Chapter 8 Definition and Incidence of the Difficult Airway
I Introduction
The fundamental responsibility of an anesthesiologist is to ensure adequate gas exchange for the patient. Failure to maintain oxygenation for more than a few minutes can result in catastrophic anoxic injury. Data from closed claims of respiratory-related malpractice in 1990 reported brain damage or death in more than 85% of patients.1 In the closed claims data from 2006, improvements in airway management techniques and monitoring standards had reduced the number of intubation-related claims,2 but difficulties with airway management during emergence remained among the leading causes of serious perioperative problems. It has been estimated that the inability to successfully manage a difficult airway (DA) is responsible for as many as 30% of deaths directly attributable to anesthesia.2
II Definition and Classification of the Difficult Airway
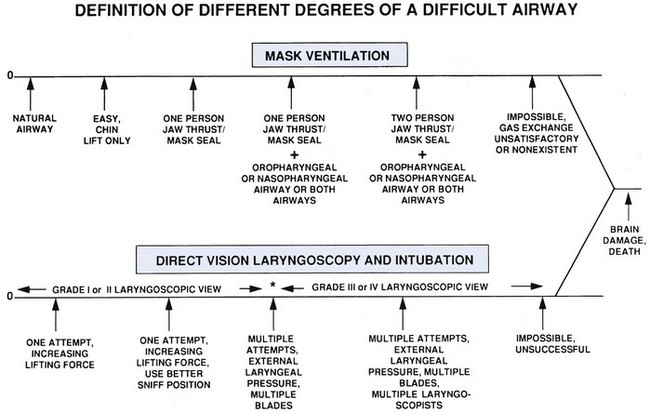
The term difficult airway spans a spectrum of clinical situations (Fig. 8-1), from difficulty or inability to provide mask ventilation to difficulty or inability to intubate the trachea. The combined “cannot intubate, cannot ventilate” (CICV) scenario carries the highest risk of brain damage or death. To better describe the layers of difficulty, we have chosen several categories of difficult or impossible mask ventilation; difficult placement of, or ventilation via an SGA; difficult laryngoscopy; and difficult intubation using direct laryngoscopy, video laryngoscopy, or flexible bronchoscopy.
A Difficult or Impossible Face Mask Ventilation
2 Definition of Difficult Mask Ventilation
The simplest mask ventilation scale in contemporary literature was described by Han and colleagues in 2004 (Table 8-1).3 In that scale, the progressive grades of difficulty are (1) ventilation by mask; (2) ventilation by mask with oral airway or other adjuvant with or without muscle relaxant; (3) difficult mask ventilation, defined as “inadequate, unstable, or requires two providers” with or without muscle relaxant; and (4) impossible mask ventilation with an inability to mask ventilate with or without muscle relaxant.
TABLE 8-1 Han Mask Ventilation Scale and Incidence of Difficult Mask Ventilation
| Grade | Description | Incidence (n, [%]) |
|---|---|---|
| 1 | Ventilated by mask | 37,857 (71.3%) |
| 2 | Ventilated by mask with oral airway or other adjuvant with or without muscle relaxant | 13,966 (26.3%) |
| 3 | Difficult ventilation (inadequate, unstable, or requiring two providers) with or without muscle relaxant | 1,141 (2.2%) |
| 4 | Unable to mask ventilate with or without muscle relaxant | 77 (0.15%) |
From Han R, Tremper KK, Kheterpal S, O’Reilly M: Grading scale for mask ventilation. Anesthesiology 101:267, 2004.
Langeron and colleagues defined difficult face mask ventilation as “the inability of an unassisted anesthesiologist to maintain oxygen saturation >92%, as measured by pulse oximetry, or to prevent or reverse signs of inadequate ventilation during positive-pressure mask ventilation under general anesthesia.”4 In their study, mask ventilation was considered difficult if one or more of six criteria were present:
1. Inability for the unassisted anesthesiologist to maintain oxygen saturation >92% using 100% oxygen and positive-pressure mask ventilation
2. Important gas flow leak by the face mask
3. Need to increase gas flow to >15 L/min and to use the oxygen flush valve more than twice
4. No perceptible chest movement
5. Need to perform a two-handed mask ventilation technique
El-Ganzouri and coworkers defined difficult mask ventilation as the “inability to obtain chest excursion sufficient to maintain a clinically acceptable capnogram waveform despite optimal head and neck positioning and use of muscle paralysis, use of an oral airway, and optimal application of a face mask by anesthesia personnel.”5
3 Incidence of Difficult Mask Ventilation
Two studies by Kheterpal and associates on difficult and impossible mask ventilation represent the largest investigations to date on the topic. The incidence of difficult mask ventilation was 1.4% in 22,660 patients and 2.2% in a subsequent study of 50,000 patients.6,7 The incidence of impossible ventilation ranged from 0.15% to 0.16% in these two large studies. Langeron and colleagues reported a 5% incidence of difficult mask ventilation, with 1 of every 1502 patients impossible to ventilate with a face mask (0.07%).4 In other large, prospective studies the incidence has ranged from 0.07% to 1.4%,5,8,9 although this was not the primary outcome being assessed. In summary, difficult mask ventilation can be expected 1 or 2 times in every 100 anesthesias, and impossible mask ventilation 1 or 2 times in 1000 anesthesias.
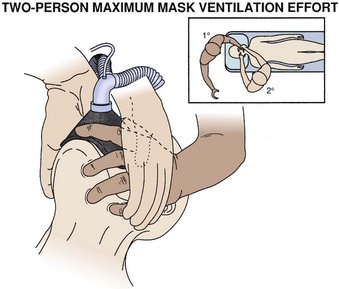
Methods used to improve airway patency include the head-tilt, jaw-thrust, and chin-lift maneuvers as well as insertion of oral or nasal airways. If mask seal is poor, the practitioner may choose a different face mask, use a two-hand or two-person technique, insert bolsters between the alveolar ridge and the cheeks, or employ other methods to improve the interface between the face and the mask. When two persons are needed, ideally the primary anesthesiologist stands at the patient’s head and initiates jaw thrust with the left hand at the angle of the left mandible and left-sided mask seal while the right hand compresses the reservoir bag. The standard position for the primary anesthesiologist appears in Figure 8-2. The secondary (helping) person stands at the patient’s side, at the level of the patient’s shoulder, facing the primary anesthesiologist. The right hand of the secondary anesthesiologist should cover the left hand of the primary anesthesiologist and contribute to left-sided jaw thrust and mask seal, and the left hand of the secondary person initiates right-sided jaw thrust and mask seal. In this way, all four hands are doing something important without interfering with one another, and there is almost no redundant effort. With this positioning, the secondary person can watch the monitors continuously, manipulate the larynx externally, and hand equipment to the primary anesthesiologist.
B Difficulties with Supraglottic Airway Devices
The last two decades have seen a phenomenal increase in the use of SGAs for elective and rescue purposes. Most studies of SGA devices describe first-attempt and overall success rates. Difficulties with the devices include failure of insertion, failure to form a clear passage to the trachea, and failure to form an effective seal in the airway.10
Most of the studies reporting difficulties with SGAs have focused on LMAs. Among these, the failure rate is 1% for the intubating and ProSeal models and 2% for the LMA classic and flexible models.10
2 Incidence of Success
For the ProSeal laryngeal mask airway (PLMA), first-attempt success rates range from 76% to 100% (mean, 87.3%), and overall insertion success rates range from 90% to 100% (mean, 98.4%).11 One of the important rescue functions of the LMA is as a conduit for flexible bronchoscopic intubation. The inability to visualize vocal cords using a trans-LMA flexible bronchoscopic technique is a significant impediment to successful tracheal intubation. The incidence of difficult laryngeal visualization ranges from 0% to 26% with the PLMA.11 Although it is possible that success rates with other SGA devices may differ, the inherent variability in success is an important learning point. Early recognition of unsuccessful placement and institution of alternative airway plans are essential to prevent morbidity from failure of an SGA device.
C Difficult Direct Laryngoscopy
1 Laryngeal Visualization
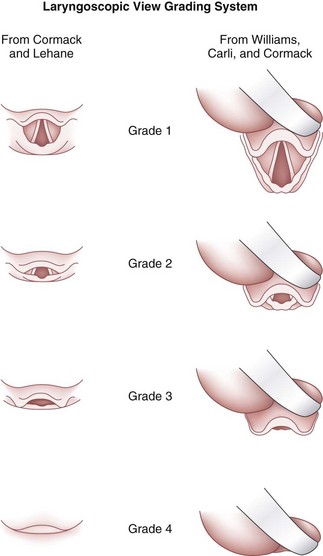
The appearance of the laryngeal inlet on direct laryngoscopy is best described by the Cormack and Lehane grade of laryngeal view.12 Difficult laryngoscopy is most commonly defined as presence of a grade 3 or 4 view on laryngoscopy.6,7 Several maneuvers have been shown to improve the laryngeal view on laryngoscopy, but in general, poorer laryngeal views contribute progressively to greater difficulty in achieving successful tracheal intubation (Fig. 8- 3).12–14 As the view worsens, increasing the anterior lifting force with the laryngoscope blade, reinstituting the optimal sniff position, making multiple attempts, manipulating the larynx externally (see Chapter 17 and Fig. 17-10), or opting for alternative devices or laryngoscopists may be required to achieve intubation.

Full access? Get Clinical Tree