Endocrine System
Addison’s Disease
(see also Aldosterone in Part 5, p. 249)
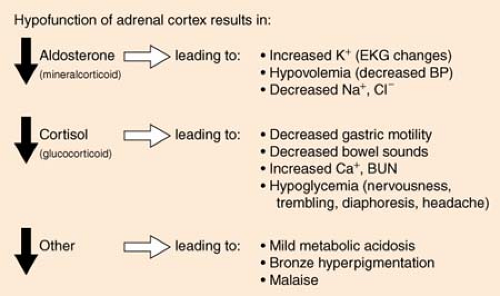
Addison’S disease results from hypofunction of the adrenal cortex of the kidney, causing a severe decrease in levels of aldosterone and cortisol with resultant fluid and electrolyte imbalances; protein, fat, and carbohydrate disturbances; and ultimately circulatory collapse. Although abrupt withdrawal of steroids is a common cause, approximately 70% of cases are idiopathic. Addison’S disease is the “opposite” of Cushing’S disease, in which there is an oversecretion of glucocorticoid hormones.
The pituitary gland secretes adrenocorticotropic hormone (ACTH), which stimulates the adrenal cortex to secrete its own hormones. Addison’S disease is diagnosed by stimulating ACTH with drug therapy and evaluating the response of the adrenal cortex. Normally, the excretion of hydroxycorticoids and ketosteroids increases, whereas patients with Addison’S disease show little or no increase. Also, eosinophils in the patient’S blood are measured. A drop of 60% to 90% in the count after ACTH is given is normal, but there is little drop in the count in a patient with Addison’S disease.
Addisonian crisis is a life-threatening exacerbation of the disease with severe hypotension, shock, coma, and vasomotor collapse.
Treatment is based on fluid replacement with 5% dextrose in normal saline and the IV administration of corticosteroids.
Remember:
No patient with Addison’S disease should ever receive insulin. The patient may die of the resultant hypoglycemia.
Adrenal Insufficiency
(see Addison’S Disease, p. 263; Cushing’S Disease, p. 264)
Cushing’s Disease
Cushing’S disease results from oversecretion of ACTH by a pituitary or adrenal basophilic tumor, although many times it is caused by steroids, which are given for a variety of conditions, ranging from asthma to lupus, rheumatoid arthritis, other inflammatory conditions, or immune suppression following a transplant.
It is diagnosed by the presence of high-glucocorticoid metabolites in urine and plasma, indicating that adrenal hyperactivity exists. It is the “opposite” of Addison’S disease, in which there is a severe decrease in the levels of aldosterone and cortisol.
Signs and Symptoms
Persistent hyperglycemia
Protein tissue wasting (weakness, osteoporosis)
K+ depletion (dysrhythmias, renal disorders)
Na+ and H2O retention (edema, hypertension, congestive heart failure)
Abnormal fat distribution (moon face; buffalo hump; striae on breasts, axilla, legs)
Increased susceptibility to infection
Mood swings
The disease is treated by surgical removal of the causative tumor. Drugs are only palliative for inoperative cancer.
Diabetes Insipidus
(see also Syndrome of Inappropriate Antidiuretic Hormone, p. 273; Cerebral Salt Wasting in Part 1, p. 14)
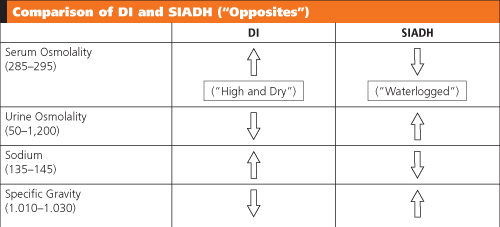
Diabetes insipidus (DI) is caused by a deficiency of the antidiuretic hormone (ADH), causing water not to be reabsorbed by the kidney tubules and resulting in excretion of large amounts of dilute urine. The disorder may appear slowly or may develop suddenly, related to injury or infectious disease.
The causes of DI fall into two categories:
Vasopressin deficiency: The pituitary gland itself is defective because of idiopathic causes such as pituitary tumors, infectious processes, vascular accidents, or neurosurgery.
Nephrogenic: Because of an inherited defect, the kidney tubules are unable to absorb water.
Signs and Symptoms
No matter what the cause, patients routinely have the following signs and symptoms:
Polydipsia and polyuria (may drink 5–40 L per day and excrete the same 5–40 L per day). Unless the patient drinks almost continuously, there is always a danger of dehydration and hypovolemic shock.
Decreased urine osmolality
Decreased urine specific gravity (<1.005)
Increased serum osmolality
Increased serum Na+
 |
Treatment
DI is treated with replacement ADH. Desmopressin acetate (DDAVP) is a synthetic ADH and is given IV on an emergent basis or as a nasal spray for long-term therapy.
Aqueous vasopressin (Pitressin), given IV or subcutaneously, is sometimes used for transient or severe DI. It is short acting and may cause angina or hypertension. Dehydration and electrolyte imbalances must also be attended to, and replacement IV therapy with hypotonic solutions (0.5 normal saline) is administered, often to match the urine output on an hour-to-hour basis.
Diabetes Mellitus
(see also Insulin in Part 8, Drugs, p. 318)
There are basically two types of diabetes mellitus: Type 1 and Type 2. They vary in their causes and their treatment.
Type 1 Diabetes Mellitus
Type 1 diabetes is thought to develop because of an autoimmune response causing the β cells within the islet tissue of the pancreas to be destroyed. Because insulin is not available, the blood glucose level rises above what is safe for the body. REMEMBER: Insulin is the “key” that unlocks the cells, allowing the glucose to enter. No insulin = no key = glucose is “locked out” of cells and remains in blood = high blood glucose levels. Over time, these high glucose levels damage blood vessels and nerves throughout the body and increase the risk of eye, heart, blood vessel, nerve, and kidney disease. Patients with Type 1 diabetes are dependent on insulin to survive. For this reason, Type 1 diabetes was once known as insulin-dependent diabetes mellitus (IDDM) and was also once known as juvenile-onset diabetes, because it usually develops during childhood or the teen years. Symptoms include increased urination, increased thirst, increased appetite, and weight loss.
Type 2 Diabetes Mellitus
Type 2 diabetes is the most common, occurring in about 90% to 95% of all patients with diabetes. It occurs when the pancreas still makes insulin, but not enough to meet the body’S needs. In some cases, enough insulin is made, but the body is unable to use it. Type 2 diabetes is often affected by obesity and can sometimes be controlled by maintenance of proper body weight, proper diet, and exercise. It was once known as non–insulin-dependent diabetes
mellitus (NIDDM). Whereas Type 2 diabetes does not always require medication, it is not the milder form of the disease: It can cause the same harmful effects as Type 1 diabetes.
mellitus (NIDDM). Whereas Type 2 diabetes does not always require medication, it is not the milder form of the disease: It can cause the same harmful effects as Type 1 diabetes.
Because the high glucose levels develop gradually in Type 2 diabetes, there are often no symptoms early in the disease, or the specific symptoms for diabetes (listed above) are easily overlooked.
Optimum serum glucose levels before meals should be below 100 mg/dL. The glycosylated hemoglobin (HgAlc) test tells how well blood glucose levels have been controlled over the previous 2 to 3 months. For most people, a good HgAlc level is 6% to 7%.
Pre-Diabetes
Defined by a blood glucose higher than normal, but not high enough to be diagnosed as diabetes mellitus, pre-diabetes has been proven to put people at an increased risk for progression to Type 2 diabetes (usually within 10 years). There are no symptoms, although the person is frequently overweight or obese. The cornerstone of therapy is diet and exercise, with a goal of reducing total body weight by 5% to 10%. Diagnosis is confirmed in one of two ways:
Fasting glucose test: No food is eaten overnight, and a blood glucose level is checked in the morning before eating.
Normal = <100 mg/dL; Pre-diabetic = 100 to 125 mg/dL; Diabetic = >126 mg/dL
Oral glucose tolerance test: No food is eaten overnight, after which a glucose-rich drink is consumed. Two hours later a blood glucose test is taken.
Normal = <140 mg/dL; Pre-diabetic = 140 to 199 mg/dL; Diabetic = >200 mg/dL
Although several drugs have been shown to reduce diabetes risk to varying degrees, none has been approved by the FDA. The American Diabetes Association recommends that metformin is the only drug that should be considered for use in diabetes prevention, and then only in cases of very high-risk individuals, with a body mass index of at least 35, and those who are younger than 60 years.
Diabetic Ketoacidosis
(see also Hyperglycemic Hyperosmolar Nonketotic Coma, p. 270)
Diabetic ketoacidosis (DKA) is a life-threatening medical emergency, seen most often in patients with Type 1 diabetes mellitus (insulin dependent). It occurs when there is insufficient insulin to metabolize glucose, resulting in a cascade of events leading to hyperglycemia, ketosis, and acidosis.

Full access? Get Clinical Tree