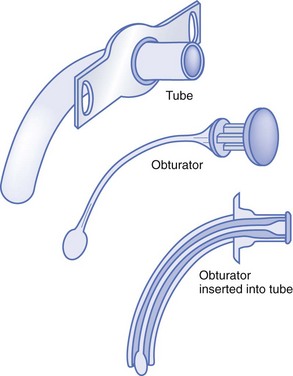
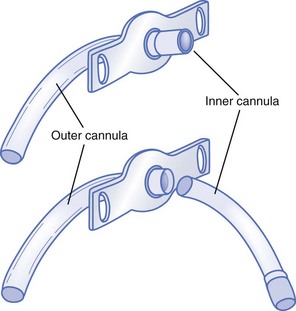
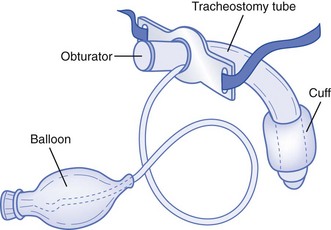
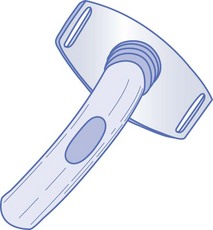
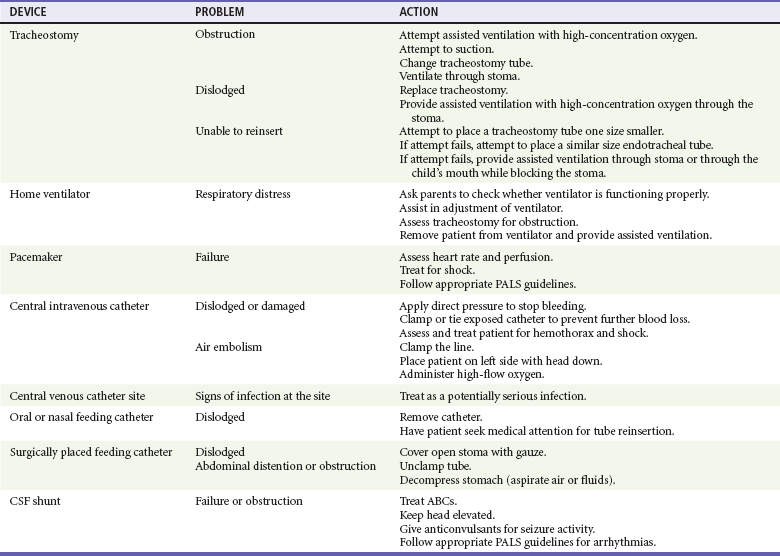
Chapter 187 Children with special health care needs are those who have or are at increased risk for a chronic physical, developmental, behavioral, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally.1 The prevalence and characteristics of the CSHCN community depend on the definition used. With use of the federal definition derived by the Maternal and Child Health Bureau of 1998, a study analyzing data from 2006 to 2008 found that approximately one in six children in the United States experienced a special health care need.2 There is a higher prevalence among older children, boys, and non-Hispanic white and black children, and after adjustment for demographic factors, families in poverty are more likely to have CSHCN. Advances in medical science and technology have been instrumental in allowing children with complex medical problems to survive beyond the neonatal period. Moreover, family-centered care has been the goal for the care of these children, and as a result, many are living at home instead of in institutions.3 CSHCN are frequent users of the emergency medical system. Emergency medical services are typically activated during the time of a crisis. This crisis may occur because of equipment failure or panic by the caregiver who is fatigued or new to caring for the child with special needs. However, a survey of 100 families with CSHCN conducted at a tertiary care urban pediatric center demonstrated that although 97% of the families had sought emergency care in the past, only 23% of the caregivers had ever called 911 before, and 93% had driven their child to the hospital during an emergency.4 Families may transport their children either to the nearest community hospital or to their “home” institution, which is likely to be a tertiary care center. Most emergency medical service jurisdictions transport to the nearest “appropriate” medical facility. Children (and youth) with special health care needs are usually cared for by adults who have been trained to manage their child’s daily care. In general, families are knowledgeable about their child’s medical conditions and technologic needs. Families may have detailed medical plans that specify such things as the size of tubes, how often to change tubes, dosages of medications, and ventilator settings. One example of a program that provides information to medical care providers is the Emergency Preparedness for Children with Special Health Care Needs program of the American Academy of Pediatrics and the American College of Emergency Physicians.5 This emergency notification program’s purpose is to communicate specific information to medical caregivers about the conditions and medications of a child or adolescent with special needs. An emergency information form is completed by the child’s primary care physician or family and is carried with the child. Although most caregivers are adept at handling many of their children’s emergencies, caregivers seek help for a variety of reasons, including the need for respite, equipment malfunction, an overwhelming medical problem, or help with transport to the child’s home hospital. In contrast to the pediatric population, there is no universally recognized definition for adults with special health care needs. The Institute of Medicine (IOM) has used several different definitions for disability, including an “inability or limitation in performing socially defined activity and roles expected of individuals within a social and physical environment.”6 The number of adults who meet this broad definition is difficult to calculate. Current estimates indicate that as many as 50 million U.S. residents have some type of disability.7 Estimates come from various national surveys that vary in their definitions, questions, and target populations. Even more importantly, of 18 different national surveys reviewed by the IOM Committee on Disability in America, only four include institutionalized individuals.7 Given the large number of surveillance groups, the IOM has recommended adoption of the World Health Organization’s International Classification of Functioning, Disability and Health, which is currently being used in many countries as a standardized assessment tool for both individuals and populations. General Issues for Children and Youth with Special Health Care Needs CSHCN differ from other children in a variety of ways. Some CSHCN may be neurologically impaired and therefore have intellectual disabilities. Their physical growth may be limited, resulting in stature smaller than that of other children of the same age. As a result, medical personnel cannot rely on age- and weight-based norms and should either ask caregivers for this information or use length-based tapes to estimate weight, to calculate drug dosages, and to determine fluid management. Children and adolescents with chronic health conditions may have vital signs that differ from those expected for children without chronic conditions of the same age.4 For example, baseline vital signs are altered in children with cardiac conditions or who are on mechanical ventilators. A child with an unrepaired complex congenital heart defect may have a baseline pulse oximetry reading in the low 80s. Some children with lung diseases may have respiratory rates higher than expected, yet these higher respiratory rates are considered their baseline.4 Also, some children may have sensorineural deficits, such as blindness and deafness, that may make history taking and physical assessment challenging. Medical care providers need to be cognizant of these differences. Airway and Pulmonary Conditions There are three causes of tracheomalacia: congenital or intrinsic tracheal anomaly (occurring within the trachea), which may be associated with a tracheoesophageal fistula (a patent connection between the trachea and esophagus); extrinsic defects (occurring outside the trachea), such as abnormal development of the vasculature around the trachea that may create a ring, which places pressure on the trachea and interferes with airflow; and acquired malacia, which occurs in children with prolonged intubation or chronic tracheal infections.8 Bronchopulmonary dysplasia (BPD), a chronic lung disease occurring in infants, is characterized by poor lung compliance and chronic exacerbations. BPD is a worldwide problem, with 5000 to 10,000 new cases reported each year. BPD, cystic fibrosis, and asthma are the three most common chronic lung diseases in infants.9 BPD develops primarily in low-birth-weight infants who have respiratory distress syndrome. Babies born before 32 weeks’ gestation may not have enough surfactant to keep their alveoli open.10 However, BPD development is not limited to survivors of respiratory distress syndrome. BPD may result from alveolar damage caused by other lung diseases, exposure to prolonged high oxygen concentrations, use of mechanical ventilation after birth because of conditions such as neonatal pulmonary hypertension and pneumonia or other infections, or trauma to the lungs.10 Apnea in infants and young children is defined as a cessation in breathing for more than 20 seconds or associated with a change in color, limpness, altered mental status, or bradycardia. Apnea occurs more frequently in infants born prematurely and generally reflects immature neurologic and respiratory control mechanisms.11 These pauses in respiration may be due to central apnea, which is the result of an absence of a neurologic signal to the respiratory muscles. Underlying causes include encephalitis, brainstem infarction or tumor, neuromuscular disorders such as muscular dystrophy, and thoracic restrictive disorders such as kyphoscoliosis. These children are discharged home from the hospital on an apnea monitor. Apnea monitor alarms often result in ED visits. The apnea monitor should be transported with the child to the hospital. Most monitors contain a computer chip that records information that can be downloaded into a computer at the child’s regular hospital (home hospital) to determine the origin of the monitor alarms (high or low heart rate, apnea, or artifact). Apnea in adults is most frequently related to obstructive sleep apnea. This can be due to altered oropharyngeal anatomy but is most commonly secondary to obesity. Decreased muscle tone during sleep leads to obstruction of the pharynx and hypopharynx with redundant tissue. Central sleep apnea is also seen in patients with heart failure. Regardless of etiology, sleep apnea can result in mild to severe sleep disturbances leading to daytime somnolence and irritability. It is also associated with significant morbidity and mortality, including heart failure, acute coronary syndrome, cerebrovascular accidents, and death.12–15 Like pediatric obstructive apnea, obstructive sleep apnea in adults is treated with noninvasive positive-pressure ventilation, such as CPAP, during sleep. Myasthenia gravis is a neuromuscular disorder that can cause respiratory insufficiency and failure. Myasthenia gravis is an autoimmune process that attacks the postsynaptic acetylcholine receptors at the neuromuscular junction. It most commonly affects the bulbar muscles but can also result in generalized weakness.16 Other neuromuscular disorders that can affect the respiratory muscles include muscular dystrophy, multiple sclerosis, and amyotrophic lateral sclerosis. In any patient with respiratory muscle weakness secondary to a neuromuscular disease, pulmonary function tests are an important component of the assessment. One test that can rapidly be obtained in the ED is a negative inspiratory force or maximal inspiratory pressure. A value of less than 20 cm H2O is the generally accepted cutoff for severe impairment and can help determine which patients need ventilatory support. This test is usually performed by a respiratory therapist with use of a pressure gauge connected to a disposable mouthpiece. Tracheostomy tubes are placed to facilitate mechanical ventilation, to provide a bypass of the upper airway, or to keep the airways clear of secretions. The more common conditions for which tracheostomy tubes are placed include tracheal stenosis, tracheomalacia, certain craniofacial anomalies, BPD, muscular dystrophy, spinal cord injury or disease, traumatic or anoxic brain injury, and cerebrovascular accidents.8 Because the tubes are available from several manufacturers, their sizing and markings vary. Common brands are Shiley, Bivona, Hollinger, Portex, and Bardeen. Typically, the sizes are marked on the packaging and on the flange, or wings, of each tube. They range in size from 00 for newborns to 7.0 for older adolescents and adults. The inner and outer diameter ranges are provided so that comparisons between brands can be made. They range from 2.5 mm for infants to 10.0 mm for adolescents and adults. This information is helpful for emergency personnel in replacing a tracheostomy tube or in choosing an endotracheal tube for oral intubation or use through a stoma. The inner diameter of a tracheostomy tube should be used to choose the endotracheal tube size for insertion through a stoma. Tracheostomy tubes also come in various lengths. Neonatal tubes are shorter than pediatric tubes, although the inner diameters may be the same.8 There are several types of tracheostomy tubes and attachments: single-cannula tubes (Fig. 187-1), double-cannula tubes (Fig. 187-2), cuffed tubes (Fig. 187-3), and fenestrated tubes (Fig. 187-4).8 Neonates, infants, and young children use single-cannula tracheostomy tubes. A double-cannula tube can be used in older children and adults. It contains an outer tube that stays in the stoma and an inner tube that is removable for cleaning and pulmonary toilet. Tracheostomy tubes for older children and adults have an inflatable cuff to keep the tube in place and to prevent air leaks. Fenestrated tubes have a hole in the cephalic portion of the tube that redirects air into the upper airway to allow the individual to speak and to breathe through the nose and mouth. This is facilitated by a decannulation plug that is attached to the opening of the tube. Figure 187-1 Single-cannula tracheostomy tube. (Modified from Susan Gilbert in Teaching Resource for Instructors in Prehospital Pediatrics [TRIPP]; www.cpem.org.) Figure 187-2 Double-cannula tracheostomy tube. (Modified from Susan Gilbert in Teaching Resource for Instructors in Prehospital Pediatrics [TRIPP]; www.cpem.org.) Figure 187-3 Cuffed tracheostomy tube. (Modified from Susan Gilbert in Teaching Resource for Instructors in Prehospital Pediatrics [TRIPP]; www.cpem.org.) Figure 187-4 Fenestrated tracheostomy tube. (Modified from Susan Gilbert in Teaching Resource for Instructors in Prehospital Pediatrics [TRIPP]; www.cpem.org.) For sudden onset of respiratory distress, suctioning of the tracheostomy tube may be helpful. Approximately 2 to 3 mL of normal saline should be instilled before suctioning. If suctioning two or three times does not relieve the obstruction or respiratory distress, the medical provider should change the tracheostomy tube because there may be a thick mucous plug obstructing airflow through the tube. An endotracheal tube can be used as a substitute if the appropriate size of a tracheostomy tube is not available. For patients cared for at home, the parents or caregivers often have spare equipment in their “go” bags that can be used (for troubleshooting, see Tables 187-1 and 187-2). Table 187-1 Medical Devices: Common Problems and Solutions Modified from Adirim T, Smith E: Special Children’s Outreach and Prehospital Education. Sudbury, Mass, Jones and Bartlett, 2006.
Evaluation of the Developmentally or Physically Disabled Patient
Perspective
Distinguishing Principles of Disease
Specific Disorders
Tracheomalacia
Bronchopulmonary Dysplasia
Apnea
Chronic Respiratory Failure in Adults
Tracheostomy Tubes

Full access? Get Clinical Tree


Evaluation of the Developmentally or Physically Disabled Patient
Only gold members can continue reading. Log In or Register to continue




