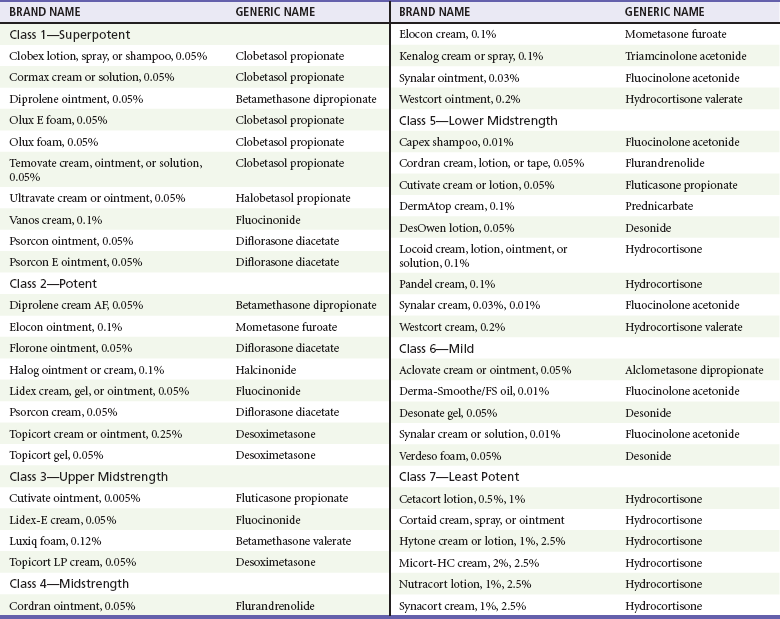
Chapter 120 The diagnosis is aided by the configuration of the lesions and distribution on the body’s surface. On occasion, a configuration is specific for a disease; however, the morphologic appearance of the primary lesion is usually given more diagnostic weight (Table 120-1). Finally, many skin diseases have preferential areas of involvement, so the location of the eruption may aid in diagnosis. Several serious dermatologic disorders, such as Stevens-Johnson syndrome, may be manifested initially with lesions on mucous membranes only, thus making an examination of the mucous membranes an important part of a dermatologic evaluation. Table 120-1 Modified from Lookingbill DP, Marks JG: Principles of Dermatology, 3rd ed. Philadelphia, Saunders, 1993. Topical corticosteroids are commonly used for a variety of inflammatory skin conditions. They induce topical vasoconstriction, depress local immunity, and cause skin thinning with prolonged use. Systemic absorption and side effects are possible. A variety of formulations are available (Table 120-2). The potency of steroids depends on the specific drug, its concentration, and the method of delivery (i.e., whether cream or ointment is used, how often it is applied, whether an occlusive dressing is placed). It is wise for clinicians to familiarize themselves with one or two high-, medium-, and low-potency steroids to limit possible errors. So-called mega potency topical steroids are generally not initiated without consulting a dermatologist. The lowest potency medication available should be used around natural orifices to minimize systemic absorption. Table 120-2 Modified with permission from National Psoriasis Foundation: Topical steroids potency chart. Available at http://www.psoriasis.org/page.aspx?pid=469. Accessed August 16, 2011. The dermatophytoses are superficial fungal infections that are limited to the skin.1 A variety of lesions may occur, but the most common are scaling, erythematous papules, plaques, and patches, which often have a serpiginous or wormlike border. Dermatophytes generally grow best in excessive heat and moisture and grow only in the keratin or outer layer of the skin, nails, and hair. Keratin tends to accumulate in body folds, such as between toes and in the inguinal area, the axilla, and the inframammary areas. With the exception of tinea capitis, dermatophyte infections are not markedly contagious. Clinical Features.: Tinea capitis is a fungal infection of the scalp. Although it is primarily regarded as a disease of preschool children, tinea capitis is increasingly recognized in adults, infants, and neonates. It is more common among African Americans, although the reasons for this are unknown.2 Nosocomial transmission of dermatophyte infections, such as Trichophyton tonsurans, has also been reported.3 Recent outbreaks in the United States caused by T. tonsurans differ from epidemics of the 1940s and 1950s caused by Microsporum audouinii in that many patients have seborrheic-like scaling in the absence of alopecia.2 Black dots, representing hair broken off near the scalp, may be noted clinically. Hair loss is the result of hyphae growing within the shaft, rendering it fragile, so that the hair strands break off 1 to 2 mm above the scalp. Circular patches of partial baldness may result. The disease may be transmitted by close child-to-child contact and contact with household pets, hats, combs, barber’s shears, and similar items. Complications include lymphadenitis, bacterial pyoderma, tinea corporis, pigmenting pityriasis alba, id reaction after treatment, secondary bacterial infection, and scarring alopecia.2 Differential Considerations.: The differential diagnosis of tinea capitis includes alopecia areata, atopic dermatitis, nummular eczema, bacterial infection, psoriasis, seborrheic dermatitis, “tinea” amiantacea, trichotillomania (hair pulling), and Langerhans cell histiocytosis. Diagnostic Strategies.: A KOH preparation is not helpful in the presence of a kerion or in the absence of alopecia, in which case a fungal culture specimen should be obtained. Management.: Systemic therapy is required for tinea capitis. Treatment usually begins with griseofulvin 20 mg/kg/day, usually not to exceed 1000 mg/day, taken as a single dose with a fat-containing food for a minimum of 6 weeks or 2 weeks after clinical resolution of inflammation. Higher doses may be needed. Griseofulvin can cause sun sensitivity. If treatment is initiated in the ED, refer the patient for a monthly follow-up evaluation. Alternative therapy includes fluconazole 200 mg/day (adults) or 3 to 5 mg/kg/day (children), itraconazole 200 mg daily (adults) or 3 to 5 mg/kg/day (children) for 4 to 6 weeks, oral terbinafine 3 to 6 mg/kg/day (children) or 250 mg/day (adults) for 4 to 6 weeks, and terbinafine cream once a day for 8 weeks. T. tonsurans species appear to be more sensitive to newer treatment modalities and require a shorter course of treatment than for Microsporum species. Selenium sulfide shampoo, 250 mg twice weekly, decreases shedding of spores. Family members should be evaluated. Clinical Features.: Tinea corporis is the classic “ringworm” infection. Its characteristic presentation is a sharply marginated, annular lesion with raised or vesicular margins and central clearing (Fig. 120-1). Lesions may be single or multiple; multiple lesions are occasionally concentric. Tinea cruris, which involves the groin, is similar in appearance and may also include the perineum, thighs, and buttocks, but the scrotum is characteristically spared. Differential Considerations.: The differential diagnosis of tinea cruris includes granuloma annulare, psoriasis, intertrigo with secondary candidiasis, and erythrasma. Management.: Infections of the body, groin, and extremities usually respond to topical measures alone. A number of effective topical antifungal agents are available, including clotrimazole (Lotrimin), haloprogin (Halotex), miconazole (Micatin), tolnaftate (Tinactin), terbinafine, naftifine, and griseofulvin 1%. Two or three daily applications of the cream form of any of these preparations result in healing of most superficial lesions in 1 to 3 weeks.4 Acute inflammatory lesions displaying oozing or blisters are treated additionally (four times a day) with open, wet compresses of Burow’s solution, an aluminum acetate solution that is useful as a soothing wet dressing for inflammatory skin conditions. Tinea pedis, or athlete’s foot, appears with scaling, maceration, vesiculation, and fissuring between the toes and on the plantar surface of the foot. In extensive cases, the entire sole may be involved. A secondary bacterial infection may occur. The vesicular pustular form of tinea pedis should be considered when vesicles and pustules on the instep are noted. The differential diagnosis includes contact dermatitis and dyshidrotic eczema. A KOH preparation is helpful to differentiate between these processes. Interdigital lesions may cause minimal symptoms and serve as a portal of entry for bacterial cellulitis. Treatment options include terbinafine 1% cream twice daily for 2 to 4 weeks; miconazole 2% cream, powder, or spray twice daily for 2 to 4 weeks; and clotrimazole 1% cream, solution, or lotion twice daily for 2 to 4 weeks.5 For severe disease or if topical treatment has failed, use terbinafine 250 mg orally daily for 2 weeks, fluconazole 150 mg orally weekly for 2 to 4 weeks, or griseofulvin 500 mg orally daily for 2 weeks. Clinical Features.: Tinea versicolor is a superficial yeast infection caused by Pityrosporum ovale. Superficial scaling patches occur mainly on the chest and trunk but may extend to the head and limbs. As the name implies, lesions can be a variety of colors, including pink, tan, and white. The disease may be associated with pruritus, but medical care is often sought because the spots do not tan. On physical examination, a fine subtle scale is noted that may appear hypopigmented (Fig. 120-2). Pale yellow or orange fluorescence under Wood’s light is sometimes present. The differential diagnosis includes vitiligo and seborrheic dermatitis. A KOH preparation reveals short hyphae mixed with spores (“chopped spaghetti and meatballs”). Management.: Tinea versicolor may be treated with 2.5% selenium sulfide shampoo, imidazole creams, ketoconazole cream or foam, or oral ketoconazole as a single 400-mg dose or 200 mg daily for 5 to 10 days.6 Fluconazole 150 to 300 mg weekly for 2 to 4 weeks may also be used. Recurrence rates vary from 15 to 50%, and recurrence is considered the rule rather than the exception. Monthly prophylaxis with propylene glycol and water, selenium shampoo, or azole creams can help prevent recurrences. Pigmentation may not return to normal for months. Propylene glycol is inexpensive and effective. Clinical Features.: Tinea unguium results in nails that are opaque, thickened, cracked, and crumbled. Subungual debris is present, and the nail may contain yellowish longitudinal streaks. The nail of the great toe is most commonly involved. Involvement of all of the nails of the hands and feet is rare. Management.: Topical therapy of the nails alone rarely results in a cure because penetration into the nail keratin is poor. Fingernails typically respond more rapidly to therapy than toenails do. Oral griseofulvin and ketoconazole require prolonged courses, with high relapse rates and numerous side effects.7 Newer agents such as itraconazole, fluconazole, and terbinafine are safer and more effective. They also offer shorter treatment periods, thus improving compliance.7 The infection may be resistant to this regimen as well, however, and surgical removal of the nail is occasionally required. The choice of specific agent may be best left to a consultant or patient’s primary physician, given the long course of treatment and frequency of treatment failure. If therapy is started in the ED, reliable follow-up is needed. Griseofulvin ultramicrosize 375 mg twice daily or ketoconazole 400 mg daily is given for 4 to 6 months. Newer agents are preferred by dermatologists: terbinafine 250 mg/day for 6 to 12 weeks (a longer course is given for toenail involvement) is considered first-line therapy. Recurrence is common.8 Clinical Features.: Oral thrush is the most common clinical expression of Candida infection. Thrush is common in newborns, with one third being affected by the first week of life. It appears as patches of white or gray friable material covering an erythematous base on the buccal mucosa, gingiva, tongue, palate, or tonsils. Fissures or crust at the corners of the mouth may be present. The differential diagnosis of oral thrush includes lichen planus (which unlike C. albicans is not easily scraped off). Oral mucous membrane infection with C. albicans is an AIDS-defining illness. If the patient does not use dentures and has not taken antibiotics recently, underlying immunosuppression should be considered. Management.: Treatment of oral thrush involves painting of the mouth with 1 mL to each side of the mouth of oral nystatin suspension (100,000 units/mL) four times a day for infants or 4 to 6 mL four times a day swish and swallow for older children and adults. Treatment is continued for 5 to 7 days after the lesions disappear. A preferable treatment option for adults is clotrimazole troches 10 mg dissolved in the mouth two to five times daily. If topical therapy is not effective or in cases of chronic candidiasis, oral fluconazole 3 mg/kg, 100 to 200 mg/day for 1 to 2 weeks, may be prescribed. If that fails, treatment options include posaconazole suspension, 400 mg twice daily for 3 days, then 400 mg daily for up to 28 days, or itraconazole 200 mg daily for 2 to 4 weeks.9 Painting of the oral cavity with small amounts of gentian violet solution 1% has been used in both children and adults for treatment of refractory oral candidiasis. Caution is needed in infants and small children to ensure that only a minimal amount of the solution is swallowed. Clinical Features.: Cutaneous candidiasis favors the moisture and maceration of the intertriginous areas—the interdigital web spaces, groin, axilla, and intergluteal and inframammary folds. Lesions appear as moist, bright red macules rimmed with a collarette of scale, which represents the pustule roof with scalloped borders. Small satellite papules or pustules are just peripheral to the main body of the rash. These satellite lesions are the most typical indicators of a Candida infection. Intertriginous lesions are prone to bacterial superinfection. Differential Considerations and Diagnostic Strategies.: The differential diagnosis of cutaneous candidiasis includes contact dermatitis, tinea cruris, intertrigo, herpes simplex such as herpetic whitlow, and folliculitis. Candidiasis, however, is less sharply demarcated than tinea cruris and brighter red than intertrigo. A KOH preparation of a specimen taken from a pustule and roof of the lesion will reveal hyphae and pseudohyphae. Management.: Treatment of intertriginous lesions requires the removal of excessive moisture and maceration. Lesions should be exposed to circulating air from a fan several times a day. Inflammatory lesions are either soaked in or covered with compresses of cool water or Burow’s solution. Topical imidazole creams, such as clotrimazole and miconazole, are applied sparingly to affected areas. Prescription creams, such as econazole, ketoconazole, and sulconazole, are also effective. Treatment consists primarily of altering the physical environment in which diaper dermatitis thrives. Advise parents to provide continuous air exposure of the area; if this is not possible, diapers should be changed frequently and topical barrier ointments, such as zinc oxide, applied. Treatment includes nystatin or other topical antifungal creams. If exudative lesions are present, treatment with topical, cool, wet compresses of saline or Burow’s solution is indicated for 2 or 3 days. Severe contact or seborrheic dermatitis may require the addition of a short course of a low-potency topical corticosteroid, such as 1% hydrocortisone in a cream base.10 Particularly severe, recurrent, or not improving diaper rash in infants raises the possibility of an immunodeficiency syndrome, diabetes, or caregiver neglect. Pityriasis rosea is self-limited, resolving in 8 to 12 weeks. Its cause is unknown, although a virus is suspected. The differential diagnosis includes tinea corporis, guttate psoriasis, lichen planus, drug eruption, Lyme disease, and secondary syphilis. Recurrences are rare. Treatment is usually unnecessary, except for symptomatic alleviation of bothersome pruritus. Direct sun exposure or, alternatively, ultraviolet B therapy to severely affected areas has been recommended; the application of moderately potent topical steroids to severely pruritic areas also has its proponents. The benefits of these treatments are questionable,11 and ED interventions are usually limited to simple reassurance and close follow-up. Atopic dermatitis is a common dermatologic condition often referred to as eczema or chronic dermatitis. Atopic dermatitis is the cutaneous manifestation of an atopic state, and although it is not an allergic disorder, it is associated with allergic diseases such as asthma and allergic rhinitis. Patients with atopic dermatitis are known to have abnormalities of both humoral and cell-mediated immunity.12 The exact mechanism is unclear, but eosinophil, mast cell, and lymphocyte activation triggered by increased production of interleukin-4 by specific T helper cells seems to be involved. Increased immunoglobulin E levels are found in most but not all patients with atopic dermatitis, but there is a poor correlation between the severity of the dermatitis and the serum immunoglobulin E level. The course of atopic dermatitis involves remissions and exacerbations. More than 90% of patients have the onset of atopic dermatitis before 5 years of age. New-onset atopic dermatitis in older children or adults should suggest other diagnoses. Atopic dermatitis has no pathognomonic skin lesions or unique laboratory parameters. Diagnostic criteria include itchy skin plus three or more of the following: history of flexural involvement, generalized dry skin, history of asthma or hay fever, onset of rash before 2 years of age, and flexural dermatitis.13 These criteria are sensitive (85%) and specific (96%). Cyclosporine and other immunosuppressant agents are being used with some promising benefit. Further studies are needed to determine ideal dosing and safety profiles for these agents.13 Topical calcineurin inhibitors, including tacrolimus ointment and pimecrolimus cream, are nonsteroidal topical immunosuppressants approved in the United States for use on children 2 years or older; they are useful for treatment of lesions on the thinner skin areas (face, groin, and axillae) where repeated applications of topical corticosteroids may result in skin atrophy or striae.14 A burning sensation at the site of application may occur. Note that the Food and Drug Administration has issued a “black box” warning concerning long-term continuous treatment with topical calcineurin inhibitors and cancer, although there is currently no evidence for a causal link.15 Eczema molluscatum is self-limited. Eczema vaccinatum results from exposure of patients to vaccinia virus either by intentional inoculation or through contact with someone recently immunized against smallpox. Therapy for eczema vaccinatum requires prompt administration of intravenous immune globulin, which can be obtained from the Centers for Disease Control and Prevention.16 Impetigo is a slowly evolving pustular eruption, most common in preschool children. Currently, Staphylococcus aureus is the most common pathogen, with group A streptococcus a distant second.17 Poor health and hygiene, malnutrition, and various antecedent dermatoses, especially atopic dermatitis, predispose individuals to impetigo. Staphylococcal impetigo is differentiated from streptococcal impetigo in that it is more superficial, and there is little surrounding erythema. Other diagnostic considerations are herpes simplex virus (HSV) and inflammatory fungal infections. A Gram stain of the weepy erosion obtained after removal of the crust will reveal gram-positive cocci. MRSA impetigo is increasingly common. Risk factors include prior infection or colonization with MRSA.18 Systemic and topical therapies are equally successful in treating impetigo.17 For more extensive lesions, systemic treatment is recommended. There is no evidence, however, that systemic antibiotics prevent the development of acute glomerulonephritis. The efficacy is similar for topical mupirocin 2% ointment three times a day, oral erythromycin ethylsuccinate 250 mg four times a day for 10 days in adults or 30 mg/kg/day in children, and cephalexin 50 mg/kg/day not exceed 500 mg per dose three times a day for 7 to 10 days.17 Mupirocin is avoided when there is concern about methicillin-resistant strains, and care should be taken that it does not get into the patient’s mouth. Therapy for bullous impetigo consists of an oral penicillinase-resistant semisynthetic penicillin, such as dicloxacillin, 250 mg four times a day for 5 to 7 days for adults, or erythromycin ethylsuccinate, 250 mg four times a day in adults or 30 to 50 mg/kg/day in children. Azithromycin may also be used, dosed at 500 mg on the first day in adults, followed by 250 mg a day for 4 days; in children, it is dosed at 10 mg/kg given on the first day, followed by 5 mg/kg/day for 4 days more. If the infection is limited to a small area, mupirocin 2% ointment three times a day may be used. Without treatment, impetigo generally heals within 3 to 6 weeks.17 Hidradenitis suppurativa affects the apocrine sweat glands. Recurrent abscess formation in the axillae and groin resembles localized furunculosis. The condition tends to be recurrent and may be extremely resistant to therapy. Hidradenitis suppurativa may be treated with drainage of abscesses if they are fluctuant, painful, and large. Antistaphylococcal antibiotics are useful if they are administered early and for a prolonged period. Begin treatment for mild disease with topical clindamycin, 10 mg/mL twice daily, for 3 months. In patients with more severe or nonresponsive disease, begin clindamycin, 300 mg twice daily, combined with rifampin, 300 mg twice daily, for 3 to 6 months.19 Antiandrogen therapy may be considered if antibiotics do not produce improvement. Many cases do not respond, however, and eventually require local excision and skin grafting of the involved area. Sonography will help differentiate abscesses from vascular or lymphoid structures. The incidence of community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) has soared since the first report in 1993. In many major U.S. cities, CA-MRSA is now the most common pathogen cultured from ED patients presenting with skin and soft tissue infections.20 Concern exists that CA-MRSA may be more virulent than methicillin-sensitive strains, and colonization with CA-MRSA may produce more overt infections.20 Hospital-acquired MRSA isolates can survive on a variety of inanimate surfaces, sometimes for weeks. It is unclear whether this is also true for CA-MRSA isolates; if it is true, their presence on such items as clothing, towels, and athletic equipment might contribute to outbreaks. Pets (including dogs and cats), livestock, and birds have been identified as MRSA carriers; their role in MRSA transmission to humans requires further evaluation.21 CA-MRSA infections are most often manifested as skin and soft tissue suppuration, such as an abscess, furuncle, or cellulitis. Lesions frequently exhibit central necrosis and are often confused with spider bites by patients.22 Clinical features cannot distinguish with certainty skin and soft tissue infections caused by MRSA from those caused by methicillin-susceptible S. aureus. Although rare, CA-MRSA infection can also be manifested as necrotizing fasciitis.23 Recurrences of CA-MRSA cellulitis are common. Contagion among the close household contacts of patients as well as correctional facility, school, and sports team contacts is well recognized. Several studies have demonstrated excellent outcomes for abscesses caused by CA-MRSA that are treated with incision and drainage alone.24 If antibiotics are needed, information on local antibiotic resistance patterns can help clinicians assess the likelihood of CA-MRSA infection and guide decisions about empirical treatment. A specimen for culture and susceptibility testing, which was considered to be unnecessary in the pre–CA-MRSA era, may be useful in guiding therapy. Specimens are obtained at the time of incision and drainage of purulent lesions. Clindamycin combines MRSA activity with effectiveness against the majority of other gram-positive organisms. Side effects include diarrhea, Clostridium difficile colitis, and increasing rates of clindamycin resistance.25 Rifamycin has anti-MRSA activity, but resistance readily develops, so it should not be used alone. The advantage of rifamycin is its long half-life, which allows once-a-day administration, and it penetrates well into all tissues and body fluids; its disadvantages include a high potential for drug-drug interactions. Linezolid is active against almost all CA-MRSA isolates and group A streptococci. Disadvantages of its use include high cost, lack of routine availability, hematologic side effects, and potential for resistance among S. aureus strains. Prolonged linezolid administration increases the likelihood of resistance.26 Patients with large abscesses, abscesses in high-risk locations, fever, signs of systemic infection, young age, or immunodeficiency prompt consideration of hospitalization. Vancomycin is still considered the parenteral drug of choice for patients with invasive S. aureus infection, although clinical failures have been reported. It seems reasonable to combine vancomycin with another effective antistaphylococcal agent because many antibiotics have better bactericidal activity. In severely ill patients, carbapenems such as meropenem, panipenem, and ertapenem are recommended because they are active against CA-MRSA and synergistic with vancomycin.27 Use of parenteral clindamycin (not recommended as monotherapy), trimethoprim-sulfamethoxazole, and linezolid has been described. In addition, daptomycin and tigecycline are now approved for the treatment of skin and soft tissue infections caused by MRSA.28 Common antiseptics appear to retain reasonable activity against CA-MRSA, although the results of studies are somewhat conflicting. Good personal hygiene, including appropriate handwashing techniques, separation of infected patients from other types of patients, and routine cleaning of shared equipment, are essential to limiting CA-MRSA spread.29 The arthritis-dermatitis syndrome is the most common presentation of disseminated gonococcal disease. It occurs in 1 or 2% of patients with gonorrhea, affecting women primarily.30 Fever and migratory polyarthralgias commonly accompany the skin lesions. The lesions are often multiple and have a predilection for periarticular regions of the distal extremities. The lesions begin as erythematous or hemorrhagic papules that evolve into pustules and vesicles with an erythematous halo (Fig. 120-3). They closely resemble the lesions of meningococcemia at this stage. They may or may not be tender and may have a gray necrotic or hemorrhagic center. Healing with crust formation usually occurs within 4 or 5 days, although recurrent crops of lesions may appear even after antibiotics have been started.
Dermatologic Presentations
Perspective
LESION
APPEARANCE
Macule
Flat; color differs from surrounding skin
Patch
A macule with surface changes (i.e., scale or wrinkling)
Papule
Elevated skin lesion <0.5 cm in diameter
Plaque
Elevated skin lesion >0.5 cm in diameter; without substantial depth
Nodule
Elevated skin lesion >0.5 cm in diameter and depth
Cyst
Nodule filled with expressible material
Vesicle
Blisters <0.5 cm in diameter filled with clear fluid
Bullae
Blisters >0.5 cm in diameter filled with clear fluid
Pustule
Vesicle filled with cloudy or purulent fluid
Crust
Liquid debris that has dried on the skin surface; usually moist and yellowish brown
Scale
Visibly thickened stratum corneum; usually white
Lichenification
Epidermal thickening characterized by visible and palpable skin thickening and accentuated skin markings
Induration
Dermal thickening that feels thick and firm
Wheal
Papule or plaque of dermal edema; often with central pallor and irregular borders
Erythema
Red appearance of skin caused by vasodilation of dermal blood vessels; blanchable
Purpura
Red appearance of skin caused by blood extravasated from disrupted dermal blood vessels; nonblanchable
Macular purpura
Flat, nonpalpable
Papular purpura
Elevated, palpable
Scales, Plaques, and Patches
Principles of Disease
Tinea Capitis
Tinea Corporis
Tinea Pedis
Tinea Versicolor
Tinea Unguium (Onychomycosis)
Candidiasis
Oral Thrush
Cutaneous Candidiasis
Diaper Dermatitis
Management
Scaly Papules
Pityriasis Rosea
Atopic Dermatitis
Clinical Features
Management
Skin Infections in Patients with Atopic Dermatitis
Pustules
Principles of Disease
Clinical Features
Management
Hidradenitis Suppurativa
Community-Associated Methicillin-Resistant Staphylococcus aureus
Clinical Features
Management
Prevention
Gonococcal Dermatitis
< div class='tao-gold-member'>

Full access? Get Clinical Tree


Dermatologic Presentations
Only gold members can continue reading. Log In or Register to continue







