Drugs, Doses, Tables
Abciximab (Reopro)
ABCIXIMAB is a GP IIb/IIIa inhibitor, used as an adjunct to PTCA or atherectomy to prevent acute cardiac ischemia complications in patients at high risk for abrupt closure of the treated coronary vessel. It is intended to be used with aspirin and heparin therapy. ABCIXIMAB is FDA approved for patients with non–Q-wave MI or unstable angina with planned PCI within 24 hours.
Dosage
0.25 mg/kg as an IV bolus, given 10 to 60 minutes before start of PTCA or atherectomy, followed by a continuous infusion of 10 μg/min for 12 hours. (Continuous infusion is sometimes ordered at 0.125 μg/kg/min for 12 hours.)
Precautions
Use a dedicated IV line with an in-line filter.
May cause bradycardia, thrombocytopenia, increased risk of bleeding.
Ace Inhibitors
Angiotensin converting enzyme (ACE) inhibitors prevent the production of angiotensin II, a potent vasoconstructor that stimulates the production of aldosterone by blocking its conversion to the active form. The result is systemic vasodilation.
Primary therapeutic effects include:
Treatment of high blood pressures (acts as an arterial and venous dilator)
Decreased preload and afterload in patients with CHF (arterial vasodilation reduces the pressure the heart must pump against, making it easier to eject blood)
Prolonging survival in patients who have had a heart attack and now have a weak heart muscle
Prevention of heart attack and stroke in patients with vascular disease and in those who have diabetes with other vascular risk factors
Remember:
ACE inhibitors end in “pril.” Some common ones are captopril, lisinopril, and ramipril.
Acetadote
Acetadote is the only FDA-approved IV formulation of acetylcysteine (Mucomyst), developed specifically for use after ingestion of a hepatotoxic dose of acetaminophen.
Dosage
Load: 150 mg/kg in 250 cc D5W, infuse over 15 minutes
Maintenance: 50 mg/kg in 500 cc D5W over 4 hours, followed by 100 mg/kg in 1 L D5W over 16 hours
Considerations
Serum sample should be drawn at least 4 hours after ingestion.
Drug should be administered within 8 hours of ingestion for maximal protection against hepatic injury.
If time of ingestion is unknown, the drug level is unknown or cannot be interpreted, or is not available within the 8 hour time interval, the drug should be administered immediately if 24 hours or less have elapsed from the reported time of ingestion, regardless of the quantity reported to have been ingested.
Activase
(see Alteplase, p. 298)
Adenosine
Adenosine is a first-line antiarrhythmic used to treat PSVT and WPW. It has an unusually rapid onset, and its half-life is less than 10 seconds.
Dosage
6 mg IV rapid push over 1 to 3 seconds. After 1 to 2 minutes, if no resolution, give 12 mg IV rapid push over 1 to 3 seconds. May repeat once in 1 to 2 minutes.
Precautions
Immediately after administration, there is usually a distinct change in the electrocardiographic rhythm, such as PVCs, SB, or more commonly a short run of asystole. This usually resolves in seconds.
Adrenaline
(see Epinephrine, p. 312)
Aggrastat
(see Tirofiban, p. 336)
Alteplase
(see also Reteplase, p. 333; Tenecteplase, p. 334)
Alteplase (Activase, t-PA, rt-PA, Cathflo) is a tissue plasminogen activator that binds to fibrin, converting plasminogen to plasmin. This conversion allows the drug to dissolve the clot causing the blockage and restores blood flow and oxygen to the affected area.
Indications (Further Defined Within Each Category)
Acute myocardial infarction
Acute ischemic stroke
Acute massive pulmonary embolism
Catheter clearance
Contraindications to Use
Absolute
Severe uncontrolled hypertension
Active internal bleeding
History of CVA
Recent (within 2 months) intracranial or intraspinal surgery or trauma
Past or present bleeding disorder
Seizure at onset of stroke
Relative
Recent (within 10 days) major surgery
Recent (within 10 days) GI or GU bleeding
Recent trauma
Puncture of noncompressible vessel within 10 days
Diabetic or other hemorrhagic retinopathy
Traumatic CPR
Advanced age (>75 years)
Pregnancy
Current use of oral anticoagulants
History of uncontrolled hypertension (systolic >180 mm Hg, diastolic >110 mm Hg)
1. Alteplase for Acute Myocardial Infarction
Indications
Patient must be symptomatic with chest pain, typical of MI, for <6 hours, preferably <4 hours.
Chest pain longer than 6 hours, if intermittent with ongoing signs of ischemia.
A 1-mm ST segment elevation in two or more leads.
Dosing
There are two dosage regimens used in the management of acute MI; no studies have compared the success of the outcomes of either. The recommended total dose in both is based on patient weight, not to exceed 100 mg of the drug, because larger doses may cause intracranial bleeding.
Accelerated Infusion (90 Minutes)
| Patient Weight | IV Bolus Over 1 to 2 Minutes | IV Infusion Over Next 30 Minutes | IV Over Next 60 Minutes |
|---|---|---|---|
| Less than 67 kg | 15 mg | 0.75 mg/kg(not to exceed 50 mg) | 0.50 mg/kg(not to exceed 35 mg) |
| More than 67 kg | 15 mg | 50 mg | 35 mg |
Three-Hour Infusion Recommended Dose is 100 mg*
| First Hour (60%) | Second Hour (20%) | Third Hour (20%) |
|---|---|---|
| 10 mg IV bolus push, then 50 mg over remaining time | 20 mg | 20 mg |
| *For patients who weigh less than 67 kg, a dosage of 1.25 mg/kg administered over 3 hours as described above may be given. | ||
Concomitant Heparin Therapy
Although the value of anticoagulants during and after administration of Activase has not been fully studied, heparin has been administered concomitantly for 24 hours or longer in more than 90% of patients.
2. Alteplase for Acute Ischemic Stroke
Indications
Treatment should begin within 3 hours after the onset of stroke symptoms, and after exclusion of intracranial hemorrhage by CT scan.
Dosing
The recommended dosage is 0.9 mg/kg infused over 60 minutes, with 10% of the total dose administered as an initial IV bolus.
Do NOT use the cardiac dose!
Do not exceed 90 mg maximum dose.
Do NOT give aspirin, heparin, or Coumadin for 24 hours.
3. Alteplase for Acute Pulmonary Embolism
Dosing
The recommended dose is 100 mg IV over 2 hours. Heparin therapy should be given near the end of the alteplase infusion, or immediately after it, when the partial thromboplastin time (PTT) or prothrombin time (PT) returns to twice normal or less.
4. Alteplase for Catheter Clearance
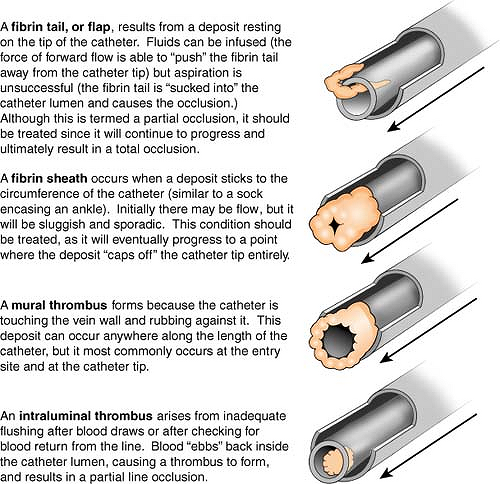
58% of catheter occlusions are thrombotic, occurring as a result of a thrombus within, surrounding, or at the tip of the catheter. The occlusions can be either:
Complete (infusion or aspiration is not possible);
Partial (can infuse, but unable to aspirate fluids).
Remember:
Both types of occlusion should be treated.
Dosing and Procedure
Withdraw 2 mL of reconstituted solution from vial.
Instill as much volume of the drug solution as possible into occluded catheter.
After 30 minutes of dwell time, assess catheter function by attempting to aspirate. Vigorous suction and excessive compression of catheter should be avoided during procedure! Excessive pressure could rupture catheter or cause expulsion of clot into the circulation. If the catheter is functional, gently aspirate 4 to 5 mL of blood to remove the drug and residual clot. Follow with an irrigation of sodium chloride. Never irrigate unless the alteplase has been aspirated. If the catheter is NOT patent, continue to Step 4.
After 2 hours of dwell time, reassess catheter function. If functional, gently aspirate 4 to 5 mL of blood to remove drug and residual clot. Follow with an irrigation of sodium chloride. If the catheter is NOT patent, continue to Step 5.
A second dose of alteplase may be instilled. (Depending on the institution, may require a physician order.) Repeat procedure beginning with Step 1.
If after a second attempt the catheter is not patent, stop procedure, recap line, and notify physician. No further attempts should be made without further investigation (e.g., chest x-ray, flow study).
Considerations in the Use of Alteplase
Observe for reperfusion arrhythmias, hypotension (acute MI).
Monitor for hypertension (acute stroke). Treat with NTG paste, labetalol, and/or Nipride.
Monitor lab results, especially coagulation profile. Watch for ecchymotic areas on patient, especially at flank.
Avoid intramuscular injection or arterial punctures.
Observe for bleeding, either internally or at external puncture sites.
Use a dedicated, nonfiltered line for infusion.
Acetaminophen may be ordered to control fever.
Amikacin
(see Therapeutic Drug Levels in Part 9, p. 357)
Aminophylline
A smooth muscle relaxant, aminophylline is sometimes useful in asthma and bronchospasms.
Mix: 500 mg in 500 mL D5W or 0.9 NS.
Infuse: If patient does not receive long-term maintenance theophylline, an IV loading dose of 5.6 mg/kg over 30 minutes is required. Maintenance IV dose ranges from 0.2 to 0.9 mg/kg/hr. Titrate infusion to therapeutic drug level of 10 to 20 mcg/mL.
Maintenance Dose of Aminophylline
| Adult, heavy smoker, 16–50 years | 0.7 mg/kg/hr (max 0.9 mg/kg/hr) |
| Adult, nonsmoker >16 years | 0.4 mg/kg/hr |
| Adult with cardiac decompensation, cor pulmonale, or liver dysfunction | 0.2 mg/kg/hr |
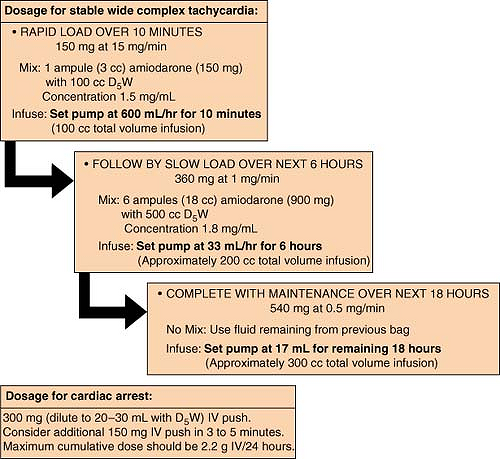
Amiodarone (Cordarone)
Amiodarone is a class III antiarrhythmic agent used for a wide variety of atrial and ventricular tachyarrhythmias, and for rate control of rapid atrial arrhythmias in patients with impaired LV function when digoxin has proven ineffective.
Precautions
May produce vasodilation and hypotension (most common).
May have negative inotropic effects.
May prolong QT interval.
Stable for 5 days when stored in glass bottles. A substantial loss of drug (40% over 120 hours) occurs from solutions stored in PVC bags or infused through PVC IV administration sets.
Terminal elimination is extremely long (half-life lasts up to 40 days).
Angiomax (Bivalirudin)
Intended for use with aspirin, Angiomax is a direct thrombin inhibitor with a naturally reversible mechanism of action. It is used as an anticoagulant (and as an alternative to unfractionated heparin) in patients undergoing percutaneous transluminal angioplasty. More recently, it has been approved for use in patients with or at risk of heparin-induced thrombocytopenia and thrombosis syndrome, who are undergoing percutaneous coronary intervention.
Dosage
1 mg/kg IV bolus, then 2.5 mg/kg/hr IV infusion over 4 hours, beginning just prior to PCTA procedure.
May give 0.2 mg/kg/hr IV infusion for up to 20 hours if necessary.
Precautions
Reduce dose with renal dysfunction.
Monitor for excessive bleeding, which would indicate the need to discontinue the drug.
Antidysrhythmic Drugs
Class Ia (sodium blockade)
Depresses sodium conduction into the cell, prolongs action potential duration, and increases refractory period. Effective in suppressing both atrial and ventricular dysrhythmias. The use of these agents is gradually on the decline, primarily as a result of the unfavorable risk-to-benefit ratio.
Examples: quinidine, procainamide
Class Ib
Decreases action potential duration and automaticity and increases fibrillation threshold in ventricles. Used widely in the acute treatment of ventricular tachycardia. (More recently, however, alternate drugs are increasingly being considered as first-line agents.)
Examples: lidocaine, phenytoin, Mexitil, tocainide
Class Ic
Depresses sinus node automaticity and prolongs conduction in atria, AV node, and ventricles. Used only for patients with life-threatening ventricular dysrhythmias. Contraindicated for use in patients with structural cardiac abnormalities and limited usefulness in the management of dysrhythmias.
Examples: flecainide (Tambocor), propafenone (Rythmol)
Class II (See also Beta Blockers, p. 305)
Blocks beta receptors, resulting in slowed heart rate and reduced automaticity in Purkinje fibers and increases effective refractory period of AV node. Used to slow ventricular rate of supraventricular tachycardias and may also help to control ventricular arrhythmias.
Class III (potassium blockade)
These drugs have a variety of pharmacokinetic and electrophysiologic properties. Prolongs duration of action potential.
Examples: amiodarone (Cordarone), ibutilide (Corvert), sotalol (Betapace), dofetilide (Tikosyn)
Class IV (See also Calcium Channel Blockers, p. 306)
Blocks calcium entry into the “slow” channels of the SA and AV nodes, thereby increasing the refractory period of the AV node and decreasing the ventricular rate. Their use in tachydysrhythmias is limited. Also relaxes smooth muscle and dilates coronary arteries.
Unclassed
Slows the AV node conduction and used primarily to treat paroxysmal supraventricular tachycardia.
Example: adenosine (Adenocard), digoxin
Argatroban
(see also HIT/HITT in Part 9, p. 350)
An anticoagulant that is a direct thrombin inhibitor, used primarily in patients diagnosed with HIT (heparin induced thrombocytopenia).
Mix: 250 mg in 250 cc 0.9 NS to make a 1 mg/1 mL concentration.
Infuse: Initial adult dosage at 2 mcg/kg/min continuous IV infusion. After initial dose, dose may be adjusted (not to exceed 10 mcg/kg/min) until PTT is 1.5 to 3 times the initial baseline (but not to exceed 100 seconds). Dose modification required for hepatic impairment, but not for renal impairment.
Considerations: Monitored by PTT.
Ativan (Lorazepam)
(see also Moderate Sedation, p. 323)
An antianxiety and amnestic, Ativan is used frequently in the ICU setting for sedation.
Mix: Best solubility is in concentrations of 0.1 mg/mL or 0.2 mg/mL. Dilute in D5W or NS.
Load (for sedation): 2 mg IV (may not be necessary if patient is receiving intermittent benzodiazepines, e.g., diazepam or midazolam).
Maintain: Continuous infusion of 0.5 to 1 mg/hr (0.25 mg/hr if patient is less agitated or has cardiorespiratory problems). Titrate to achieve sedation. Increase in 1-mg increments. Up to 5 to 10 mg/hr has been used. When sedation is adequate, wean to lowest amount needed.
Precautions
Very viscous; mix well and observe for crystallization (may occur more frequently if diluted in NS rather than D5W, and with 4 mg/mL vials rather than 2 mg vials). Frequent IV tubing changes may be necessary.
Refrigerate before dilution; protect from light.
Stable at room temperature for 12 hours in plastic, 24 hours in glass.
Continuous long-term use is not recommended. Withdrawal symptoms (i.e., rebound insomnia) can occur following cessation after as little as 1 week of therapy.
If long-term therapy is prescribed, abrupt discontinuation should be avoided and a gradual weaning schedule should be followed.
Banana Bag
Also known as a “rally bag,” this IV mixture (most commonly used for chronic alcoholics) contains vitamins and minerals to replenish nutritional deficiencies.
Mix: 1 L 0.9 NS with
10 mL MVI
100 mg thiamine
1 mg folic acid
Some institutions routinely add 1 to 3 g of magnesium sulfate.
Infuse: Typically infused over 4 to 8 hours.
Beta Blockers
Beta receptors are found in a number of places in the body: heart, lung, arteries, brain, and uterus, to name a few. Like a key in a lock, beta blocker drugs (also known as beta adrenergic blocking agents) fit into the beta receptor sites and prevent epinephrine and other catecholamines from binding to the receptors that cause a response.
The body has two main beta receptors:
Beta 1, responsible for heart rate and contractility.
Beta 2, responsible for function of muscles that control body functions but that you do not have control of (such as bronchial smooth muscle).
Remember:
Beta 1 works primarily on the heart (you have ONE heart).
Beta 2 works primarily on the lungs (you have TWO lungs).
Beta blocker drugs can be selective or nonselective.
Selective beta blocker drugs block beta 1 receptors more than they block beta 2 receptors, which means that they act primarily on the heart and will decrease heart rate and contractility. Some examples of selective beta blockers are metoprolol (Lopressor, Toprol XL), atenolol (Tenormin), esmolol (Brevibloc), and bisoprolol (Zebeta). Selective beta blocker drugs should be chosen when possible.
Nonselective beta blocker drugs block both beta 1 and beta 2 receptors, resulting in cardiac and pulmonary effects. These drugs are typically not given to patients with pulmonary disease because they may cause bronchoconstriction. Some examples of nonselective beta blockers are propranolol (Inderal), carvedilol (Coreg), labetalol (Normodyne, Trandate), and sotalol (Betapace).
Important Points
Avoid use in patients with bradycardia or heart blocks greater than first degree.
Use with caution when given concurrently with calcium channel blockers because of intensified cardiosuppression.
Beta blockers may mask signs of hypoglycemia in diabetic patients.
Most common side effects are bradycardia and hypotension (these resolve when medication is withdrawn), weakness, drowsiness, reduced peripheral circulation, constipation, and GI upset.
Bivalirudin
(see Angiomax, p. 303)
Brevibloc
(see Esmolol, p. 313)
Bumex (Bumetanide)
Bumex is a potent loop diuretic with rapid onset and short duration. It is indicated for treatment of edema associated with CHF and hepatic or renal dysfunction. Usual dose is 0.5 mg to 2 mg IV or PO daily, but use of a continuous drip in the ICU is not uncommon. Since 1 mg of Bumex has the potency equivalent of 40 mg of furosemide, a drip rate of 0.1 to 1 mg/hr is standard, though higher doses are sometimes seen. In a small number of patients, IV infusion may result in severe muscle cramps or stiffness. This complication appears to be dose related, and generally subsides when the drug is discontinued. Patients who experience this reaction may need to be diuresed with equivalent doses of furosemide (Lasix) instead.
Calcium
(see also Calcium in Part 9, p. 341; Hypocalcemia in Part 9, p. 352; Hypercalcemia in Part 9, p. 350)
Calcium is an electrolyte that helps maintain the function of the nervous and muscular systems. It is also important in blood coagulation.
Calcium Chloride (10%)
Each ampule (10 mL) contains 272 mg Ca (13.6 mEq) and is three times stronger than calcium gluconate.
Infuse IV push at a maximum rate of 1 mL/min (1.4 mEq/min).
Infuse IVPB at a maximum rate of 100 mg/min.
Calcium Gluconate (10%)
Each ampule (10 mL) contains 90 mg Ca (4.5 mEq) and is one third the strength of calcium chloride.
Infuse IV push at a maximum rate of 1.5 mL/min (7.7 mEq/min).
Infuse IVPB at a maximum rate of 200 mg/min.
Calcium Channel Blockers
Calcium channel blockers inhibit calcium influx across cardiac and smooth muscle cells, resulting in decreased myocardial contractility and decreased oxygen demand while dilating coronary arteries and peripheral arterioles.
Primary therapeutic effects include:
Treatment of hypertension.
Control of angina.
Management of certain types of abnormal heart rhythms (e.g., atrial fibrillation).
Use after a heart attack when beta blockers cannot be tolerated.
Management of cardiomyopathy.
Prevention of vascular spasm after subarachnoid hemorrhage (nimodipine only).
There are many calcium channel blockers on the market, and their differences vary widely. For example, amlodipine (Norvasc) has very little effect on heart rate and contraction, so it is a good choice for use in individuals who have heart failure or bradycardia. Conversely, drugs like diltiazem (Cardizem) have their greatest effect on the heart and in reducing the strength of contraction, so they are best utilized for tachycardias.
Remember:
Do not give calcium channel blockers to patients with sick sinus syndrome or heart blocks greater than first degree.
Risk of AV block is increased with concurrent use of digoxin.
Calcium channel blockers should be administered several hours apart from beta blockers to minimize cardiosuppression.
Diltiazem and verapamil have the most interactions with other drugs. They may increase blood levels of Tegretol, Zocor, Lipitor, and Mevacor, leading to toxicity.
Cardene
(see Nicardipine, p. 327)
Cardizem
(see Diltiazem, p. 309)
Cathflo
(see Alteplase, p. 298)
Cerebyx (Fosphenytoin)
Cerebyx is indicated for short-term parenteral administration when other means of phenytoin administration are unavailable, inappropriate, or deemed less advantageous. It is used for control of generalized convulsive status epilepticus and prevention and treatment of seizures occurring during neurosurgery. Cerebyx should always be prescribed in phenytoin sodium equivalent (PE) units.
Dosage: Before IV administration, Cerebyx should be diluted in D5W or 0.9% NS for injection to a concentration ranging from 1.5 to 25 mg PE/mL.
Load: 10 to 20 mg PE/kg given IV or intramuscularly. If administered IV, infuse at a rate no greater than 150 mg PE/min.
Maintenance: 4 to 6 mg PE/kg/day
Precautions
High risk of hypotension; be sure to administer IV slowly.
Observe patient throughout the period when maximal drug concentrations occur (10–20 minutes after completion of infusion).
Cholinergic Agents
Also known as parasympathomimetics, cholinergic drugs produce the same effects as the body’s parasympathetic nervous system (the part of the peripheral nervous system responsible for dealing with everyday activities such as digestion, sphincter muscle relaxation, salivation, and reducing heart rate and blood pressure). Nerve impulses in the parasympathetic nervous system are transmitted from one nerve junction to another with the help of acetylcholine, and cholinergic agents work by either mimicking the effect of acetylcholine or blocking the effects of acetylcholinesterase (giving acetylcholine a longer life). Cholinergic drugs are frequently used in the diagnosis of myasthenia gravis and are widely used in surgery to reduce urinary retention and to counteract the effects of some muscle relaxants given.
Conversely, anticholinergic drugs are used to inhibit parasympathetic nerve impulses by blocking the binding of acetylcholinergic to receptor sites in the nerve cells. Anticholinergics are used to treat a variety of disorders such as gastrointestinal cramps, urinary bladder spasm, asthma, motion sickness, muscular spasms, and as an aid to anesthesia.
Chronotropic Agents
Chronotropic agents affect the heart rate. Positive chronotropes (e.g., epinephrine and Isuprel) will increase the heart rate, while negative chronotropes (e.g., beta blockers, calcium channel blockers, such as diltiazem) will decrease the heart rate.
Cisatracurium
(see Nimbex, p. 328)
Cordarone
(see Amiodarone, p. 302)
Corlopam (Fenoldopam)
A rapid-acting vasodilator used for short-term management (up to 48 hours) of severe hypertension, including malignant hypertension with deteriorating end organ function.
Mix: In 0.9% NS or D5W as directed in the following table:
Corlopam Concentration
| mL of Concentrate (mg of Drug) | Added to | Final Concentration |
|---|---|---|
| 4 mL (40 mg) | 1,000 mL | 40 μg/mL |
| 2 mL (20 mg) | 500 mL | 40 μg/mL |
| 1 mL (10 mg) | 250 mL | 40 μg/mL |
Infuse: Start dosage at 0.03 to 0.1 μg/kg/min, and titrate every 15 minutes by 0.05 to 0.1 μg/kg/min until desired blood pressure is achieved. No bolus is required.
Corlopam Maintenance (Concentration 40 μ/mL)
| Dose (μg/kg/min) | 0.25 | 0.05 | 0.1 | 0.2 | 0.3 | 0.4 | 0.5 | 0.6 | 0.7 | 0.8 |
|---|---|---|---|---|---|---|---|---|---|---|
| Weight (kg) | Infusion Rate mL/hr | |||||||||
| 40 | 1.5 | 3 | 6 | 12 | 18 | 24 | 30 | 36 | 42 | 48 |
| 50 | 1.8 | 3.7 | 7.5 | 15 | 22.5 | 30 | 37.5 | 45 | 52.5 | 60 |
| 60 | 2.2 | 4.5 | 9 | 18 | 27 | 36 | 45 | 54 | 63 | 72 |
| 70 | 2.6 | 5.2 | 10.5 | 21 | 31.5 | 42 | 52.5 | 63 | 73.5 | 84 |
| 80 | 3 | 6 | 12 | 24 | 36 | 48 | 60 | 72 | 84 | 96 |
| 90 | 3.3 | 6.7 | 13.5 | 27 | 40.5 | 54 | 67.5 | 81 | 94.5 | 108 |
| 100 | 3.7 | 7.5 | 15 | 30 | 45 | 60 | 75 | 90 | 105 | 120 |
| 110 | 4.1 | 8.2 | 16.5 | 33 | 49.5 | 66 | 82.5 | 99 | 115.5 | 132 |
| 120 | 4.5 | 9 | 18 | 36 | 54 | 72 | 90 | 108 | 126 | 144 |
Considerations
Infusion can be abruptly discontinued without adverse effect, or may be tapered gradually.
There are no known contraindications to Corlopam.
Adverse reactions include allergic-type reactions (anaphylactic symptoms), tachycardia, hypotension, hypokalemia (monitor potassium levels every six hours after initiating a bolus), or an increase in intraocular pressure.
Avoid concomitant use of β-blockers.
Corvert
(see Ibutilide, p. 318)
Coumadin
Coumadin (warfarin) is an anticoagulant that inhibits vitamin K and directly interferes with clotting factors II, VII, IX, and X.
Dosage: 2 to 10 mg PO daily, based on PT ratio (1.5–2.5 × control) or INR of 2 to 3.
Remember:
The half-life of Coumadin is 36 to 42 hours; therefore, an increase in the INR is not seen until 2 days after the first dose is administered.
Precautions
Anticoagulant effect can be reversed by 5 to 25 mg of vitamin K given IM or SQ.
Dalteparin
(see Fragmin, p. 315)
Dexmedetomidine
(see Precedex, p. 331)
Diltiazem (Cardizem)
Diltiazem is a calcium channel blocker used in SVT, atrial fibrillation, angina, and hypertension.
Dosage: 0.25 mg/kg IV push over 2 minutes (average 20 mg IV). If no response, may repeat in 15 minutes at 0.35 mg/kg over 2 minutes.
Mix: 250 mg in 250 mL D5W
Infuse: 10 to 15 mg/hr; titrate to heart rate.
Precautions
May cause bradycardia, headache, weakness, GI disturbances, dizziness. Concurrent IV administration with beta blockers can cause severe hypotension. Avoid in patients receiving oral beta blockers.
Diprivan
(see Propofol, p. 332)
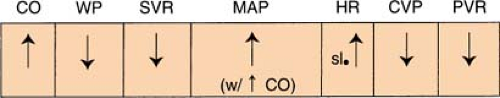
Dobutamine (Dobutrex)
Dobutamine is a synthetic sympathomimetic catecholamine with inotropic, chronotropic, and vasodilator effects. It is useful in treating heart failure (especially with an increase in SVR and PVR by increasing contractility with no significant increase in heart rate.) The blood pressure is increased because of the increased cardiac output. The vasodilatory effects of the drug, however, are more pronounced in some patients, and may actually cause a decrease in the blood pressure.
Infuse: 2 to 10 μg/kg/min (can go up to 40 μg/kg/min with physician approval)
Mix: 250 mg in 250 mL D5W or 0.9% NS
Dobutamine Maintenance (250 mg in 250 mL)
| Dose (μg/kg/min) | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| Weight (kg) | Infusion Rate (mL/hr) | |||
| 50 | 6 | 9 | 12 | 15 |
| 60 | 7 | 10 | 14 | 18 |
| 70 | 8 | 12 | 17 | 21 |
| 80 | 9 | 14 | 20 | 24 |
| 90 | 11 | 16 | 22 | 27 |
| 100 | 12 | 18 | 24 | 30 |
Or mix: 500 mg in 250 mL D5W or 0.9% NS
Dobutamine Maintenance (500 mg in 250 mL)
| Dose (μg/kg/min) | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| Weight (kg) | Infusion Rate (mL/hr) | |||
| 50 | 3 | 4.5 | 6 | 7.5 |
| 60 | 4 | 5 | 7 | 9 |
| 70 | 4 | 6 | 8.5 | 10.5 |
| 80 | 5 | 7 | 10 | 12 |
| 90 | 5 | 8 | 11 | 13.5 |
| 100 | 6 | 9 | 12 | 15 |
Dobutrex
(see Dobutamine, p. 309)
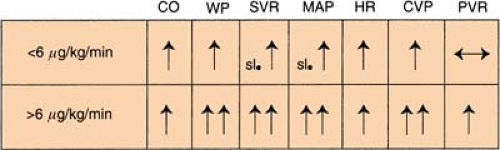
Dopamine (Intropin)
Dopamine is a natural catecholamine that is the immediate precursor of norepinephrine. It is used to raise low blood pressure that is refractory to fluid therapy, to treat heart failure, and to correct hemodynamic imbalance in shock syndrome. Onset of the drug is rapid, usually 5 minutes, with duration lasting about 10 minutes.
Infuse:
Low dosage (renal perfusion): 1 to 3 μg/kg/min (generally accepted but institution specific)
Medium dosage (increases contractility): 3 to 10 μg/kg/min
Medium dosage (produces vasoconstriction): >10 μg/kg/min
High dosage (works like Levophed): >20 μg/kg/min
Mix: 400 mg in 250 mL D5W or 0.9% NS
Dopamine Maintenance (400 mg in 250 mL)
| Dose (μg/kg/min) | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| Weight (kg) | Infusion Rate (mL/hr) | |||
| 50 | 4 | 6 | 7.5 | 9 |
| 60 | 4.5 | 7 | 9 | 11 |
| 70 | 5 | 8 | 10.5 | 13 |
| 80 | 6 | 9 | 12 | 15 |
| 90 | 7 | 10 | 13.5 | 17 |
| 100 | 7.5 | 11 | 15 | 19 |
Or mix: 400 mg in 500 mL D5W or 0.9% NS
Dopamine Maintenance (400 mg in 500 mL)
| Dose (μg/kg/min) | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| Weight (kg) | Infusion Rate (mL/hr) | |||
| 50 | 8 | 11 | 15 | 19 |
| 60 | 9 | 14 | 18 | 23 |
| 70 | 11 | 16 | 22 | 26 |
| 80 | 12 | 18 | 24 | 30 |
| 90 | 14 | 20 | 27 | 34 |
Or mix: 800 mg in 250 mL D5W or 0.9% NS
Dopamine Maintenance (800 mg in 250 mL)
| Dose (μg/kg/min) | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| Weight (kg) | Infusion Rate (mL/hr) | |||
| 50 | 2 | 3 | 4 | 5 |
| 60 | 2 | 3 | 4.5 | 6 |
| 70 | 3 | 4 | 5 | 6.5 |
| 80 | 3 | 4.5 | 6 | 7.5 |
| 90 | 3 | 5 | 7 | 8.5 |
| 100 | 4 | 5.5 | 7.5 | 9 |
Precautions
Renal ischemia occurs at high doses.
Causes tissue sloughing if IV infiltrates (use Regitine).
Dromotropic Agents
Dromotropic agents affect atrial-ventricular (AV) nodal conduction. A positive dromotrope will increase the conduction (e.g., atropine sulfate), and a negative dromotrope will slow conduction (e.g., Lanoxin).

Full access? Get Clinical Tree