Technique
Advantages
Disadvantages
PTGBD
Relatively easy
External drain in place
High technical success rate
Possible dislodgement of drain
Reliably effective
Relative contraindication in liver disease, coagulopathy, ascites
Access to the gallbladder maintained
PTGBA
Relatively easy
Relative contraindication in liver disease, coagulopathy, ascites
No external drain in place
ENGBD
Not limited by liver disease, coagulopathy, ascites
Technical success rate is low
Physiological bile flow
External drain in place
Access to the gallbladder maintained
Possible dislodgement of drain
Post-ERCP pancreatitis
Some cases inaccessible
Endoscopic transpapillary gallbladder stenting
Not limited by liver disease, coagulopathy, or ascites
Technical success rate is low
Possible stent clogging
Physiological bile flow
Post-ERCP pancreatitis
No external drain in place
Some cases inaccessible
EUS-guided transmural nasogallbladder drainage
Not limited by liver disease, coagulopathy, or ascites
External drain in place
Possible dislodgement of drain
Access to the gallbladder maintained
Possible bile peritonitis
No post-ERCP pancreatitis
EUS-guided transmural gallbladder stenting
Not limited by liver disease, Coagulopathy, or ascites
Possible stent clogging
No post-ERCP pancreatitis
Possible bile peritonitis
No external drain in place
Percutaneous Transhepatic Gallbladder Drainage
PTGBD is the most common method for nonoperative gallbladder drainage. The procedure is an interventional radiologic procedure designed to decompress the acutely inflamed gallbladder. Its use has been described in both high-risk surgical patients unresponsive to medical therapy and as first line treatment to delay cholecystectomy [7–9].
Various methods have been described for PTGBD, but the most common is ultrasound-guided transhepatic gallbladder puncture. This procedure is accomplished with minimal anesthesia and generally an 18-gauge needle for drainage. Gallbladder puncture is performed under direct ultrasound guidance to avoid injury to adjacent structures. A 6- to 10-Fr pigtail catheter is then placed in the gallbladder, using a guidewire under fluoroscopy (Seldinger technique) (Fig. 12.1) [6]. Technical and clinical response rates to PTGBD have been reported between 56 and 94 % [9–11], with consistently higher success being documented in more recent studies. The primary advantage of PTGBD in high-risk surgical patients is the avoidance of general anesthesia and those associated cardiovascular risks. That being said, up to 16 % of patients experience complications, including bile peritonitis, bleeding, catheter dislodgement and pneumothorax. In addition, PTGBD may be inappropriate for patients with massive ascites or coagulopathy, and patient discomfort from the catheter has been postulated to decrease quality of life [7, 8, 12, 13].
Fig. 12.1
Percutaneous transhepatic gallbladder drainage (PTGBD) technique. Figures from Tsuyuguchi et al. [27]
There are no randomized controlled trials that directly compare the outcomes of PTGBD to LC [10] although the morbidity [1, 2, 10, 14], mortality [2, 10, 14] among high-risk surgical patients undergoing LC is well documented. Success rates for PTGBD are fairly high, and the mortality related to the procedure (0.36 %) is fairly low, but the overall mortality rate following PTGBD (15.4 %) appears equal to or higher than that for emergency LC (4.5 %) [10]. However, the limitations of the literature preclude absolute conclusions to be made regarding the comparative advantages of this procedure.
There are two randomized controlled trials comparing PTGBD with conservative management. In 2002, Hatzidakis et al. found no difference in resolution of symptoms or overall mortality when comparing PTGBD to nonoperative management in high-risk surgical patients. These authors concluded that the nonoperative treatment should be attempted first, and PTGBD should be reserved for those unresponsive to initial medical management [8]. In a later study, Akyürek et al. compared PTGBD with early LC to medical management with delayed LC in high-risk surgical patients [7]. While the conversion to open cholecystectomy and complication rates were similar in both groups, the study did show a shorter hospital stay and lower overall cost in the group treated with PTGBD and early LC. Thus the authors advocate for percutaneous drainage in high-risk surgical patients over medical management [7].
As previously stated, there is no randomized controlled trial comparing PTGBD to emergency LC in high-risk patients. With the advances in surgical laparoscopic training, intensive care management and perioperative anesthesia, the outcomes of PTGBD and LC may be more similar than one thinks. To this end, the CHOCOLATE trial is an ongoing randomized controlled trial comparing morbidity and mortality between LC and PTGBD in high-risk surgical patients [15].
Percutaneous Transhepatic Gallbladder Aspiration
Percutaneous transhepatic gallbladder aspiration is a method to aspirate the gallbladder with a small-gauge needle under ultrasonographic guidance (Fig. 12.2) [6]. It is an easy, low-cost, bedside-applicable procedure, without the patient discomfort seen with an indwelling catheter (PTGBD).
Fig. 12.2
Percutaneous transhepatic gallbladder aspiration (PTGBA) technique. Figures from Tsuyuguchi et al. [27]
Fundamentally, PTGBA should not work in the setting of infection by the principle of all infections needing continuous drainage. However, infection is not the inciting factor in AC, with obstruction of the cystic duct causing increased intraluminal pressure, leading to venous congestion, compromised blood supply and impaired lymphatic drainage. The mucosa becomes ischemic and releases inflammatory mediators causing trauma, edema, ulcers and possible wall necrosis. Secondary bacterial infection can then occur from the initial obstruction and activation of the inflammatory cascade. Secondary infections complicate up to 50 % of clinical courses, as 40–50 % of cases have been shown to have positive bile cultures [16].
This idea corresponds to Chopra et al., who documented a lower clinical response rate to PTGBA in patients with positive bile cultures [17]. Since infection may not always be present, continuous drainage could be considered excessive treatment in some patients. One time aspiration of bile from the obstructed gallbladder removes the irritant luminal contents and reduces the intraluminal pressure, thereby providing relief prior to the onset of infection. Further studies have concomitantly used antibiotic irrigation during aspiration to counteract any infection that may be present; however, the effectiveness of this technique is unclear due to limited data [18]. In comparing PTGBA to PTGBD, Chopra et al. argues that PTGBA should be the procedure of initial choice as the technical (97–100 % [17, 18]) and clinical (71–77 % [17, 18]) response rates are remarkably high, thus PTGBD should be saved as a salvage procedure for those failing to respond to a single PTGBA. Using this method, 77 % of patients in this study avoided PTGBD [17]. Tsutsui et al. advocate for repetitive PTGBA in patients that fail to initially improve, arguing that the vast majority of patients will respond within two PTGBAs, avoiding placement of an indwelling catheter [18].
The incidence of adverse events for PTGBA is lower (0–4 %) than in PTGBD, and no serious adverse events have been reported [19]. Instances may exist when PTFBD is favorable to gallbladder aspiration. These situations include patients with thick bile or pus that is difficult to aspirate or patients with a large amount of bile that requires continuous drainage for infection source control. In such patients, PTGBD has a greater chance of success because of the larger caliber of the catheter and the potential for repeated irrigation. Also, because it does not provide continuous drainage, PTGBA is inappropriate in patients in whom the indication for gallbladder drainage is to provide relief from a distal biliary obstruction, such as in biliary malignancies [17].
Despite its potential advantages, PTGBA has not been widely adopted as a standard treatment modality because AC is commonly thought to require continuous drainage and the data supportive of PTGBA is limited to case series and retrospective reviews.
Endoscopic Transpapillary Gallbladder Drainage and Stenting (ENGBD and ENGBS)
ENGBD involves placement of a nasobiliary drainage tube and generally does not require biliary sphincterotomy. After successful bile duct cannulation, a guidewire is advanced into the cystic duct and subsequently into the gallbladder. A 5–8.5Fr pigtail nasobiliary drainage tube catheter is then placed into the gallbladder (Fig. 12.3) [6]. It has been reported in patients with specific comorbidities, including end-stage liver disease or coagulopathy where transhepatic techniques are contraindicated.
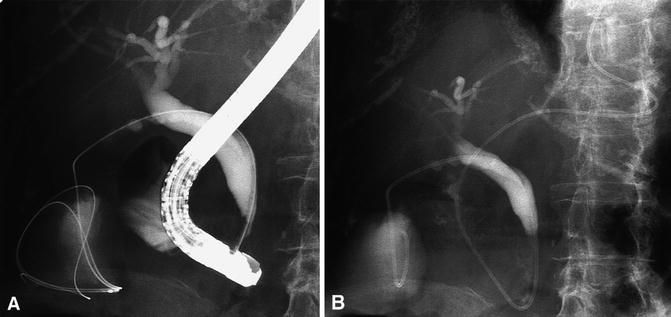
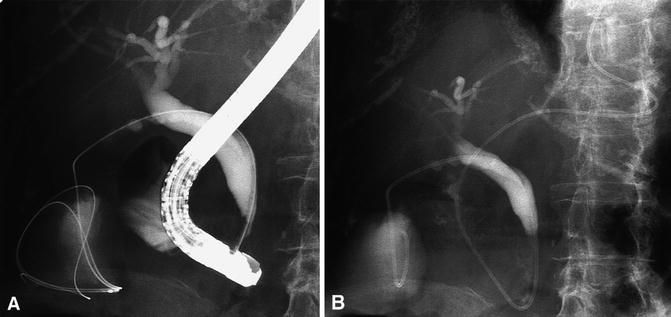
Fig. 12.3
Endoscopic transpapillary gallbladder drainage (ENGBD) technique. Figures from Itoi et al. [28]
In ENGBS, the procedure is identical to ENGBD, but a 6–10-Fr diameter double-pigtail stent is placed instead of a nasobiliary drainage tube (Fig. 12.4) [6]. When larger diameter stents are placed (i.e., 10F), a sphincterotomy is performed to prevent post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis [19]. Also, unlike ENGBD, stents cannot be irrigated to prevent occlusion by blood or debris, which is a potential cause for concern over time [19].
Fig. 12.4
Endoscopic transpapillary gallbladder stenting (ENGBS) technique. Figures from Tsuyuguchi et al. [6]
While supportive data are limited, a meta-analysis of ENGBD and ENGBS by Itoi et al. demonstrated a technical success rate of 81 % and 96 % and a clinical response rate of 75 % and 88 % respectively [19]. These early results are comparable to the success rates of the more established approaches of PTGBD and PTGBA [19]. This meta-analysis also found the incidence of adverse events to be similar to that of PTGBD (0–16 %). It is important to note that LC can be performed following resolution of the acute inflammation and sepsis. The tube or stent can then be removed preoperatively or intraoperatively when the time comes [19].
Both ENGBD and ENGBS require difficult endoscopic techniques and only case series have been conducted at a limited number of institutions [6]. Both methods have not yet been established as a standard of care. Therefore, while results are promising, these are newer options for a specific patient population, and should currently only be performed in high-volume institutes by skilled endoscopists [6].
Endoscopic Ultrasound-Guided Transmural Gallbladder Drainage (EUS-GBD)
Although endoscopic ultrasound (EUS)-guided drainage procedures have been safely used with peripancreatic fluids, including those from pancreatic pseudocysts and pancreatic, subphrenic and splenic abscess, little is known regarding EUS-guided transmural gallbladder drainage (GBD) for high-risk patients with AC [20].

Full access? Get Clinical Tree








