Critical care ultrasound (CCUS) is an extension of the physical examination. The front-line clinician performs, interprets, and applies goal-directed examinations to rapidly diagnose and manage life-threatening conditions, including acute respiratory failure and undifferentiated shock. The American College of Chest Physicians/La Société de Ré animation de Langue Francaise Statement on Competence in Critical Care Ultrasonography (ACCP/SRLF Statement) highlights five areas of focus for intensivists: cardiac, thoracic (consisting of both the lungs and the pleura), vascular (consisting of both diagnostic and vascular access), and abdominal ultrasound.1 CCUS examinations are not comprehensive examinations that evaluate all anatomic structures and measurements of an organ or body region.
This chapter serves as a brief overview of the most common uses of CCUS. In no way is it meant to be completely comprehensive; however, it serves as an adequate introductory tool and covers the material most frequently tested on the American Board of Internal Medicine Pulmonary and Critical Care board examinations.
It is imperative to have an easily accessible and portable machine that allows for rapid and repeated use. Machines ideally should have a high-frequency vascular probe (Fig. 31-1A) and low-frequency phased array probe (Fig. 31-1B). Appropriate manufacturer warranty and technical support should be included in the purchase because of heavy use and the high likelihood for maintenance.
FIGURE 31-1
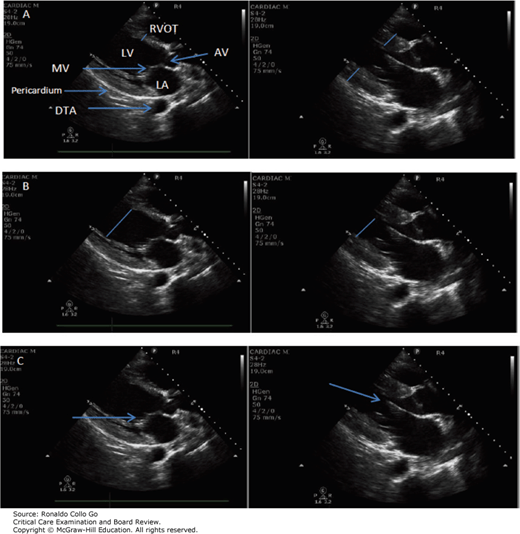
(A) Note the difference in length of blue lines in diastole and systole indicating the change in thickness of myocardial wall of the interventricular septum. Arrow points to the descending thoracic aorta. (B) Note the difference in LV cavity size in systole and diastole. (C) Note the close approximation of the anterior leaflet of mitral valve to the interventricular septum (arrow). AV, aortic valve; DTA, descending thoracic aorta; LA, left atrium; LV, left ventricle; MV, mitral valve; RVOT, right ventricular outflow tract.
It is imperative to develop a consistent approach when obtaining, describing, and interpreting ultrasound images. If possible, the operator should always be positioned immediately down- or upstream (adjacent) to the system console, allowing for ease of image acquisition and manipulation. When appropriate (if possible), patient position should be optimized for the current examination (eg, when possible, goal-directed echocardiography GDE should be performed with the patient in the left lateral decubitus position).
Operators should familiarize themselves with the various functions of the ultrasound interface. For basic CCUS, one must master the functions that manipulate image position (depth) and brightness (gain). Depth should be adjusted so that the structure of interest (eg, the heart) occupies the center of the screen. Gain can be increased or decreased to make structures brighter or darker, respectively. Machines often have near, far, and full screen gain adjustment.
Operators should hold the ultrasound probe similar to how they hold a pen, allowing the base of the hand to rest on the patient to provide added stability. The probe indicator should always be uniform for various examinations (eg, for lung or pleural ultrasound, the indicator should always be cephalad, with vascular diagnostics and access to the patient’s left). Operators should slide the probe across the surface of interest (eg, thorax) either medial lateral or cephalocaudal to obtain the appropriate window for the structure being examined (eg, lung). Rotating the probe clock or counterclockwise, fanning medial lateral, or angling the probe toward or away from the indicator all allow for optimizing or adjusting a scanning plane. These maneuvers are best appreciated with hands-on training.
Basic critical care echocardiography is a qualitative “eyeball” assessment of global cardiac function done in a systematic fashion to answer a particular question. A goal-directed echocardiogram consists of five views: parasternal long-axis (PSLA), midventricular parasternal short-axis (PSSA), apical four-chamber (A4C), subcostal long-axis (SCLA), and longitudinal inferior vena cava (IVC).1 It has been shown that with focused training, these combined views performed in a goal-directed fashion can differentiate a critically ill patient’s shock state, including hypovolemic, obstructive, vasodilatory, or cardiogenic shock.2
The PSLA (Fig. 31-1) is obtained by placing the probe in an intercostal space (second to fifth depending on patient anatomy) immediately adjacent to the left side of sternum and rotating the probe indicator toward the patient’s right shoulder (10 o’clock position). Left ventricular function (LVF) is assessed looking for myocardial thickening, endocardial excursion, and anterior mitral valve leaflet excursion (Table 31-1). The presence of a pericardial effusion is assessed by observing fluid tracking anterior to the descending thoracic aorta (DTA). Aortic and mitral valve catastrophe can be assessed in the PSLA by applying two-dimensional color. An on-axis image will show the right ventricular outflow tract (RVOT), aortic valve (AV), and left atrium all midline, and the left ventricle (LV) apex should be just out of the image window.
| Ultrasound findings | Left Ventricular Function |
|---|---|
| Myocardial thickening A | Increase in heart muscle wall thickness; Normal values varies per age and sex |
| Endocardial excursion B | LV cavity shrinking by > 40% |
| Mitral valve excursion C | Approximation of MV < 1 cm to the interventricular septum (no presence of severe mitral/aortic valvular regurgitation) |
The PSSA (Fig. 31-2) is obtained by rotating the probe indicator 90 degrees clockwise from the PSLA to face the patient’s left shoulder (2 o’clock position). The operator should fan the probe until the LV is visualized at the midventricular–papillary muscle level. LVF, right ventricle (RV) and LV septum kinetics, pericardial effusions, and regional wall motion abnormalities can all be assessed in the PSSA. An on-axis image will show a circular left ventricular cavity (as opposed to off-axis, yielding an oval-shaped LV) and small crescentic shaped RV at the LV anteroseptal wall.
The A4C view (Fig. 31-3) is obtained by sliding the probe slightly inferolateral to the nipple line. (In women, the probe must be positioned under the breast tissue.) The orientation marker should be rotated perpendicular to the patient’s left shoulder (3 o’clock position). If a patient can safely be turned to the left lateral decubitus position, this often yields a higher quality image. An on-axis view elongates the heart into a “football” shape compared with a foreshortened “basketball” shape, leading to gross overassessments of RV and LV size. To correct an off-axis “basketball” shape, the operator often must slide the probe one intercostal space caudad. The A4C view allows comparison of the RV-to-LV ratio to assess for shock caused by acute cor pulmonale. LVF can be underestimated in this view because of difficulty in assessing myocardial thickness and endocardial excursion.
The SCLA view (Fig. 31-4) is obtained by laying the probe flat on the patient’s abdomen just inferior to the xiphoid process with the indicator rotated to the 3 o’clock position. The liver edge is the most anterior structure and is used as an acoustic window. The SCLA view is sometimes the only view obtainable because of barriers in critically ill patients such as chest wall drains, dressings, obesity, or increased air artifact caused by chronic lung disease and use of mechanical ventilation. The SCLA view can be used to assess for shock caused by pericardial effusion in the clinical context of cardiac tamponade, LVF, and RV-to-LV ratio and for cardiac standstill during advanced cardiac life support.
FIGURE 31-4
Subcostal long axis. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.


Full access? Get Clinical Tree








