Immediate Management of Potentially Harmful Disorders
The complaint of ear pain is more common among children than adults and usually relates to an infectious process. Though some conditions are serious, patients with most ear pain conditions can receive treatment and be discharged by the emergency physician without consultation (Table 32–1).
| Diagnosis | Diagnostic Clues | Treatment | Comments |
|---|---|---|---|
| Acute mastoiditis | Fever or chills, pain, swelling, and erythema at mastoid process; typically an extension of acute otitis media; normal canal and findings of concurrent otitis media | ENT consultation, admission, IV antibiotics, possible necessity for surgical intervention; Cefotaxime, 1 g IV q 24 h, or ceftriaxone, 1–2 g IV q 24 h | Relatively rare; usually S. pneumoniae, S pyogenes, S. aureus; if it develops after resolved otitis media: acute coalescent mastoiditis |
| Bullous myringitis | Severe ear pain, TM bullae on TM surface, with surrounding erythema; middle ear space not affected | Erythromycin (EES, adult: 400 mg q.i.d.; child: 10 mg/kg q.i.d.), doxycycline, azithromycin | Mycoplasma (or viral) |
| Chondritis, perichondritis | Pain or swelling to the external (cartilaginous) ear; recent ear trauma; warm, erythematous, tender auricle, pinna skin; evidence of recent trauma or piercing; if ear is deformed, suspect chondritis (cartilage infection) | Remove foreign bodies, irrigate wounds; warm soaks and oral cephalexin; outpatient ENT follow-up; if evidence of cartilage involvement, ENT consultation, admission, IV antibiotics | |
| Foreign body | Usually young child, witnessed insertion; foreign body in canal | Removal is typically uncomfortable; tailor method to the characteristics of the foreign body (Frazier suction, alligator forceps, curette); prep with topical anesthetic; children may require restraint or sedation | If canal trauma is present, treat as for otitis externa, outpatient follow-up |
| Infected sebaceous cyst | Pain in canal; no discharge; erythematous, cystic canal surface; pain with pinna traction | Incise and drain cysts; cephalexin or dicloxacillin; outpatient ENT follow-up | May prevent recurrence with selenium sulfide (Selsun) or ketoconazole/steroid shampoo |
| Insect in canal | Buzzing or movement sensation; insect in canal or on TM catheter; flush out when patient is calm | Immobilization will relieve the discomfort; instill mineral oil in the canal with a syringe and flexible tip | Alternatively, may remove a large insect with narrow alligator forceps through the otoscope |
| Otitis externa (swimmer’s ear) | Common in regular swimmers; ear pain, itching. Purulent discharge, erythematous canal, pain with pinna traction; canal may be occluded by wall edema; normal hearing unless canal is occluded | Place a cotton wick through an obstructed or near-obstructed canal; treat with topical steroid and antibiotic preparations: hydrocortisone-polymyxin neomycin (Cortisporin Otic), 4 drops q.i.d., or hydrocortisone-ciprofloxacin (Cipro HC Otic), 3 drops b.i.d. | Typically Pseudomonas; outpatient follow-up within 3 days; reduce recurrence risk with drying rubbing alcohol drops following water exposure; consider malignant variant in diabetic, immunocompromised, or elderly patients |
| Otitis externa (malignant) | Elderly, immunocompromised, or diabetic patient with findings of otitis externa; physical findings as above | ENT consultation, admission, IV antibiotics (imipenem-cilastatin, 500 mg IV q 6 h; ciprofloxacin, 400 mg IV q 12 h or 750 mg PO q 12 h) | Pseudomonas can cause rapidly progressing, necrotizing disease among vulnerable patients; outpatient treatment may be acceptable in early disease; CT scan if mastoid osteomyelitis is suspected |
| Serous/secretory otitis media | Preceding upper respiratory infection or otitis media; unilateral hearing loss, pain, pressure, or bubbling sound (all of variable severity); normal canal; TM not erythematous, but decreased motility and light reflex; landmarks visible; air–fluid levels behind TM | Decongestant for 14 days | Not infectious; relates to eustachian canal obstruction; obtain ENT evaluation if it does not resolve in 2 weeks; some clinicians rous (mobile fluid) from secretory (thick, nonmotile fluid) otitis, but treatment is the same |
| Suppurative otitis media | Common in children; preceding upper respiratory infection; may lead to TM rupture (severe pain followed by rapid, spontaneous relief); normal canal; TM is erythematous, dull light reflex, limited motility (most specific), landmarks not visible; compare to other side; make note of TM rupture, if present; decreased hearing on affected side | Amoxicillin (adults: 500 mg t.i.d. × 10 d; children: 15 mg/kg t.i.d. × 10 d); if child has had abscess in past month, high-dose amoxicillin (30 mg/kg t.i.d. × 10 d); if recent treatment failure, amoxicillin–clavulanate (Augmentin, 25–30 mg/kg t.i.d. × 10 d); other options, trimethoprim–sulfamethoxazole, cefuroxime, ceftriaxone IM | Typical organisms: S. pneumonia, H. influenzae (children); ruptured TM will require follow-up every 2–4 weeks to ensure healing |
Ask patients about history of trauma, surgery, or recurrent infections involving the ear. Also ask about specific symptoms (eg, recent fever, upper respiratory infection, or canal discharge) and pain quality (eg, pain, pressure, itching, or “buzzing” sounds). Have the patient identify the exact location of the pain. A narrow differential diagnosis can be explored based on these historical characteristics.
Visually inspect the external ear, external canal orifice, and surrounding structures. Palpate the area surrounding the ear to identify lymph nodes or a bony prominence. Tender nodes are common in infections of the middle and external ear. Pain, swelling, and erythema at the mastoid process should prompt the clinician to consider mastoiditis. Next, view the canal and tympanic membrane. Make careful note of the appearance of the tympanic membrane regarding color, reflectivity, visibility of landmarks, and presence of fluid, air bubbles behind the membrane, or perforations. Check tympanic membrane motility by insufflation. Compare to the normal ear. If the ear examination is normal, look to the upper teeth and temporomandibular joint as possible causes.
If history and physical examination suggest mastoiditis, computed tomography (CT) scan should be obtained.
Each condition requires a specific treatment (see Table 32–1).
Sudden hearing loss is a deficit of less than 3 days duration and may be partial or complete. Diagnoses can be categorized as conductive (mechanical cause) or sensorineural (inner ear or cochlear nerve-central nervous system cause). Medication-related hearing loss is usually dose and duration related. Many potential causes must be considered (Table 32–2).
|
The patient’s account of precipitating events (trauma or recent activities) and the duration of symptom onset (seconds, hours, days) should help narrow the focus on possible causes. Unilateral deafness should increase the suspicion for a structural process (conductive or acoustic neuroma), whereas bilateral symptoms would suggest a systemic (metabolic or drug related) problem. Take a careful medication history. Severity (partial vs complete loss of hearing) also should be assessed. Finally, the presence of tinnitus, vertigo, or other neurologic symptoms should alert the clinician to the likelihood of a sensorineural cause.
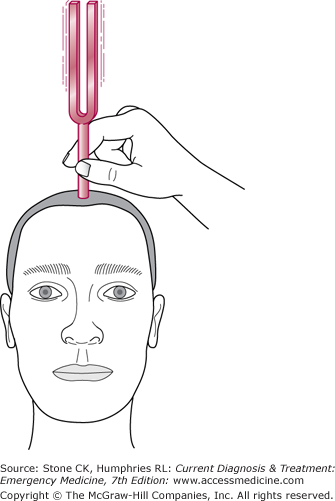
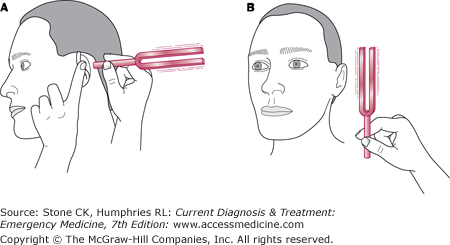
Look at the canals and tympanic membranes to rule out foreign body obstruction, infection, or injury. The cranial nerves should be examined. Weber and Rinne tests are useful for differentiating between conductive and sensorineural causes only in cases with unilateral hearing loss. The Webber test is performed by placing a vibrating 512-Hz tuning fork on the midparietal head (Figure 32–1). Sound should be heard equally on both sides. The Rinne test is performed by placing the base of a vibrating fork on the mastoid process. When the patient can no longer hear the sound, it is quickly moved off the bone and the tines placed at the ear canal (Figure 32–2). Repeat on each side. The patient should be able to hear the vibration in the air after the fork is removed from the bone. In sensorineural hearing loss, the Rinne test will be normal bilaterally and the Webber test will lateralize to the unaffected side. In conductive hearing loss, the Webber test will lateralize to the affected side and the Rinne test will also be abnormal on that side.
Bloodwork is helpful if infectious or metabolic causes are being considered. CT or magnetic resonance imaging (MRI) scan is appropriate for a suspected acoustic neuroma.
Treatment should be directed toward the underlying disorder. Rapid follow-up by the appropriate provider (ie, otolaryngologist and neurologist) is recommended.
True vertigo is a sense of motion when one is stationary. It is typically described as feeling the world spin. It can be quite disconcerting to patients, some of whom present in dramatic discomfort.
The most important determination is between central (central nervous system) and peripheral (relating to the eighth cranial nerve or the inner ear apparatus) causes. This classification usually can be resolved on the basis of history alone (Table 32–3). Symptoms that are severe, of sudden onset, and related to head movement are typically caused by a peripheral disorder. Ask about recent use of potentially vestibulotoxic drugs such as aminoglycosides, vancomycin, phenytoin, quinidine, and minocycline. Caffeine, nicotine, and alcohol are known to exacerbate symptoms. Head trauma can occasionally lead to semichronic symptoms (lasting months to years). Specific causes of peripheral vertigo are described in Table 32–4.
| Symptom or Examination Finding | Peripheral Causes | Central Causes |
|---|---|---|
| Duration of onset | Minutes to hours | Weeks to months |
| Intensity | Severe | Moderate |
| Nausea, vomiting | Typical | Often absent |
| Relation to head movement | Movement exacerbates symptoms | Often symptoms unrelated to movement |
| Patient age | Any; often young | Usually elderly |
| Nystagmus | Always horizontal or rotatory; worse with head movements and fatigues over 5–30 seconds | Presence is variable; may be vertical or horizontal with no fatigue |
| Cranial nerve or cerebellar deficits | Absent | Often present (especially ataxia–usually with slow onset; sudden onset suggests cerebellar hemorrhage) |
| Hearing | Often decreased (unilateral) or with tinnitus | Usually normal |
| Causes | Meniere’s disease | Drugs |
| Labyrinthitis (viral or bacterial) | Cerebellar mass or stroke | |
| (Benign) positional vertigo | Encephalitis or brain abscess | |
| Canal foreign body or otitis media | Vertebral basilar artery insufficiency | |
| Acoustic neuroma | Temporal lobe epilepsy | |
| Multiple sclerosis |
| Condition | Diagnosis | Comments |
|---|---|---|
| Acoustic neuroma | Gradual (days to weeks) onset, unilateral hearing loss and tinnitus; initially mimics vestibular neuronitis, but symptoms worsen over weeks as tumor progresses centrally; central signs and symptoms (decreased corneal reflex, ataxia) later in course; diagnosis by CT scan | Schwann cell tumor; recovery correlated with early surgery |
| Benign paroxysmal (positional) vertigo | Symptoms and nystagmus associated with head movement—often subsiding gradually several minutes after movement | Most common cause of peripheral vertigo; typically no specific cause |
| Ménière disease (paroxysmal labyrinthine vertigo) | Associated with unilateral hearing loss and tinnitus; vertigo with sudden onset and short (1–24 h) duration; intense, recurrent, associated with vomiting and distress; ear pressure; nystagmus during the attacks, not between or positional | Sometimes associated with high salt intake; may improve with low-sodium diet |
| Suppurative labyrinthitis | Prominent hearing loss and vertigo; temporally related to recent bacterial infection of middle or inner ear; diagnosis by CT scan | CT scan to evaluate for mastoiditis; requires inpatient treatment with intravenous antibiotics or surgery |
| Vestibular neuronitis | Symptom onset over 1–2 hours; nystagmus and discomfort associated with head movement; nohearingloss | Lasts 3–7 days, but mild symptoms may persist for weeks; thought to be related to viral labyrinthitis |
Examine the ear canal, tympanic membrane, cranial nerves, and cerebellar function. All patients with vertigo may have difficulty with the tandem walk exercise, but the presence of focal cerebellar examination findings (rapid alternating movements, heel-shin slide, or finger-to-nose pointing tests) should raise suspicion for a central cause. Identifying nystagmus, especially with head movement can help narrow the differential diagnosis. The Dix-Hallpike test can help elicit the vertigo symptoms and nystagmus if they are not present at rest. In this test, the examiner places a hand on the patient’s occiput, and the patient is rapidly reclined from an upright position onto a flat surface. The head should extend off the back edge so that the neck can be somewhat hyperextended. The test can be repeated with the head rotated to each side. A positive result occurs with acute worsening of the vertigo or production of nystagmus. Nystagmus relating to a peripheral cause typically starts in 1–3 seconds and diminishes over 5–30 seconds after head movement. Nystagmus from a central cause does not typically extinguish.
Imaging (by CT scan or MRI) is warranted for patients with a suspected central cause or elderly patients with equivocal findings. MRI provides superior resolution of the cerebellum, though CT scan will typically rule out large lesions.
Patients with prolonged nausea and poor fluid intake will often require intravenous hydration. Pharmacotherapy is more successful in peripheral-type vertigo. It is directed at relief of symptoms and does not affect the duration of the illness. The first-line agent is oral meclizine (25–50 mg every 8–12 hours), but patients unable to manage oral fluids are better off with intravenous normal saline and diazepam (5–10 mg intravenously, 2–4 mg intravenously for the elderly). In general, drugs with anticholinergic effects are useful. These include diphenhydramine (50 mg intramuscularly or orally every 6–8 hours), dimenhydrinate (50–100 mg intramuscularly or orally every 4 hours), cyclizine (50 mg orally every 6 hours), and promethazine (25 mg orally, rectally, or intravenously every 6–8 hours). Patients with peripheral vertigo can be discharged after moderate improvement of symptoms and ability to take oral liquids. Some patients may need to be admitted to hospital for severe symptoms or inability to maintain oral intake. Depending on the cause, symptoms are likely to last several hours to 1 week but may persist for 4–5 weeks. Many patients with central vertigo will require inpatient management targeted at the underlying cause, though those who are comfortable after treatment and have firm follow-up can be discharged.
A particle repositioning (Epley) maneuver may be attempted if positional vertigo is suspected. It is based on the belief that moving the canalith to the utricle area of the inner ear will prevent it from stimulating the sensory mechanism. All motions should be done slowly such that each full cycle of the maneuver takes 2 minutes. First, perform the Dix-Hallpike test. Then place the patient in a sitting position, turn the head 45° toward the affected side, lay the patient down, and allow the head to extend 45° beyond neutral while hanging off the top edge of the bed. Rotate the extended head to the midline and then 90° away from the affected side (as determined by the fast component of the nystagmus). Then flex the neck to neutral, sit the patient up, and rotate the head back to midline. The maneuver often must be repeated several times to be successful.
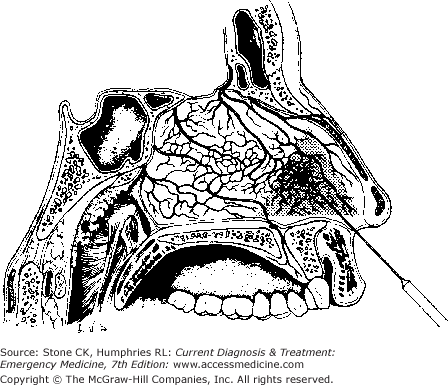
Most episodes of epistaxis do not result in significant blood loss, are not life-threatening, and can be managed with minimally invasive measures. However, the clinician should begin with an assessment of hemodynamic stability and provide support (intravenous fluids or blood products) when appropriate. The typical bleeding site is the Kiesselbach area of the anteromedial nostril, an area at risk due to the anastomoses of three separate arteries (Figure 32–3). Though predominantly due to trauma or environmental exposure, epistaxis can rarely be the first symptom of a growing nasal or sinus malignancy.
Many patients will be predisposed to bleeding, due to warfarin, platelet-inhibiting medications, renal failure, or hemophilia. Initial history should be directed toward medications as well as easy bruising or bleeding. In cold seasons, the dry conditions created by heated indoor air can dehydrate the airways, predisposing the nasal mucosa to cracking. The repeated blowing and wiping of a nose in the setting of upper respiratory infection or allergic rhinitis can abrade and injure the mucosal surface as can blunt trauma and nose picking. The possibility of pregnancy should be assessed since the incidence of epistaxis is increased and the choice of pharmacologic agents may be changed by this knowledge.
Hemodynamically stable patients are best examined sitting upright. In this position, most blood will exit the anterior nose and ingestion or aspiration will be minimized. If the bleeding is active, the patient should be told to clear each nostril of clots and then pinch the entire cartilaginous portion of the nose for 15 minutes continuously. This is sometimes all that is required to stop the bleeding (however, the nose should always be reexamined to confirm hemostasis). During this time, the clinician should don protective clothing and eyewear and set up adequate lighting, a nasal speculum, and a suction device. The predominant side of the epistaxis should be noted. Bilateral bleeding suggests a posterior source. All mucosal surfaces of the nose should be examined for bleeding and the integrity of the septum confirmed. Observe the posterior oropharynx for 10–15 seconds to confirm whether fresh blood is flowing down the back wall. Bilateral bleeding suggests a posterior source as does a large amount of fresh blood in the oropharynx and little in the anterior nose.
Epistaxis from an anterior source can usually be controlled. In general, minimally invasive and technically simple methods are preferred, but refractory bleeding requires escalation to more invasive procedures. Some patients may benefit from gentle opiate or benzodiazepine sedation. While using the suction device to keep the field clear of blood, apply 1% phenylephrine, 4% cocaine, or 2% lidocaine-epinephrine solution with a cotton swab or pledget for vasoconstriction and local anesthesia. Alternatively these solutions may be sprayed onto the mucosal surface. When the bleeding site can be visualized, simple cautery with silver nitrate is often all that is required (see Figure 32–3). Exercise care to use only unilateral, brief applications. Roll the tip a short distance from above and over the bleeding site to prevent interference from blood flowing downward.
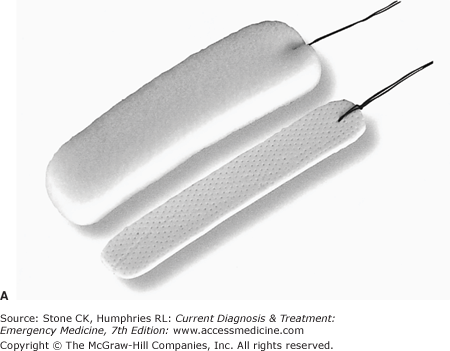
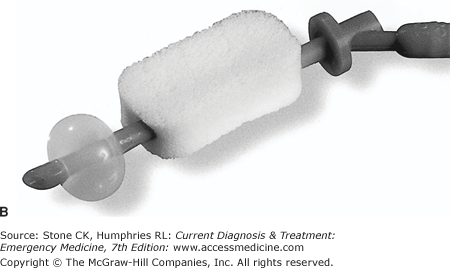
Bleeding that persists should be treated with packing. Several options are available. Cotton pledgets soaked with vasoconstrictive agents such as phenylephrine or lidocaine-epinephrine can be placed in the inferior nostril via narrow forceps and successively pushed superiorly until the nostril is packed. Commercial nasal tampons are simple to place (Figure 32–4A). They are inserted blindly along the inferior (floor) surface of the nostril and then expanded with the application of saline or 1:1 dilutions of the vasoconstricting agent. Take care not to injure the lateral turbinates. As the material expands, pressure is uniformly applied to the inner walls, tamponading bleeding. Procoagulant products (Surgicel, Gelfoam) may be used alone or in conjunction with other materials to augment the hemostatic effect.
If none of these methods is successful, a formal anterior pack with petroleum jelly gauze strip material may be necessary. It is placed in a similar fashion to the pled-gets: the end of a continuous strip is placed inferiorly and far back in the nose, then pushed up to tamponade the upper surfaces and make room for successive strips. The nostril must be fairly tightly packed, and most clinicians repeat the procedure on the other side if bleeding persists. Many authors suggest that patients with nasal packs should receive prophylaxis against bacterial sinusitis: amoxicillin–clavulanate, 875 mg twice daily for adults, 40 mg/kg/d divided two to three times daily for children. More study is needed, but some studies indicate antibiotics may not be needed in these patients. Packing material should be removed in 3–5 days. Patients with anterior packs can be discharged to home.
Posterior bleeding more typically arises from an arterial source and will not respond to the methods described above. Treatment of this entity usually requires the use of a nasal balloon device (Epistat, Nasostat) (Figure 32–4B). In addition to a posterior balloon, the specialized devices have an anterior tamponade apparatus (balloon or expanding tampon) that can be inflated or expanded independently. To prevent ischemia of the anterior nasal mucosa, the anterior portion is intended to exert less pressure than the posterior balloon. Insert it into the nostril such that the balloon is in the posterior portion of the nose. Then inflate the posterior balloon with saline until the point of discomfort. Properly placed, the posterior balloon may be all that is required to stop the bleeding. Usually, though, the anterior nose should be packed as well. Most patients with posterior packs should be admitted for airway observation, prophylactic antibiotics, and ENT consultation.
Most patients who present to the emergency department will have an acute obstruction (foreign body, trauma). Rarely, the problem is a complication of a chronic obstructive condition, such as an infection relating to a tumor or deviated septum.
Ask the patient how long the symptoms have been present and whether there were any precipitating events. In children, the most common cause of obstruction is a foreign body, often a colorful bead or a piece of food, and the history and diagnosis will be straightforward. Patients should also be queried regarding presence of a discharge. Purulent or foul-smelling discharge suggests an established organic foreign body. Nearly all cases of nasal obstruction will involve one side, negating the risk of airway compromise and allowing for outpatient workup of cases that defy emergency department management.
Look into each nostril with the otoscope or a nasal speculum. Most conditions can be characterized and treatment initiated based on direct inspection (Table 32–5).
| Diagnosis | Diagnostic Clues | Treatment |
|---|---|---|
| Abscess | Red, tender, fluctuant mass | Incise, drain, place temporary wick, or pack inside to prevent recurrence |
| Choanal atresia |