a prehospital setting is common especially among younger children. Most prehospital providers have more experience with intubating adults, leading to a tendency toward deeper tube placement. In addition, the shorter airway of children increases the likelihood that an endotracheal tube will migrate from the proper position during transport. An easy rule for rapidly assessing tube depth is that the length of the tube at the teeth should be three times the tube size. Age-specific formulas for evaluating endotracheal tube depth are available and are more easily used by providers with greater experience in management of airways. Assessment that the endotracheal tube is an adequate airway should include steps that are more formally part of the breathing (B) phase of the primary survey, including assessment of ventilation by auscultation and inspection and measurement of end tidal CO2. Because of a shorter airway and relatively less margin for movement of an endotracheal tube in younger child, correct endotracheal tube position cannot be reliably confirmed by auscultation of bilateral breath sounds alone.12 Final confirmation of endotracheal tube position requires obtaining a chest radiograph. In most cases, the chest radiograph should be deferred until later in the resuscitation because simpler and more rapid evaluations can be performed to verify tube position that do not interrupt the conduct of the primary survey. However, a chest radiograph should be performed in the emergency department before transport to other areas of the hospital to avoid the need for airway management in less optimal hospital settings.
The final category of injured children undergoing airway evaluation is those who present with airway compromise requiring intervention. Because this category of injured children is least common, clearly defined personnel and procedures are needed to prepare the team to efficiently and safely establish an airway. Indications for endotracheal intubation in pediatric trauma include apnea, inability to maintain a patent airway by other means, need to protect the lower airway from aspiration of blood or vomitus, impending or potential compromise of the airway, presence of a closed head injury (Glasgow Coma Scale [GCS] score ≤8), and inability to maintain adequate oxygenation with face-mask oxygen supplementation.2 An altered level of consciousness, usually due to an intracranial injury, is the most commonly observed reason for emergency airway intervention in the acutely injured child. Although a neurologic assessment is performed later in the primary survey, early recognition of children requiring a formal airway because of an altered level of consciousness is essential. The AVPU scale (awake, responds to verbal stimuli, responds to painful stimuli, and unresponsive) is one model for assessing consciousness that has been found to correlate with the GCS scale and which may be useful for identifying children who are at risk for a compromised airway because of an altered level of consciousness.13 Patients with an AVPU score of “P” or “U” can be anticipated to have a GCS score of 8 or 3, respectively, and should receive early airway intervention.14
When a more definitive airway is needed, the preferred method for establishing an airway in pediatric trauma is orotracheal intubation. A rapid-sequence technique is preferred for most injured children, because intubation is made easier by eliminating protective airway reflexes and safer by preventing aspiration and decreasing physiological stress that can lead to increased intracranial pressure in children with severe head injuries.15 During intubation, steps should be taken to account for the short length and narrow diameter of the trachea and the narrowing of the trachea at the cricoid ring, including choosing an appropriately sized tube and confirming tube position. While it can be a good option in other settings, nasotracheal intubation is usually not performed for injured children because this technique is more difficult due to the acute angle of the posterior pharynx of the child. Nasotracheal intubation has not been recommended in patients with facial trauma, cerebrospinal fluid leaks, or suggestions of basilar skull fractures, because these injuries suggest the possibility of a disruption between the cranial vault and nasopharynx.16,17 Laryngeal mask airway (LMA) is also an option for emergency airway management in situations in which endotracheal intubation cannot be accomplished.17–19 However, as the LMA does not protect against aspiration and cannot be used effectively to provide positive pressure ventilation in patients with altered respiratory compliance or resistance, it should be used only as a rescue technique if the patient cannot be intubated.20
Fewer than 1% of all adult patients who require an emergency airway in the emergency department require a surgical airway.21 The percentage of children requiring an emergency airway after injury is likely to be even smaller. Among injured children with a comprised airway, endotracheal intubation may not be possible because of significant craniofacial injuries, massive bleeding from the nasopharynx or oropharynx, or preexisting anatomical features such as a short neck, micrognathia, or small mouth that make intubation more difficult. In this “cannot intubate/cannot ventilate” subset, a systematic approach is needed to rapidly secure a patent airway (Figure 112-3).20
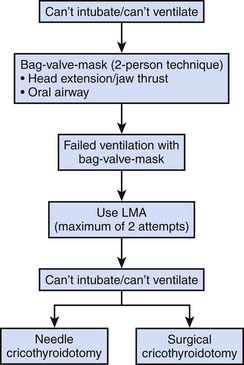
Figure 112–3 Flow chart for “can’t intubate/can’t ventilate” airway emergencies.
(Modified from Henderson JJ, Popat MT, Latto IP, et al: Difficult Airway Society guidelines for management of the unanticipated difficult intubation, Anaesthesia 59:675-694, 2004.)
If bag-mask ventilation is successful, the team has time to find alternative routes of securing an airway. Examples include attempting fiberoptic intubation or bringing a more experienced physician to the trauma bay to assist with establishing an airway. If bag-mask ventilation is not successful, an appropriate invasive procedure may be required. Among injured children, appropriate options include surgical or needle cricothyrotomy, depending on the child’s size. Among children with a larger airway whose cricothyroid membrane is easily palpated, a surgical cricothyrotomy is preferred.2 If small neck size or other anatomic features preclude the safe placement of a cricothyrotomy, a needle cricothyrotomy with needle jet insufflation of oxygen into the airway is the recommended approach. Surgical cricothyrotomy should be performed by members of the team with experience with this technique. This procedure has four main steps: (1) identification of the cricothyroid membrane, (2) making an incision through the skin and cricothyroid membrane, (3) stabilization of the larynx with a tracheal hook at the inferior aspect of the ostomy, and (4) placement of a tube in the trachea.22 Training in this technique is now included as part of the ATLS course.
Although controversy surrounds whether needle cricothyrotomy should be used at all in pediatric patients, it is still advocated by some authorities as a rescue technique in specific clinical scenarios. Needle cricothyrotomy can be performed using commercially available kits. When one is not available, the procedure can be carried out by inserting a large bore (12 to 18 gauge) angiocatheter in a caudal direction at a 30- to 45-degree angle through the cricothyroid membrane. During needle advancement, constant negative pressure is applied to the plunger of the syringe to aspirate air and confirm its endotracheal position.23 After confirmation of endotracheal placement, the syringe and stylet are removed and the cannula is connected to an oxygen source. Among larger children and adolescents, the cannula should be connected to an unregulated oxygen supply of 50 psi, because ventilation cannot be adequately provided using an ambu bag.24 While pediatric evidence is limited, a flow of 25 to 35 psi from a standard regulator set at 10 to 12 L/min for most children has been recommended. Another approach that can be used is based on flow rates and estimated tidal volumes (TV): 10 to 25 psi with TV of 340 to 625 mL for children 8 years and older; 5 to 10 psi with TV of 240 to 340 mL for children 5 to 8 years old; and 5 psi with TV of 100 mL for patients who are 5 years and younger.23 Standard intravenous tubing can be connected to the cannula and a Y connector placed between the intravenous tubing and the oxygen tubing. Intermittent occlusion for 1 second and release of the Y-connector for 4 to 5 seconds provides some passive ventilation. A needle cricothyrotomy is a highly tenuous airway and should be carefully secured after placement and converted to a more stable airway as soon as possible. This approach is only sufficient for 30 to 45 minutes because of the progressive respiratory acidosis that results from underventilation.2 Because surgical airway management is rarely performed in pediatric patients, centers that manage injured children should have the equipment and adequately trained personnel for performing these procedures when needed.
Cervical spine stabilization should be viewed as part of the “A” step and is included as part of airway management in ATLS. In contrast to intubation in other hospital settings such as the intensive care unit, intubation in the trauma bay should proceed with the assumption that a cervical spine injury is present until this type of injury has been formally ruled out. This step is needed in patients with any mechanism of injury that can be associated with cervical spine trauma. Many injured children present to the emergency department with a cervical collar that was placed in the field because of the mechanism of injury. The initial evaluation of the airway should be immediately followed or simultaneously performed with an assessment of the proper size and fitting of the cervical collar or placement of a cervical collar when one is not present. When endotracheal intubation is required, in-line cervical spine stabilization should be used. A member of the team holds the neck on each side with his or her hands and forearms maintaining the stability of the spine during airway manipulation. Despite the importance of this step, neck inspection and palpation while maintaining C-spine precautions and head stabilization during transfer to the trauma gurney are steps omitted in 80% and 20% of trauma resuscitation performed for injured children, respectively.10

Full access? Get Clinical Tree