94 Critical Care Nutrition
Less than ideal NT is unfortunately provided to a significant proportion of ICU patients. A recent evaluation of nutrition practices in 158 ICUs across 20 countries by Cahill et al.1 reported significant deficits in meeting caloric and protein goals and adhering to the provision of specialized nutrition. For example, delivery of protein goals was only achieved 60.3% of the time.
 Gut Use and Differential Response to Feeding and Starvation
Gut Use and Differential Response to Feeding and Starvation
Lack of adequate food intake is a frequent problem in the ICU. Diseases are frequently associated with significant anorexia and/or inability to eat. Surgical procedures and diagnostic tests often demand an empty stomach. A nil per os (NPO) order is too easily written even in the absence of a logical reason to do it. Despite physiologic differences between starvation in a healthy individual and lack of adequate intake during illness, it is essential to study starvation as an important aspect of nutritional care in the critically ill patient. The functional and structural integrity of the GI tract is affected by whether the gut is used and the patient receives enteral feeding. Animal and human studies suggest that enteral feeding maintains mucosal mass, stimulates cellular proliferation and production of brush-border enzymes, and maintains villus height.2–4 Enteral nutrients maintain the integrity of tight junctions between intestinal epithelial cells, stimulate blood flow to the gut, and promote release of a variety of endogenous agents such as cholecystokinin, gastrin, bombesin, and bile salts—substances with trophic effects on intestinal epithelium. Bombesin, for example, can reverse all the histologic and functional deficits caused by parenteral feeding,5 and gastrin and cholecystokinin can encourage partial recovery of gut-associated lymphoid tissue after the use of parenteral nutrition (PN).6 Secretory immunoglobulin A (sIgA) and the production of bile salts help coat bacteria within the GI tract, preventing adherence. Along with the production of mucus and good GI contractility, this helps wash away bacteria in a caudad direction.3 These mechanisms, together with antimicrobial secretions such as pancreatic enzymes, proteases, and lactoferrin help keep the total number of bacteria in check. The normal predominant anaerobic flora of the gut is maintained, preventing overgrowth of more pathogenic organisms such as Enterobacteriaceae, a process referred to as colonization resistance.7
Gut disuse, with or without PN, can lead to deterioration of the functional and structural integrity of the gut. In animals, gut disuse is associated with a marked reduction in villus height, cellular proliferation, mucosal mass, and brush-border enzymes. Intestinal changes caused by starvation in humans are less pronounced than in rodents, but whereas gut disuse may result in a 40% decrease of mucosal mass in rats, the decrease in humans still appears to be about 10% to 15%.2 In humans, loss of villus height in response to pancreatitis is diminished by enteral feeding.4 Villus atrophy is perpetuated in a time-dependent fashion with parenteral feeding.3 Starvation alone may be insufficient to increase gut permeability, but injury followed by starvation increases mucosal permeability proportional to the severity of disease.3,8 Increased permeability is prevented through early feeding, and in burns inversely correlates with the amount of enteral feeding delivered.9 Increases in gut permeability are associated with systemic endotoxemia in humans.8,10 Among burn patients, infection is associated with increased gut mucosal permeability.9 Increases in gut permeability in critically ill patients correlate with the development of organ dysfunction.11
Lack of feeding in animals results in bacterial overgrowth and loss of mucosal defenses against bacterial invasion.7,12 Reduced peristalsis (ileus) can contribute to bacterial overgrowth. Reduced secretions of bile salts and sIgA promote bacterial adherence to the mucosa. Bacterial translocation, a process whereby bacteria transgress the mucosal barrier, is associated with aerobic bacterial overgrowth and decreased intestinal sIgA levels.3 Recent animal studies suggest that these gut-derived factors can reach the systemic circulation via the lymphatic system rather than via the portal bloodstream and thereby cause distant organ injury.13 Thus, animal models suggest that bacterial overgrowth in the lumen leads to bacterial translocation, potentially being a portal for development of sepsis and organ failure.
The significance of bacterial translocation in humans as a cause of systemic illness is still unclear.14,15 Translocation of bacterial products such as endotoxin may also occur. Endotoxin itself, when infused in even small doses in normal volunteers, increases gut mucosal permeability.7 The intestinal secretion of sIgA is diminished within 5 days of gut disuse, with or without PN.5,16 Respiratory tract secretion of IgA may be diminished even sooner. Reduction in the mucosal mass of gut-associated lymphoid tissue and decreased sIgA production increase susceptibility to infections normally controlled by IgA-mediated defenses in experimental animals.17 In mice, as little as 5 days of gut disuse with PN results in loss of protection against respiratory viral infection and reduces clearance of the virus.18 Refeeding with enteral nutrients restores antiviral defenses. Established antiviral mucosal immunity is lost when the GI tract is not stimulated by enteral feeding.17
Dendritic macrophages act as antigen-presenting cells that release cytokines and activate naive CD4+ helper T cells (TH0).19 Secretion of interleukin (IL)-12 stimulates the naive cells to differentiate into T helper 1 (TH1) lymphocytes, favoring a proinflammatory response and release of other proinflammatory cytokines such as IL-2, interferon gamma (IFN-γ), and tumor necrosis factor (TNF). TH1 responses are associated with increased inflammation and are essential for host defenses against infection. Uncontrolled TH1 responses, however, can result in self-injury. Production of IL-4 also stimulates differentiation of TH0 into TH2 lymphocytes,19 leading to secretion of additional IL-4, IL-6, and IL-10. The TH2 response tends to curb or check the TH1 inflammatory response. TH2 responses are essential to prevent self-injury caused by inflammation. However, excessive regulation of inflammatory responses by TH2 cytokines can lead to immune suppression.19
Gut disuse, with or without PN, alters the balance of these lymphocyte populations and the profile of associated cytokines. In animals, gut disuse with PN for 5 days decreases IL-4 and IL-10 secretion and markedly reduces sIgA levels.17 In human babies, use of PN reduces sIgA in intestinal immunocytes.20 IFN-β, IL-5, and IL-6 production by TH1 lymphocytes is not affected by gut disuse and PN.21 Thus, the absence of enteral nutrition (EN) can unbalance the ratio of proinflammatory to antiinflammatory responses.
Gut disuse affects expression of adhesion molecules required for proper homing by naive B cells to the intestinal lamina propria and gut-associated lymphoid tissue. MADCAM-1 is the primary ligand required for the proper homing of B cells, and decreased expression of this molecule interferes with the normal migration of B cells from the vascular space into the lamina propria, leading to atrophy of Peyer’s patches. In animals, there is a 60% decrease in MADCAM-1 expression within 4 days of initiating PN.17 Within 3 days of starting PN, the number of T and B cells in the lamina propria and Peyer’s patches decreases by about 50%.3 In this model, secretion of the TH1 cytokine, IFN-γ, is unchanged, but secretion of the TH2 cytokines, IL-4 and IL-10, decreases. Decreased production of IL-4 and IL-10 leads to increased expression of the adhesion molecules, ICAM-1 and E-selectin, in both the intestinal and pulmonary microvasculature. Increased E-selectin expression on endothelial cells in the pulmonary microvasculature promotes sequestration and extravasation of polymorphonuclear neutrophils.22–24 As a result, any subsequent injury (e.g., ischemia-reperfusion) can promote accumulation of polymorphonuclear neutrophils in the lungs, exacerbating organ injury and even increasing mortality.25,26 Abundant data demonstrate that gut disuse through starvation, either caused by disease or through ill-advised physician orders or neglect, is a real problem that contributes to development of systemic infections, a systemic inflammatory response, and development of multiple organ failure.
EN, particularly if started early, prevents the ill effects of starvation. Normal enteral feeding stimulates proliferation of TH2 CD4+ helper T lymphocytes and the production and release of IgA-stimulating cytokines including IL-4, IL-5, IL-6, IL-10, and IL-13.27 This process is normally counterbalanced by proliferation of TH1 CD4+ helper T lymphocytes and IgA-inhibitory cytokines including IFN-β, TNF, and IL-2. IL-4 stimulates naive CD4+ helper T lymphocytes to convert to IgA-positive B cells in Peyer’s patches. IL-10, IL-5, and IL-6 stimulate the differentiation of IgA-positive B cells into sIgA-secreting plasma cells in the lamina propria.17
Approximately 1 ton of food passes through the intestinal tract of an adult human every year.20 About 1/100,000 of this intake represents intact immunologic antigen.20 Oral tolerance refers to the process whereby the immune response is down-regulated to prevent excessive responses to common antigens found in food and in the commensal bacterial flora of the GI tract. During the induction of oral tolerance, an alternative pathway for CD4+ helper T-cell activation leads to proliferation of special regulatory T cells (TH3 and Tr1) which produce the counter-regulatory cytokines, IL-10 and transforming growth factor beta (TGF-β).20 The stimulation and proliferation of TH3 cells induced by enteral feeding therefore promotes expression of a balanced TH2/TH1 profile. The large dietary and indigenous microbial antigenic load is extremely important for maintaining normal mucosal immunity.20 Antigenic constituents of food clearly exert a stimulatory effect on the intestinal B-cell system, helping to explain why enteral feeding supports a high density of IgA-secreting immunocytes within the intestinal lamina propria. Continued enteral feeding, as well as maintenance of the indigenous microbial flora in the gut, may help keep a balance between the TH1 and TH2 profile and prevent an exaggerated TH1 inflammatory response.
The importance of EN for modulating the inflammatory response was illustrated by a classic study of human volunteers challenged with a small dose of Escherichia coli lipopolysaccharide (endotoxin).28 One group of subjects was maintained for 1 week without feeding and received PN, whereas another group was fed enterally during the same period. After 7 days of either PN or EN, both groups were challenged with lipopolysaccharide. The subjects in the PN group had an exaggerated response to the proinflammatory stimulus, manifested by higher circulating levels of cortisol and TNF, among other findings. Similarly, following injury or an inflammatory disease process, early enteral feeding can blunt the hypermetabolic response.29,30 Among patients with acute pancreatitis, those fed enterally rather than parenterally had significantly lower circulating levels of C-reactive protein, less evidence of oxidative stress, faster resolution of systemic inflammatory response syndrome (SIRS), and a greater decrease in their Acute Physiology and Chronic Health Evaluation (APACHE) II scores over a week of nutritional therapy.14 In another study of patients with acute pancreatitis, there was faster resolution of the disease process among patients treated with enteral feeding compared with similar patients receiving PN.31
The traditional model of SIRS and the compensatory antiinflammatory response syndrome (CARS) described in trauma and sepsis may be influenced by the differential immunologic response between enteral feeding and starvation or gut disuse.32 In SIRS, there appears to be an up-regulated, nonspecific activation of the innate immune system, with an increase in the expression of proinflammatory cytokines such as IL-1, TNF, IL-2, and IFN-γ. This profile is similar to that of the TH1 subset response (in which IFN-γ, TNF, and IL-2 are produced). Intracellular bacteria and viruses absorbed through the intestinal epithelium may activate dendritic cells, macrophages, and natural killer cells to produce IL-2 and IFN-γ, which causes naive CD4 cells to proliferate into TH1 cells. CARS, in contrast, appears to be a pattern of macrophage deactivation, reduced antigen presentation, and T-cell anergy, which results in a shift of the T–helper cell pattern to a TH2 response.32 Gut disuse following injury or illness may promote a SIRS response through stimulation of both the innate immune system (causing a hyperinflammatory response from macrophages and natural killer cells) and the acquired immune system (resulting in a shift from a TH2 to a TH1 profile).
Compared with the metabolic response to enteral feeding, this exaggerated stress response to gut disuse with or without PN has been shown to exacerbate disease severity, increase the rate of complications, and lead to prolongation of the disease process.14,31 There is thus little justification to prolonging NPO status in critically ill patients beyond the period absolutely necessary during resuscitation, surgery, or other procedures. Process-improvement efforts aimed at minimizing starvation is an important goal of any modern ICU.
 Impact of Enteral Nutrition on Outcome
Impact of Enteral Nutrition on Outcome
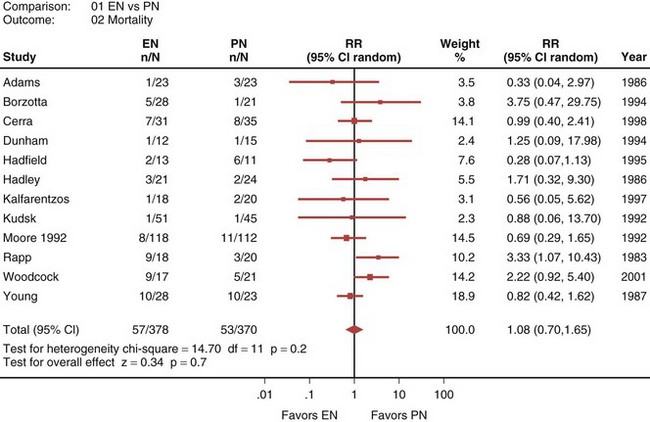
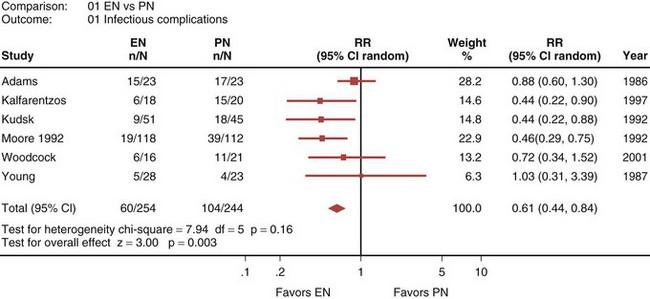
A recently published systematic analysis reviewed data from 13 randomized controlled studies comparing EN and PN in heterogeneous populations of ICU patients, including those with head trauma, abdominal trauma, sepsis, and severe acute pancreatitis, among other conditions.33 When a meta-analysis was carried out, there was no apparent difference in mortality rate between patients treated with EN and those treated with PN (relative risk [RR] 1.08; 95% confidence interval [CI], 0.70-1.65; Figure 94-1). However, compared with PN, EN was associated with a significant reduction in infectious complications (RR 0.61; 95% CI, 0.44-0.84; Figure 94-2).
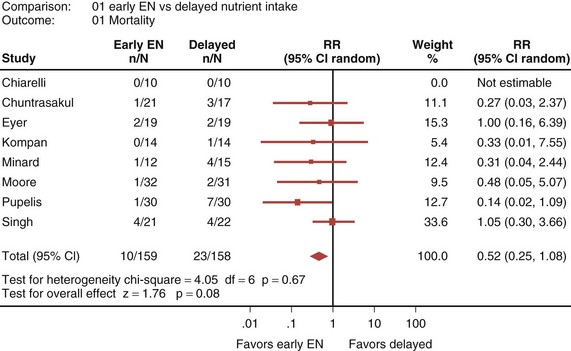
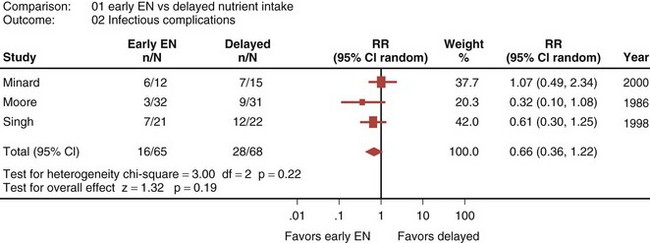
Eight randomized controlled trials that compared early EN with more delayed forms of nutrition were recently reviewed and analyzed.33 When these studies were aggregated, early EN was associated with treatment benefits that approached statistical significance. Early EN was associated with reduced mortality (RR 0.52; 95% CI, 0.25-1.08; Figure 94-3) and fewer infectious complications (RR 0.66; 95% CI, 0.36-1.22; Figure 94-4) compared with delayed nutrient intake. These differences approached but did not achieve statistical significance. No differences in length of hospital stay were observed between the groups. All seven studies that reported nutritional endpoints (e.g., nitrogen balance) showed a significant benefit for early EN. There were no differences in complications between the groups.
A number of strategies can be employed to maximize the delivery of EN while minimizing the risks of gastric colonization, gastroesophageal regurgitation, and pulmonary aspiration (Box 94-1). By delivering enteral feeds into the small bowel beyond the pylorus, the frequency of regurgitation and aspiration is decreased.34 In a recent meta-analysis, there were seven randomized trials that evaluated the effect of route of feeding on rates of ventilator-associated pneumonia.35 When these results were aggregated, there was a significant reduction in ventilator-associated pneumonia with feeding distal to the pylorus (RR 0.76; 95% CI, 0.59-0.99). These studies also demonstrated that small-bowel feeding is associated with an increase in protein and calories delivered and a shorter time to attain the target dose of nutrition.
Unless logistic problems represent an unacceptable hurdle, we recommend routine use of small-bowel feedings. If routine use of this strategy is not feasible, small-bowel feedings should be considered for patients at high risk for intolerance to EN (e.g., patients receiving inotropic or vasoactive drugs, continuous infusion of sedatives, or paralytic agents; or those with large volumes of nasogastric drainage) or at high risk for regurgitation and aspiration (e.g., patients kept supine). Finally, if obtaining small-bowel access is not feasible (e.g., because access to fluoroscopy or endoscopy is limited and blind techniques are not reliable), small-bowel feedings should be considered for selected patients who repeatedly have large gastric residual volumes and are not tolerating adequate amounts of EN intragastrically.33 Additional strategies to maximize the benefits of EN while minimizing the risks (see Box 94-1) include caring for the patient with the head of the bed elevated 30 to 45 degrees,36 using GI promotility agents, reducing doses of opioids,37 and using nurse-directed feeding protocols that include frequent checking of gastric residual volumes.38,39
 Assessment of the Critically Ill Patient
Assessment of the Critically Ill Patient
The clinician must first evaluate the level of stress in a critically ill patient to determine the likelihood of deterioration in nutritional status and to assess the overall need for aggressive nutritional support. Standardized scoring systems such as APACHE II or APACHE III, the Injury Severity Score (ISS), and the Abdominal Trauma Index (ATI) can be helpful for determining the level of stress and the likelihood of deterioration in nutritional status.40,41 Scoring systems have also been used to assess the need for nutritional support in patients with acute pancreatitis.42 Patients with an APACHE II score greater than 10 and having more than three Ranson’s criteria require additional nutritional support.42
Assessment of the patient’s nutritional status is difficult in the ICU. Classic chemical biomarkers, such as circulating levels of albumin and prealbumin, and immunologic parameters, such as lymphocyte counts, are all affected by the inflammatory response observed in critical illness. It is also the case for other parameters such as isokinetic dynamometry. Clinicians therefore have to be diligent at obtaining an excellent history and physical examination, identifying clinical signs of malnutrition. A history of poor nutrient intake and recent weight loss should alert the clinician that gut assimilation may be a problem, that more aggressive delivery of enteral or parenteral nutrients is appropriate, and that there is a greater need to meet calorie and protein requirements sooner in the hospital course (see Figure 94-2).
If the overall level of stress and severity of illness indicate the need for nutritional support, the clinician must next evaluate the status of the GI tract. Intravascular volume status should be optimized before initiating enteral feeds. It is not safe to infuse nutrients into the gut if there is ongoing ischemia or a high risk of mesenteric hypoperfusion. Feeding standard enteral formulas to patients with hypotension, hypovolemia, or septic shock, especially when vasopressors are being used to support blood pressure, may precipitate bowel ischemia.43
When EN is started soon after the onset of critical illness (i.e., enteral nutrients have been lacking only a short time), one can presume that the integrity of the intestinal mucosa is well maintained, and a standard enteral formula can be used. If the period of gut disuse has been more prolonged, the clinician must consider the possibility that mucosal integrity is not normal. If there is evidence of malassimilation and diarrhea, enteral formulas containing oligopeptides may enhance absorption and assimilation of protein.44 In a recent review of 19 prospective randomized trials in humans, 11 studies showed evidence of clinical benefit when oligopeptide-containing formulas were used instead of standard enteral (intact protein) formulas. Although there was no impact on patient outcome, the benefits of oligopeptide-based diets included significantly improved nitrogen absorption, higher visceral protein levels, more weight gain, less frequent stooling, and reduced stool volume.44
Once EN is started, the clinician must monitor tolerance. Overall assimilation of nutrients by the enteral route is assessed clinically by checking for the presence or absence of diarrhea. Additionally, it is important to monitor circulating concentrations of glucose, triglycerides, urea nitrogen, and creatinine ratio. Risk factors for aspiration include age older than 60 years, decreased level of consciousness, bolus feeding, and supine position.45–47 Gastric residual volumes, output from the gastric port of an aspiration or feeding tube, and passage of stool and gas are valuable indices of intestinal motility.
 Practical Considerations
Practical Considerations
All critically ill patients require a nutritional evaluation, and many benefit from receiving nutritional therapy. The complexity and degree of nutritional intervention necessary is proportional to the patient’s severity of illness. In the ICU, nutritional intervention is subject to the same rules of any medical therapy demonstrating a mechanism of action, a benefit in clinical outcome, acceptable risks and side effects, and ideally a cost benefit. The form of nutritional intervention a given patient should get is not necessarily intuitive. In certain disease processes associated with high severity of illness—trauma, burns, acute pancreatitis, acute respiratory failure requiring mechanical ventilation, for example—the decision to use the parenteral rather than the enteral route for feeding can significantly affect outcome.48,49
The greater importance of EN among sicker patients was first shown by evaluating septic complications in trauma patients randomized at the time of surgery to receive either PN or EN.50 Patients were ranked for severity of disease by their ATI scores. Among patients with ATI scores higher than 24, the incidence of septic complications was greater in the PN group than in the EN group (47.6% versus 11.1%; P < 0.05). Among patients with moderate illness and ATI scores lower than 24, there was no significant difference in the incidence of septic complications between the PN and EN groups (29.2% versus 20.8%; P = NS).50
Further evidence of the importance of maintaining gut integrity in patients with more severe disease was provided by a series of prospective randomized controlled trials of EN versus PN in patients with acute pancreatitis.14,51,52 In the first trial published, feeding by the enteral route was shown to be safe, but only 19% of the patients had severe pancreatitis, and there were no differences in the rates of nosocomial infection, organ failure, or overall complications.52 In a second study, 38% of the patients had severe pancreatitis, and a significantly greater percentage of those fed enterally rather than parenterally had resolution of SIRS over the first week of therapy (81% versus 17%; P<0.05); nevertheless, there were no differences between the groups with respect to rates of nosocomial infection or complications.14 In a third study, 100% of the patients had severe pancreatitis, and septic complications were reduced from 50% in the PN group to 28% in the EN group (P<0.05); the overall rate of complications was reduced from 75% in the PN group to 44% in the EN group (P<0.05).51
For EN support, clinicians must determine caloric requirements in order to set a goal or mandatory threshold for the volume, or “dose,” of enteral feeding provided. Use of indirect calorimetry or simplistic equations (e.g., 25 kcal/kg/d) to estimate caloric requirements can help identify this threshold amount. Focusing on such a goal volume allows clinicians to determine a dose/response effect of enteral tube feeding; that is, the percentage of this goal volume required to achieve desired therapeutic endpoints (maintenance of gut integrity, containment of intestinal permeability, attenuation of the stress response, reduction of overall disease severity). In the early stages of critical illness, patients are in the throes of the hypermetabolic stress response and more prone to ileus owing to higher doses of narcotics, electrolyte abnormalities, and shifts in fluid volume. In this situation, it is difficult to provide full caloric requirements. The minimum amount or volume of feeds (as a percentage of total caloric requirements) sufficient to achieve the desired therapeutic effect is not known. Recent evidence suggests that “trophic” or “trickle” rates of feeding (usually meaning 10-30 mL/h of a nutritional formula containing ≈1 kcal/mL) are probably inadequate to provide demonstrable benefits. Data from clinical studies indicate that 50% to 65% of goal calories are needed to prevent increases in intestinal permeability in burn victims9,53 and bone marrow transplant patients (M.T. Demeo, personal communication), promote better and faster return of cognitive function in head injury victims,54 and reduce the duration of mechanical ventilation and ICU and hospital length of stay in critically ill patients.55 When higher feeding rates are not feasible, trickle feeds may have limited value and should be provided, but efforts to infuse greater volumes should be continued.
 Immunonutrition
Immunonutrition
L-arginine
The amino acid, L-arginine, plays fundamental roles in protein metabolism and polyamine synthesis and is a critical substrate for nitric oxide (NO) production.56 L-Arginine stimulates the release of growth hormone, insulin growth factor, and insulin, all of which may stimulate protein synthesis and promote wound healing. The enzyme, L-arginase, metabolizes L-arginine to L-ornithine, an amino acid implicated in wound healing. NO is produced by a family of enzymes called nitric oxide synthases (NOSs) which exist in constitutive and inducible isoforms.57 Under normal conditions and in some disease states, small quantities of NO are synthesized by the constitutive forms, which have a beneficial effect on tissue oxygenation, vasodilation, and immune function.58

Full access? Get Clinical Tree