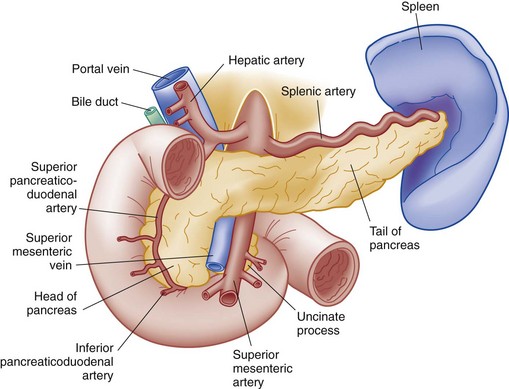
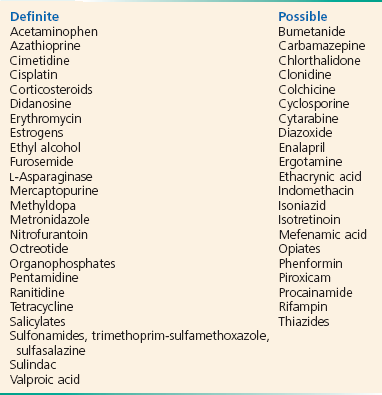
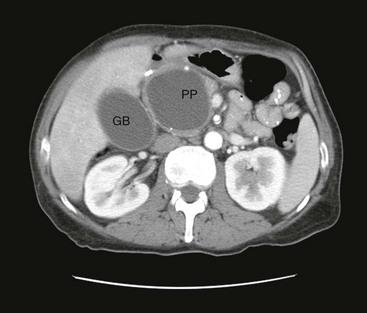
Chapter 91 The pancreas is a retroperitoneal organ extending across the posterior abdomen in the epigastrium that provides essential endocrine and exocrine functions (Fig. 91-1). In the general population, diabetes is the most common disorder of the pancreas, followed by pancreatitis. Acute pancreatitis is an inflammatory process of the pancreas usually associated with abdominal pain, elevated pancreatic enzymes, and variable involvement of other regional tissues or remote organ systems. Both local and systemic complications may occur. Repeated bouts of pancreatitis from any cause may eventuate in chronic pancreatitis as a result of permanent alterations in function and morphology. Chronic pancreatitis is an ongoing inflammation of the pancreas, which may be interrupted by spells of acute pancreatitis. Pancreatic tumors may develop from the endocrine or nonendocrine structures. These tumors may cause acute pancreatitis, which usually manifest in an indolent fashion. The most common is adenocarcinoma originating from the pancreatic ducts. The first reports of pancreatitis date to the 1700s, and the first accurate study and description were completed by Fitz in 1889.1 He noted that performing surgery in the early stages of this disease was “extremely hazardous.” Since then, the understanding of pancreatitis has evolved; however, treatment remains largely supportive rather than curative. Advances in care have decreased hospital mortality for all patients with pancreatitis, from 10 to 15% as reported 20 years ago to 4 to 7% more recently.2,3 Most patients with pancreatitis have a mild course; however, 10 to 15% of cases will progress to severe disease, with a mortality rate in this subset of 20 to 50%. Children are at increased risk for death, with mortality rates of approximately 10%.4 Severity also is increased in obese patients. Pancreatitis can be classified as mild or severe, the latter category of the disease being defined by the presence of organ failure or local complications, such as necrosis, pseudocysts, or abscess.2,5 The gravity of the impending illness may not be apparent at the initial presentation, and in all patients, disease progression and outcome are difficult to predict at onset. Death in the first week usually is from pulmonary failure, multiorgan failure, or cardiovascular collapse. Later deaths are more likely to be from infective complications. In approximately 40% of cases, fatal pancreatitis on autopsy was undiagnosed. Therefore pancreatitis should be suspected in moribund patients with multiorgan failure, particularly elders. The incidence of acute pancreatitis in the United States ranges from 4.8 per 100,000 to 40 per 100,000, varying with age, gender, and social characteristics of the population studied.2 The incidence appears to be increasing, although the increase may be related to both improved diagnosis and greater prevalence of risk factors. Gallstones are the most common obstructive cause of pancreatitis and occur more commonly in women than in men, with peak symptomatic incidence between the ages of 50 and 60 years. Some variations of ductal anatomy are associated with increased risk of obstruction. Many gallstones are asymptomatic; however, among people with gallstones, pancreatitis occurs with a frequency of 8 to 20 per 1000 person-years 2. Alcoholic pancreatitis is more common in men than in women. In most (but not all) populations, this is the second leading cause of pancreatitis after obstructive causes. In children, trauma is the most common identifiable cause of acute pancreatitis.4,6 Many of the pathobiologic responses that occur in acute pancreatitis, such as edema, inflammation, and parenchymal cell death, are easy to conceptualize. However, knowledge about the exact molecular mechanisms that ultimately lead to these events is still evolving. Intense research to further the understanding of pancreatic intracellular digestive enzyme activation, pancreatic inflammatory response, and cell death responses, such as necrosis and apoptosis, is ongoing, with the aim of identifying new strategies for treatment.7 Acute pancreatitis may be divided into three pathologic phases. The first phase is the local inflammation from obstruction of the pancreatic or bile ducts, direct toxicity of the pancreatic cells, toxins, infections, trauma, or idiopathic causes. Local inflammation subsequently causes premature activation of pancreatic enzymes, such as trypsinogen and zymogen, either in the ducts or in the acinar cells.2,8 This activation causes the release of enzymes that are intended to digest dietary proteins and fats; instead they produce cellular breakdown and pancreatic tissue autodigestion. Initially the inflammatory process is localized, creating focal pancreatic injury and edema. With increasing severity, the inflammation becomes generalized and causes necrosis of the pancreas and spreads to the surrounding fat and tissues. During this second phase of generalized injury, there may be necrosis of the pancreatic ducts as well as the vascular structures, leading to hemorrhage. Necrosis involving more than 30% of the pancreas increases both morbidity and mortality.9,10 Enzyme activation, inflammation, and necrosis cause a variety of complications. For example, fluid collections develop in 30 to 50% of patients with severe pancreatitis.10 Over time, a fibrinous or granulation wall may form around this fluid collection, creating a pseudocyst. Thus, pseudocysts are not present in the initial phases of pancreatitis but instead develop over 4 to 6 weeks. Fluid collections, necrotic areas, or pseudocysts may become infected in a small number of cases, usually after several weeks. In addition, irritation of the surrounding bowel is common, creating bowel wall edema, ileus, and third-spacing of fluid. Formation of ascites is common and, together with bowel edema, can lead to significant intravascular fluid loss and hypotension. The final stage of injury occurs with the development of multiorgan damage. Because of the release of inflammatory mediators, the initial localized inflammatory response may cause a systemic immune response syndrome (SIRS), resulting in multiple organ failure. This is a sepsis-like response, and any organ system can be involved, potentially resulting in myocardial depression, acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC), or renal failure.2,11 Pancreatitis has several causes, but the vast majority of cases (80%) will be a result of either gallstones or alcohol, with gallstones the most common cause in most series (approximately 45% vs. 35%)2 (Box 91-1). The exact pathomechanism of biliary pancreatitis is not clear. Either a stone within the bile duct applies transmural pressure on the pancreatic duct, or a stone in the common channel of the pancreatic duct or common bile duct causes obstruction. Obstruction or pressure on the pancreatic duct causes bile reflux or increased pressure of pancreatic secretions. Either mechanism leads to the activation of pancreatic enzymes, setting off the cascade of pancreatitis. Many cases presumed to be idiopathic probably are caused by small stones, sludge, or crystals that are too small to be detected on ultrasound examination but may be seen on endoscopic retrograde cholangiopancreatography (ERCP). This cause of pancreatitis is potentially correctable; if it is missed, recurrences are likely. Alcohol is the cause of approximately 35% of pancreatitis cases. As with the other causes of pancreatitis, the mechanism by which alcohol is toxic to the pancreas is not well understood. Possible mechanisms include toxic effects of the ethanol metabolite acetaldehyde, ethanol-related lipid metabolism, or spasm of the sphincter of Oddi. Patients with alcoholic pancreatitis usually have 5 to 10 years of chronic alcohol use before the onset of pancreatitis.8 In addition to alcohol, many medications and toxins may cause pancreatitis, including didanosine, pentamidine, oral contraceptives, and selected scorpion venoms12 (Box 91-2) Pancreatitis can be caused by hypertriglyceridemia, with levels more than 500 mg/dL being implicated. In pregnancy, both gallstones and increased triglyceride levels can cause pancreatitis.8 When this occurs, both maternal and fetal mortality rates are high. Blunt and penetrating abdominal trauma can disrupt the ductal system and the pancreatic cells, setting off the enzyme cascade that will result in acute pancreatitis. Pancreatitis also may result from iatrogenic ductal injury in 1 to 10% of ERCP procedures.2,8,13 Likewise, postoperative pancreatitis is well recognized and carries a higher mortality than that associated with other causative disorders. Although both viral and bacterial disorders may precipitate pancreatitis, the two most common viral causes of pancreatitis are mumps and Coxsackievirus B infection. Pancreatitis is more common in patients with human immunodeficiency virus (HIV) infection than in the general population.14 In addition to the common etiologic risk factors for pancreatitis, this population is at additional risk because of the risk of opportunistic infections, toxicity from HIV-specific medications, and acquired immunodeficiency syndrome (AIDS)–related cancers.2,12 Acute pancreatitis is ultimately classified as idiopathic in approximately 10% of cases.2 Suspected but uncertain causes may include sphincter of Oddi dysfunction and pancreas divisum, which arises from a failure of the dorsal and ventral ducts to fuse. With this entity, most of the pancreatic juice flows through the minor pancreatic duct and papilla. The etiologies of pancreatitis in adults and children are similar, although incidence rates for specific causative disorders are different. Trauma (including child abuse), infection, and idiopathic causes account for 70% of the cases in children.4 Hereditary pancreatitis is an autosomal dominant trait, with onset frequently noted during childhood. Other causes include infections and congenital anomalies. Almost all patients with pancreatitis give a history of abdominal pain, most commonly in the midepigastric area; however, the pain also can be in the right or left upper quadrant. If significant inflammation is present, the pain may be diffuse and the patient may have difficulty localizing the discomfort. Typically, onset of symptoms is relatively rapid, increasing in severity over a few hours. The pain generally is described as constant and severe and may radiate to the midback. The degree of pain does not correlate with the severity of disease. Even though gallstones are frequently the cause of pancreatitis, the onset of pain is not usually related to eating. Nausea and vomiting often will accompany the pain. Although the discomfort may be lessened by lying on the side or sitting up, more typically little relief is obtained with position change, moving, eating, vomiting, or bowel movement. Colicky pain or pain that waxes and wanes suggests another diagnosis. Approximately 50% of patients will have a history of similar abdominal pain that may represent a previous episode of biliary colic or mild pancreatitis.15 On physical examination, vital signs may be stable but frequently are abnormal. Hypotension, tachycardia, and shock indicate severe disease with complications or an alternate diagnosis. Vital signs also may be influenced by pain (tachycardia, tachypnea, hypertension) or alcohol withdrawal (tachycardia, hypertension, fever). A low-grade fever is present in approximately half of patients with pancreatitis, both at presentation and for the first several days thereafter, even in the absence of infection.9 A high fever is uncommon during the acute phase of pancreatitis; infection is usually a late complication. Ongoing evaluation should include pulse oximetry because acute hypoxia is an indicator of systemic complications and severe disease. Coagulopathy develops from circulating proteases that affect the coagulation cascade. Acute tubular necrosis can cause acute renal failure and results from the effects of circulating inflammatory mediators or from hypotension and hypoperfusion. Ultimately, multisystem organ failure will occur if the balance of proinflammatory cytokine production overwhelms the anti-inflammatory response, which seeks to restrict the inappropriate movement of proinflammatory agents into the circulation.15 Late complications occur after the second week of illness and include involvement of local structures, abscess formation (1-4%), gastrointestinal bleeding from stress ulcers, splenic vein thrombosis, rupture of pancreatic pseudoaneurysms, fistula formation, splenic rupture, venous thrombosis, and right hydronephrosis. Pancreatic pseudocysts develop in 1 to 8% of patients after 4 to 6 weeks and are more common with alcoholic pancreatitis (Fig. 91-2). Long-term complications of acute pancreatitis include recurrent or chronic pancreatitis, diabetes mellitus, and digestive and malabsorption problems. Amylase Assay.: Amylase is an enzyme that cleaves carbohydrates. It is produced primarily in the salivary glands and pancreas, although it also can be found in small amounts in the fallopian tubes, ovary, testis, muscle, intestines, and other organs. Elevations of amylase may be seen in healthy persons, patients with ectopic pregnancy, macroamylasemia, parotitis, renal failure (decreased clearance), mesenteric ischemia, bowel obstruction or infarction, perforated duodenal ulcer, acute peritonitis from other causes, and many other diseases. Pancreatic amylase can be differentiated from other sources of amylase by electrophoresis, a test that is not readily available in the emergency department (ED). Because of the other nonspecific sources of amylase, elevations of amylase lack specificity for the diagnosis of pancreatitis.16 In acute pancreatitis, amylase rises within 6 to 24 hours, peaks in 48 hours, and normalizes in 3 to 7 days. Thus the sensitivity of amylase decreases after the first 24 to 48 hours.16 Lipase Assay.: Lipase is a pancreatic enzyme that hydrolyzes triglycerides and has been used both as an adjunctive test and an alternative test for the diagnosis of pancreatitis. Unfortunately, lipase assays are associated with many of the same pitfalls as amylase assays. In the presence of pancreatic inflammation, lipase levels increase within 4 to 8 hours and peak at 24 hours. The levels stay elevated longer than amylase levels, falling over 8 to 14 days,8,16 thus providing greater sensitivity in patients with delayed presentations. Lipase, like amylase, is present in other tissues and tends to be elevated in similar clinical situations. Improved assays have rendered lipase more specific than amylase. Yet, there are still nonpancreatic causes of elevations of lipase, such as duodenal ulcers, bowel obstruction, and idiopathic causes.8,16 Comparisons between amylase and lipase are limited by the lack of a true “gold standard” for the diagnosis of pancreatitis, as well as the choice of cutoff values used for the diagnosis. Despite these limitations, lipase is at least as sensitive as and probably more specific than amylase (specificity of 80 to 99%). At values five times the upper limits of normal, lipase is 60% sensitive and 100% specific. The use of twice the upper limit of normal has been recommended to decrease the possibility of missing the diagnosis of pancreatitis.16 Expert guidelines recommend the use of lipase over amylase in the diagnosis of pancreatitis.17,18 The degree of elevation of amylase or lipase is not a marker of disease severity.3 For example, compared with nonalcoholic patients, alcoholics will frequently have lower amylase levels but may have more severe disease. In a patient with prolonged abdominal pain or a history of pancreatitis, elevated biomarkers for longer than a week may suggest pseudocyst or pancreatic absess.19 Use of the amylase-to-lipase ratio has not proved helpful in the determination of a specific cause of pancreatitis.14
Disorders of the Pancreas
Background
Acute Pancreatitis
Principles of Disease
Etiology
Clinical Features
Complications
Diagnostic Strategies

Full access? Get Clinical Tree


Disorders of the Pancreas
Only gold members can continue reading. Log In or Register to continue