Fig. 21.1
Members of the New York Society of Anesthesiologists’ Committee on Fellowships. (Courtesy of the New York State Society of Anesthesiologists, New York, NY.)
Francis McMechan established the International Anesthesia Research Society (IARS) in 1922, and the International College of Anesthetists (ICA’which awarded the first certificate in anesthesiology in 1935), but circumstances militated against his efforts to establish a US based certification.
ICA certification required:
1.
Documentation of graduation from medical school and type of anesthesia practice
2.
Documentation of the candidate’s practice for the previous 3 years, meetings attended, and papers published
3.
Submission of 10 complete records including preoperative evaluation, with a discourse on that which was learned from each case.
McMechan, crippled with rheumatoid arthritis, would not tolerate dissent and rarely sought compromise. His adamant opposition to anesthesia practiced by nurses, placed him in direct opposition to surgeons and the American Medical Association (AMA) who favored non-physician anesthesia, demonstrating their allegiance to the nurses providing anesthesia in support of their surgeries. McMechan, an internationalist, married to a French woman, favored international over a more limited US certification. The AMA, the NYSA, and the ABMS established in 1933 by the AMA, opposed such an approach. McMechan’s internationalism came at a time of increasing isolationist views in America. Having suffered over a million casualties, beginning with the Revolutionary War and continuing through the Great War (World War I), American society had turned inward, giving a deaf-ear to McMechan’s proposals. His uncompromising persona precluded reconciliation.
Paralleling McMechan, the Committee on Fellowships of the NYSA, with Buchanan as Chair and Paul Wood, (an Obstetrical Anesthesiologist at the 5th Avenue Hospital in New York City who famously created the Library-Museum bearing his name) as secretary, began developing its own certification process, a process that eventually established the ABA. The Committee formally incorporated in 1935 “under and by virtue of the laws of the State of New York, (and) the name…shall be the Examining Board, Committee of Fellowship, American Society of Anesthetistsor American Board of Anesthesiology.” Initial Committee members were Buchanan, Wood, and William Branhower, E Leslie Burwell, Archer Bush, Simon Ehrlich, Bernard Eliasberg, Robert Hammond, and George Tong.
On 23 July 1935, approximately 1 year after McMechan’s ICA awarded its first certificates, the Committee met for the first time. In 1936, Fellowships were granted to 88 members of the NYSA, “certifying on record only”. The Committee’s intent for establishing specific certification for anesthesiologists was that “the basic science for anesthesiology must, of course, stress pharmacology and physiology which, apparently, are less important to the operating surgeon”.
In 1927, at the University of Wisconsin, Ralph Waters created the first academic Department of Anesthesiology. His protégés subsequently developed parallel anesthesia programs that enlarged the recognition of anesthesiology as a physician-led, independent specialty and thereby prompted the formation of a certification processes. One protégé, Emery Rovenstine, established the Department of Anesthesia at the Bellevue Hospital at New York University College of Medicine, in 1935. Rovenstine, Buchanan, Wood and Waters would join the first Board of Trustees of the new Examining Board.
Restriction of the certification by the Fellowship Committee of the NYSA to locally trained practitioners precluded support by the nationally-based AMA. In 1935, the NYSA extended membership outside New York, accepting anesthetists from 17 other states. Further to the national focus of the AMA, on December 10, 1936, the NYSA incorporated in New York as the American Society of Anesthetists (ASA). Reflecting McMechan’s concerns regarding non-physician practitioners, the ASA by-laws stated that the purpose of the Committee on Fellowships was “to protect the public against irresponsible and unqualified practitioners who profess to be specialists in anesthesiology.”
The ABMS rebuffed early ASA attempts to establish a primary certification process. The ABMS and the AMA considered anesthetists as “surgeons specializing in anesthesia”. This hostile climate led the Committee on Fellowships to seek other options, leading to a discourse with the American Board of Surgery (ABS) which was organized on 1 January 1937. On 10 January 1937, Waters and Wood presented the ASA position to the ABS. The ABS instructed the ASA to form an “examining board in anesthesiology” as a sub-board of the ABS. A formal affiliation was established on 2 June 1937. The initial examining board consisted of 3 members nominated by the ASA, 3 by the ABS and 3 by the Section of Surgery of the AMA. A 10th member would be a representative from the ABS. The initial articles of incorporation specified that the Examining Board would establish criteria of fitness to practice anesthesia, and arrange, control and conduct examinations to determine the qualifications, and grant certificates to those who voluntarily apply and meet these required standards.
The initial Board of Trustees, as it was called, included the then giants of anesthesia (Fig. 21.2): Buchanan (NYC), Arthur Guedel (Los Angeles), John Lundy (Rochester, Minnesota), Rovenstine (NYC), Henry Ruth (Philadelphia), Ralph Tovell (Hartford, Connecticut), Waters (Madison, Wisconsin), Wood (NYC), and Philip Woodbridge (Boston). The surgical representative from the ABS was Arthur Elting from Albany, New York. Buchanan was designated Chair with Ruth as Vice-Chair and Wood as Secretary-Treasurer.
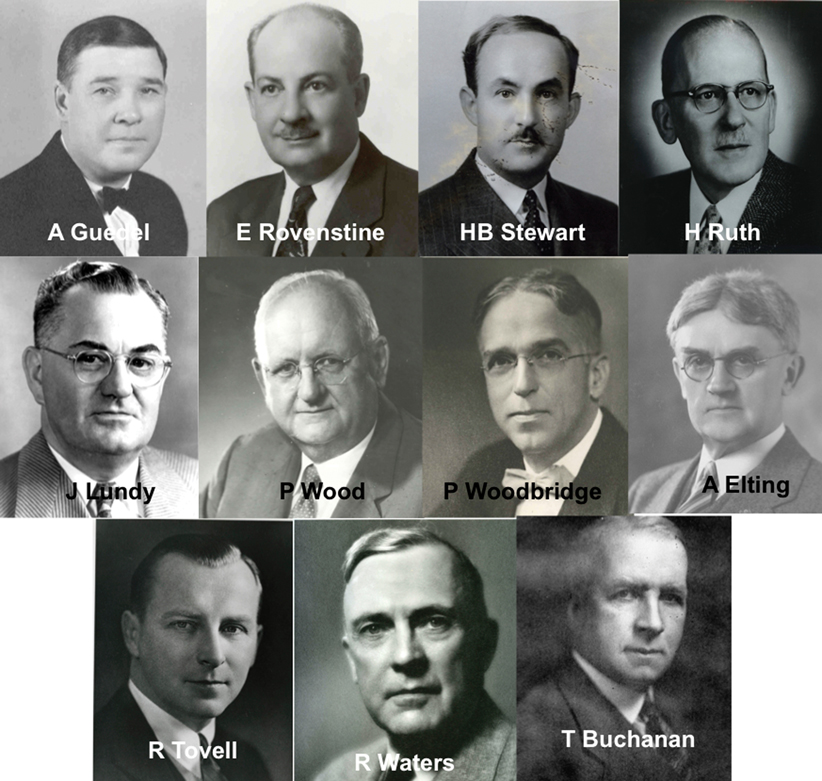
Fig. 21.2
The initial Board of Trustees of the American Board of Anesthesiology. (Courtesy of the American Board of Anesthesiology, Inc., Raleigh, NC.)
The Examining Board established criteria for entering the examination process:
1.
Medical school graduation
2.
Completion of internship
3.
2 years of training, including 18 months of practical training in anesthesia
4.
2 years in the sole practice of anesthesia
5.
Membership in the AMA or a comparable approved national medical society (a change from the original criteria that required NYSA membership)
The Board developed categories for the first candidates for certification:
I.
Founders: Professors and Associate Professors previously elected to Fellowship in the ASA were to be certified without examination
II.
Group A: Those having practiced for 15 or more years were to appear before the Board and could be certified without examination
III.
Group B: Those practicing for 7.5 years or more or having administered anesthesia in at least 1500 major procedures could be certified following only an oral examination
IV.
Group C: Those who met the 5 “criteria for entering the examination process” listed above and submitted 150 of their cases for evaluation were allowed to enter the full examination system
Finally, certification required a positive vote of two-thirds of the Board of Trustees of the Examining Board and approval by the ABS.
Arthur Guedel did not fall under any of the group designations, and he was removed as a Trustee and replaced by H. Boyd Stewart of Tulsa, Oklahoma. In 1943, recognizing Guedel’s enormous contributions to anesthesiology, the Board of Directors of the ABA approved his certification without examination. Guedel said, “thank you”.
The AMA initially resisted certification of the Founder’s group of 40 anesthetists and suggested placing this group in Group A. The ABS rejected this proposal as it would have eliminated 95% of the candidates including Rovenstine, Wood, and Tovell. On 1 January 1939, the ABA awarded certificates to the Founders and 6 candidates from Group A (Fig. 21.3).
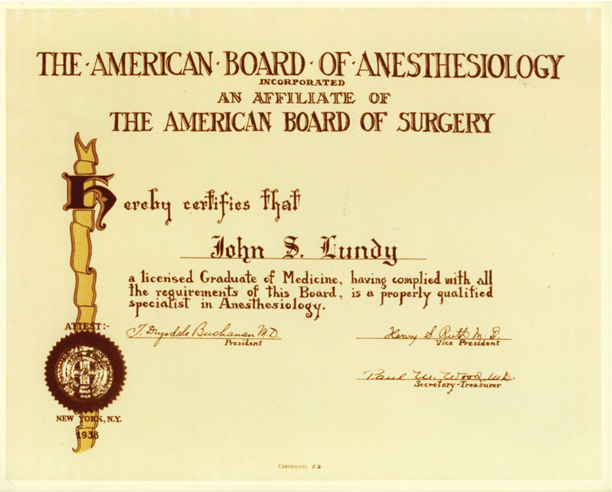
Fig. 21.3
The second certificate given by the American Board of Anesthesiology. (Courtesy of the American Board of Anesthesiology, Inc., Raleigh, NC.)
The ASA Trustees next sought independent recognition by the ABMS, and thus the medical establishment, for anesthesiology. In February 1938, the ABMS approved the ABA as a sub-board of the ABS, and on 23 March 1938, this new Board was incorporated in the State of New York. The final articles of incorporation began the separation from the ABS, as desired by the ASA Trustees, by replacing the 3 nominations previously assigned to the ABS with 3 nominations from the American Society of Regional Anesthesia (ASRA). The role of the ASRA in the nominating process ended with its merger with the ASA in 1939. These articles also identified the former Trustees as Directors.
An early issue faced by the new sub-board of the ABS was the status of nurse anesthetists and “non-professional” practitioners. (This could be almost anyone, including a first-year medical student such as Eger, who with his first anesthetic nearly killed a patient [1].) The National Association of Nurse Anesthetists (NANA’later the American Association of Nurse Anesthetists or AANA) asked the ABS to protect the position of nurse anesthetists. The ABS requested a meeting between the NANA, the ABS and the ABA to examine the feasibility of having the ABA sanction a training curriculum and certification for nurse anesthetists. They met on 27 November 1938. The minutes of this meeting indicated that the NANA wanted to “compile a pattern curriculum which we expect to have taught in the various schools of anesthesia for nurse anesthetists. After this has been introduced we expect to have examinations for the students with eventual certification.”
Discussions revealed mutual distrust and ABA apprehension concerning independent nurse anesthesia practice. Elting, the ABS representative to the ABA, attempted to encourage discussion, stating that “Just as the American Board of Surgery is perhaps in the relative position of the god-father of the American Board of Anesthesiology, so the American Board of Anesthesiology might perhaps be the god-father to the Association of Nurse Anesthetists or the nurse anesthetists of this country.” The ABA continued the dialogue to avoid offending the ABS, but expressed little enthusiasm for involvement with nurse anesthesia. At an ABA meeting in May, 1939, Buchanan related a conversation with an ABS surgeon who cautioned, “To be frank with you I want to state that Dr. Graham, Dr. Elting and I are very concerned about the way you are handling this nurse anesthetist question … Frankly we feel that you are side-stepping it.” At this May meeting, Buchanan reported that he had told Elting and Rodman that he “would not consent to the American Board of Anesthesiology being sponsors to any nurse anesthetists and they both agreed with me that I was right.”
Thus the two protagonists’anesthesiologists and nurse anesthetists’missed an opportunity. Trained anesthetists’nurse and physician’were scarce, and the approaching World War indicated a great increase in the need for trained anesthetists. A formal teaching arrangement might have been established that would have benefited the nurse-physician relationship and the quality of care given to our patients. Anesthesiologists’especially those involved in certification’might have taken the opportunity to participate in nurse certification. The nurses asked for guidance and physicians rejected their overtures to the detriment of their relationship.
An October 1939 report to the ABA by John Lundy exemplifies the physician perception of nurse anesthetists: “The Committee has functioned perfectly. There have been many opportunities offered to the girls to come to us for advice on what would be the best books to read and the advice hasn’t been sought.” Several ABA discussions considered withdrawing or not certifying physicians who were involved in training nurse anesthetists. Furthermore, when in 1950, the ABA added membership in “good standing” in the ASA, as a criteria for candidacy for certification, the board stated that “If a man signs a nurse’s training certificate he is not in good standing in the ASA”. However, we cannot find that the ABA acted against any physician working with or training nurse anesthetists. In a statement in 1976, the ABA demonstrated an attempt at accommodation with nurse anesthesia, in proposing to become involved in and accept responsibility “for examination and certification of non-physician anesthesia personnel.” Subsequently, the ABA refrained from involvement with nurse anesthetist certification, leaving such matters to the ASA as the representative of the practicing anesthesiologist. Anesthesiologists do contribute to nurse anesthetist education, participating importantly in training, but without the sanction of the ASA or the ABA.
The ABA relationship with its “god-father”, the ABS, was sometimes contentious. In October, 1939, Lundy reported on a conversation with the ABS’s Elting. Elting stated that “The first thing I want to tell you is that the American Board of Anesthesiology is not an independent Board. They cannot issue a certificate without our consent and while we haven’t bourn [sic] down on them previously, we may have to.” The ABA remained sensitive to their position as an affiliate of the ABS, and attempted to limit concerns raised by the ABS as evidenced by a Lundy statement at the October 1939 ABA meeting: “I too hope that this Board will keep those problems under their consideration and that they won’t do the thing that will offend that Board [ABS] and make them think that we are unsympathetic as to the problem they have to face.”
In March 1940, the ABMS with the support of the ABS, recommended ABA independence to the AMA. On 16 February 1941, the ABMS approved the ABA as a primary board with equal standing to others, including the ABS. Neither Buchanan nor McMechan lived to see this event. McMechan died on 26 June 1939, with some speculating that the AMA’s decision to establish the Section on Anesthesiology in June 1940 was not just coincidental. Buchanan died suddenly on 22 March 1940 and was replaced as President by Ruth, and as Director by Charles McCuskey, from Glendale, California. In recognition of his contributions in establishing certification for anesthesiologists culminating in the acknowledgement of anesthesiology as a primary specialty, the ABA directors paid tribute to Buchanan.
The by-laws of the ABA as a primary ABMS Board listed the following objectives:
1.
To elevate the standard of anesthesiology
2.
To familiarize the public with its aims and ideals
3.
To protect the public from irresponsible and unqualified practitioners
4.
To examine and certify
Organization of the ABA and its Directors
Achievement of a balanced national representation motivated selection of future directors. The merger of the ASRA and the ASA in 1939, eliminated the short-lived role of the ASRA in the nomination process. The seal (logo) of the ABA, designed in 1941 and still in use today, reflects this relationship of the ABA with the ASRA along with the AMA, ASA and ABS (Fig. 21.4). In 1942, the AMA provided four nominees (Lundy, McCuskey, Ruth, and Tovell), the ASA provided four (Rovenstine, Waters, Wood, and Woodbridge) and the Southern Medical Society provided one (Stewart). In 1944, the New England Society of Anesthesiology nominated a tenth (Meyer Saklad). Over the following decade, the ABA asserted increasing control over the selection process, assuming sole responsibility for the final selection of nominees, while expressing its desire for input from the nominating bodies. Notwithstanding that expression of desire, conflicts arose between the ABA and the nominating bodies. With Stewart’s resignation in 1946, the Southern Medical Society nominated John Winter. Winter completed Stewart’s term in 1949, by which time nominations by component societies (Southern and New England) had been assigned to the ASA. The ASA refused to re-nominate Winter, and instead nominated Harvey Slocum who was selected. When, in 1950, the ASA also refused to re-nominate Ruth and Lundy, expressing concern over their “heavy-handedness” and length of service, the ABA “in defiance of their wishes” re-elected the two and made it clear that if the ABA so desired, the AMA and ASA were compelled to nominate a specified candidate, thereby insuring the re-election of existing Directors and control by the ABA of its own makeup.
Fig. 21.4
The ABA seal (logo). (Courtesy of the American Board of Anesthesiology, Inc., Raleigh, NC.)
Differences between AMA and ABA continued into the 1950s. In 1955, the AMA refused to re-nominate Edward Touhy, appointed in 1951 to fill Ruth’s unexpired term. The last founding Director, Lundy, retired in 1955 after 18 years of service. Albert Faulconer and Forrest Leffingwell replaced Ruth and Lundy.
The controversy over control of the nominating process was resolved when the ABA, AMA and ASA created a joint nominating committee, with 2 representatives from each organization. The ABA president served as the non-voting chair of the committee. The ABA gained the control it desired when it was agreed that each ASA and AMA representative would have 1 vote and each ABA representative would have 2 votes. The ABA could not be out-voted. Established in 1961, this Triple Committee would nominate 3 candidates for each position, and the ABA would elect its Directors from this slate. As the work of the ABA increased, the number of Directors increased from 10 to 11 in 1950, and to its current number of 12 in 1973. Director’s terms as a member of the Board were initially 6 years without term limits. In 1950, this changed to a maximum of two 6-year terms, and in 1957 to three 4-year terms, requiring re-nomination and re-election at each interval. Gender was also considered as a factor in discussions related to Director nominations in 1938, when Huberta Livingstone was considered “… as the probable female member of the Board when it was organized….”, but the first female Director, Judith Donegan, was not elected until 1983. Gender equality continued to evolve slowly so that as of October 2012, there are three female directors.

Full access? Get Clinical Tree







