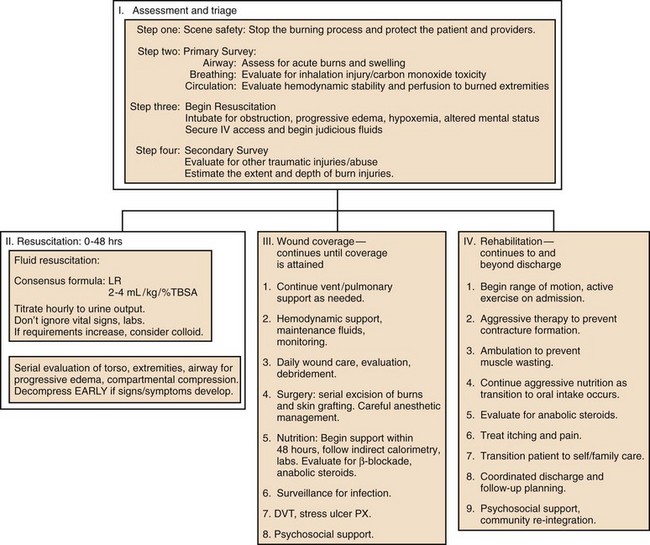
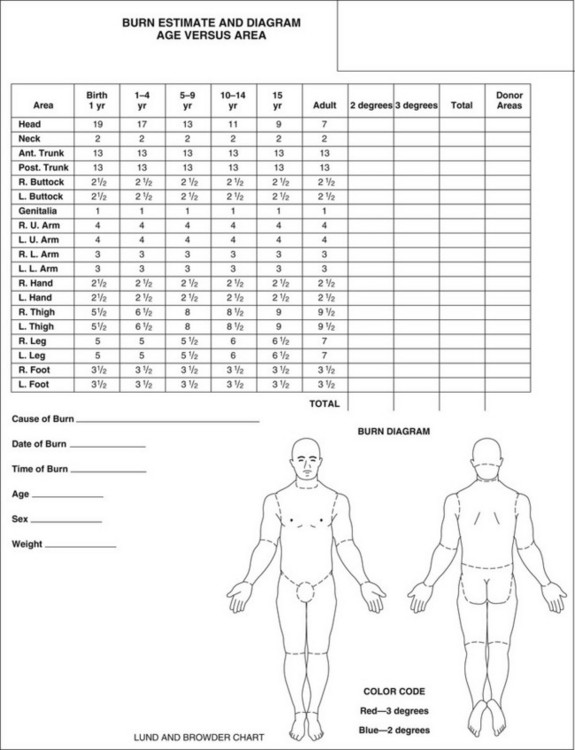
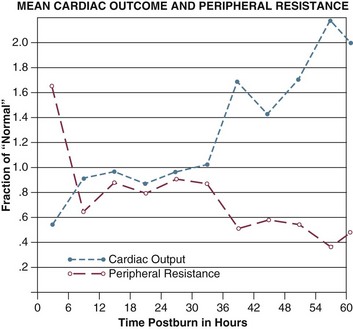
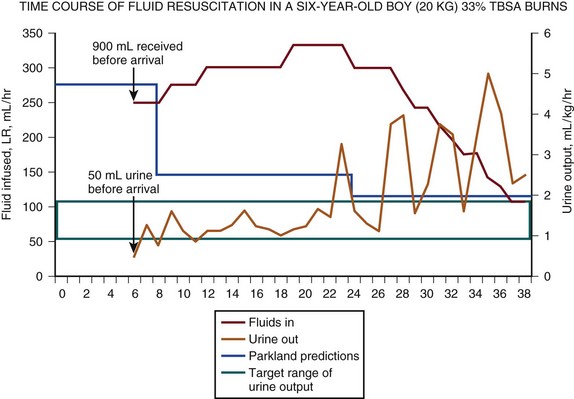
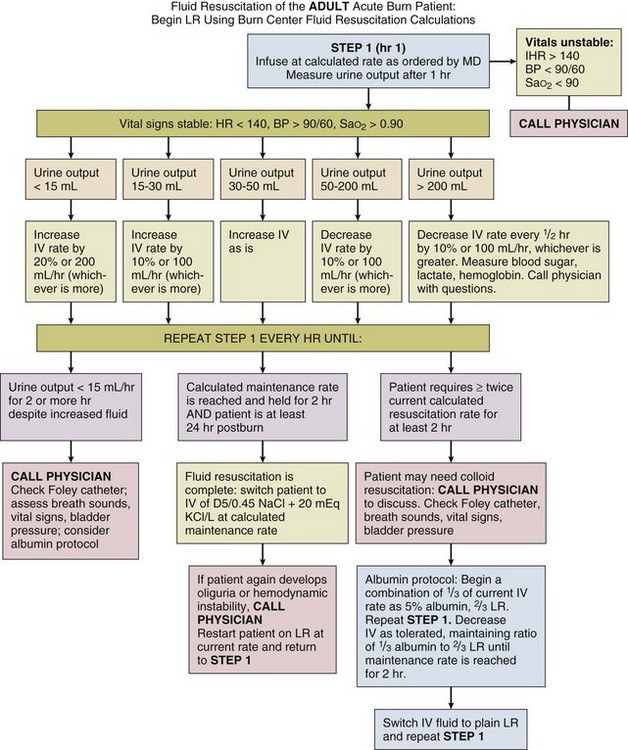
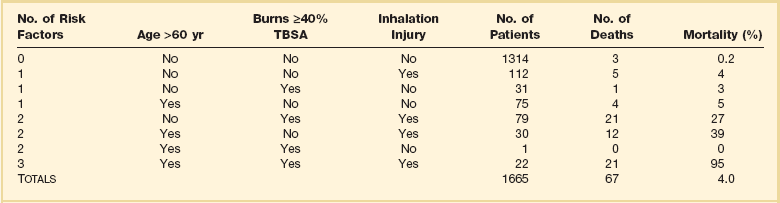
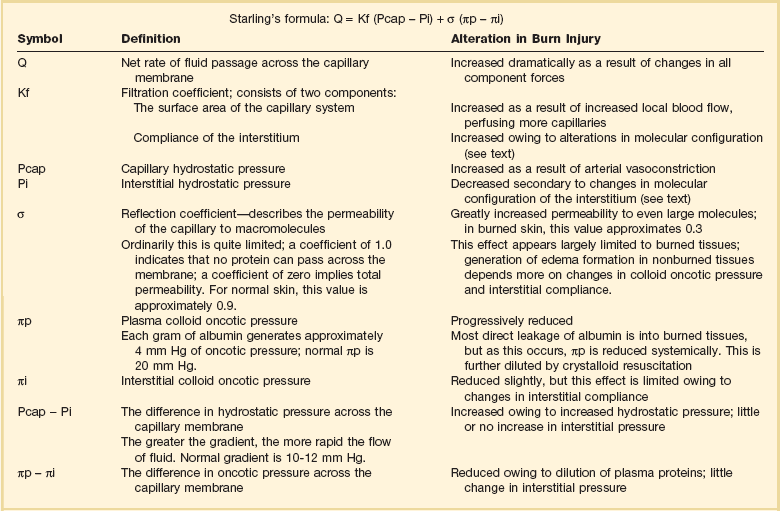
67 This chapter will review the critical care management of burned adults. It will be apparent that in many areas existing literature is neither comprehensive nor rigorously “evidence-based.”1 In providing a rationale for treatment, therefore, it is often necessary to extrapolate from studies in other disorders, particularly trauma. This may or may not be valid, particularly in such “burn-specific” areas as fluid resuscitation, inhalation injury, and nutritional support. These issues will be discussed as they arise, but readers will need to interpret this information for themselves. The incidence of burn injury has declined in the United States throughout recent decades. From the 1960s to the early 1990s, reported burns decreased from 10.2 to approximately 4.2 injuries per 1000 Americans annually, or about 1.25 million injuries2; hospitalizations decreased from over 90,000 to approximately 52,000/year; and deaths decreased at least 40%, from 9000/year to 5500/year. These trends are likely to continue. Simultaneously, survival from burns has improved dramatically. During World War II, burns of 40% total body surface area (TBSA) produced a 50% mortality rate; today a similar mortality rate is seen with burns of over 80% TBSA.3 Survival rate is lower—though still improved—for the elderly, and even higher for children and young adults.4 These accomplishments are due to cumulative advances in fluid resuscitation, critical care, nutrition, surgery, and skin substitutes. However, it has been the organization of specialized burn centers around a consolidated team of experts that has made this success possible.5 Burn survival has been repeatedly shown to correlate with three major factors: patient age, burn size, and the presence of inhalation injury. Pulmonary damage from smoke inhalation is itself a serious injury, and can as much as double the mortality rate from cutaneous burns alone.3,5 Ryan and colleagues found that burn size 40% TBSA or greater, age 60 years or older, and inhalation injury contributed to the mortality rate in a stepwise manner; patients with all three had a mortality rate of 90% (Table 67.1).6 Table 67.1 Risk Factors for Death from Burn Injuries* TBSA, total body surface area. *This table indicates the three risk factors universally accepted to affect burn patient mortality rate, their prevalence, and relative contribution to mortality rate. These data are similar to those from many modern burn centers. Note that overall mortality rate is only 4% and that most patients are relatively young and have limited burn wounds, placing them at little risk of dying. Adapted with permission from Ryan CM, Schoenfeld DA, Thorpe WP, et al: Objective estimates of the probability of death from burn injuries. N Engl J Med 1998;338(6):362-366. Copyright ©1998, Massachusetts Medical Society. All rights reserved. This experience has two important implications for current and future burn treatment. First, mortality risk for many patients is now so low that almost no injury is too large to preclude survival. The decision to intentionally withhold treatment is now rare and is based on predicted quality of life rather than predicted fatality itself. Second, it has necessitated unprecedented research and interest on the rehabilitation of patients who increasingly survive catastrophic injuries. Functional outcomes of burn treatment, including quality of life and return to work, are now the most relevant measures of successful care for all patients.7,8 However, the decline in burns has had other unintended consequences, which create challenges to the provision of effective burn care in many areas. As burns have decreased, so has the number of burn centers in the United States. There are now over 25% fewer burn centers than in 19709; only 60 facilities in the United States are currently verified by the American Burn Association (ABA) and American College of Surgeons (ACS).10 This reduced number limits access to specialized burn care for many Americans. For the same reason, the experience of most physicians with even basic burn care has been dramatically reduced; many U.S. doctors—even surgeons—receive little or no burn training. As a result, important errors in initial burn assessment are made commonly by primary care providers,11–13 leading to significant under- or (mostly) overtriage, care that is sometimes inadequate, and further stress on the few remaining centers, which now must cover larger referral areas.14,15 Acute burn treatment can be divided into four phases, which are outlined in Figure 67.1. Initial assessment is the process of stabilizing the acutely injured patient, treating immediate life-threatening injuries, and preparing for inpatient care. The first 48 hours following injury constitute acute resuscitation, focused on initial assessment, airway support, and fluid replacement. The wound coverage phase then ensues, in which the major goal of treatment is surgical excision and closure of burn wounds. Ventilator management, metabolic support, control of infection and pain, physical therapy, and other supportive measures are essential adjuncts during this period. The goals of the final rehabilitation phase include scar control, optimizing function, and return to independent living. This period can last for months and continue long past discharge. Obviously these phases overlap: discoveries made during initial assessment may require prolonged management; many units begin surgical excision even before resuscitation is completed, and several aspects of rehabilitation—physical therapy, psychosocial support, nutrition, etc.––should start essentially at the time of injury. Initial assessment of burn victims should follow the universally accepted protocol of the American College of Surgeons’ Advanced Trauma Life Support (ATLS) course.16 In doing so, attention must be paid to several burn-specific issues, but it must be remembered that other types of trauma or preexisting conditions can always be present, emphasizing the importance of systematic patient evaluation. In burn patients, assessment of airway, breathing, and circulation must include evaluation for signs and symptoms of inhalation injury. Carbon monoxide (CO) poisoning and asphyxia cause the vast majority of scene and emergency room fatalities, and up to 80% of fire-related deaths.17,18 Inhalation injury and its management are covered in Chapter 48. Inhalation injury should be suspected in all patients exposed to flames or smoke, especially if the patient was unconscious or trapped in a closed space. Physical findings include facial burns, singed nasal hairs or eyebrows, wheezing or stridor, carbonaceous sputum, hoarseness, and anxiety. These findings should alert the examiner to the possible need for airway support.19 CO is a product of incomplete combustion, and its highest concentrations occur in indoor fires, where its effects may be amplified by flame-induced oxygen depletion.20 CO displaces oxygen binding, producing systemic hypoxia despite normal oxygen tension. The most common symptoms are mental status changes, varying from headache to coma, which can present without burn injuries or respiratory distress and be overlooked easily. Classic “cherry red cyanosis” appearance is absent in many victims or can be obscured by soot or burns. Importantly, pulse oximetry is inaccurate in the presence of CO. Direct measurement of carboxyhemoglobin concentration should be performed but should never delay treatment. Patients are at greatest risk on presentation, and immediate application of oxygen is often definitive. As reviewed in Chapter 48, the use of hyperbaric oxygen for acute CO poisoning is controversial; it should probably be reserved for severe cases with neurologic compromise, when its use will not interfere with other essential components of acute burn care. Smoke contains many other toxic chemicals, including cyanide. Cyanide poisoning has been documented in burn victims and does not always correlate with CO exposure.21 Because blood levels cannot be obtained immediately, empiric treatment using cyanide antidote kits has been advocated in patients with unusually severe acidosis or shock.22 The recent availability of hydroxocobalamin as a cyanide antidote, which has few side effects, has led to both renewed interest in the treatment of cyanide toxicity and aggressive marketing of the drug. However, a recent review points out that confirmed cases of significant cyanide poisoning following smoke exposure are rare.23 At present, treatment of suspected cyanide toxicity in acutely burned patients is controversial, and indications are unclear.24 High-flow oxygen coupled with aggressive resuscitation and cardiovascular support remain the mainstays of treatment. Patients with extensive or deep burns to the face, or who have breathed substantial quantities of hot gases or soot, are at risk of airway occlusion from progressive pharyngeal or supraglottic edema and facial swelling. This swelling can occur even without flame injury in children with scalds or severe chemical burns. Edema formation can be extremely rapid and progress for at least 24 hours. Patients must be followed serially, and intubated early and electively if evidence of progressive airway compromise occurs. Figure 67.2 illustrates such a case. Awareness of the potential for acute airway compromise following burn injury has led to a liberal attitude toward intubation that is probably appropriate. “When in doubt, intubate” expresses many physicians’ attitude toward this problem. However, this dictum has sometimes led to indiscriminate and unnecessary intubation of patients with even minor facial burns.25 The presence of inhalation injury does not mandate intubation, and airway compromise can be life-threatening even in the absence of inhalation injury. Indications for intubation, as in all trauma patients, are based on symptoms found on initial assessment, including altered mental status, refractory hypoxemia, and signs of impending airway obstruction including wheezing, stridor, dyspnea, and progressive facial swelling. Emergency tracheostomy or cricothyroidotomy, which should rarely be needed if intubation is performed in a timely manner, can be an extremely challenging procedure in the setting of massive head and neck swelling. Exposure of the bronchi and small airways to toxic smoke causes chemical injury to the epithelium, which can progress to mucosal sloughing, mucous plugging, bronchiectasis, hypoxemia, and pneumonia. Clinical signs of this problem may be absent for up to 72 hours after exposure, and initial chest radiographs are usually normal.26 Patients with immediate respiratory distress, stridor, or hypoxemia are much more likely to have upper airway injury. Even in the absence of symptoms, patients suspected of having inhalation injury require hospital admission and close observation. Fiberoptic bronchoscopy demonstrating carbonaceous debris, erythema, or mucosal sloughing is highly sensitive for diagnosis of inhalation injury and can facilitate immediate intubation if injury is confirmed27 (Fig. 67.3). Inhalation injury is discussed further in Chapter 48. Following quick initial assessment, intravenous resuscitation and other support should be initiated. As resuscitation is beginning, a thorough head-to-toe examination is performed. Burn victims frequently suffer other trauma, which can be obscured by overlying burns (see later). Much of the subsequent care of the burn patient is based on assessment of the extent and depth of injury, including fluid resuscitation, nutritional requirements, surgery, and in extreme cases, the decision to provide aggressive treatment. For these reasons, the burn wound should be washed and thoroughly debrided and then documented as accurately as possible, preferably by an experienced clinician. Rough estimates of burn size are often made using the “rule of nines”; more accurate detailed documentation can be done using the Lund and Browder chart (Fig. 67.4). Computerized programs are also becoming popular, such as the Sage diagram (www.sagediagram.com). In evaluating smaller injuries, another useful rule is that the area of the patient’s palm (with fingers) equals about 1% of his/her TBSA. The many mishaps that cause burns often cause other trauma as well. These situations can include explosions (blasts, falls, projectile wounds), electrocutions (tetany-induced fractures, falls), fires in motor vehicle or airplane crashes, and escaping fires (lacerations, falls). Combined burn/trauma injuries are particularly likely following assault or child abuse and should increase suspicion for such causes.28 The combined mortality rates for burns and trauma appear to be at least additive compared to either injury alone.29,30 Thorough evaluation of all potential injuries according to ATLS guidelines is imperative and can be challenging in burn patients: the discoloration, pain, and swelling of burn wounds, for example, can conceal underlying fractures31; and burns of the torso or acute inhalation injury can obscure a pneumothorax or other injuries. For this reason, it is important not to focus too heavily on burn injuries in performing the secondary survey. In addition, care should be provided by a multispecialty team with expertise in managing all injuries. Treatment of many traumatic injuries takes priority over definitive burn care and mandates immediate operation. Because fresh burn wounds are initially—and briefly—free of bacteria, laparotomy, craniotomy, repair of lacerations, and operative fixation of fractures should be performed immediately, and no later than 12 to 24 hours after burn.32,33 This approach will minimize risk of infections, permit early mobilization, and facilitate access to burn wounds for dressings and surgery. These interventions can be performed safely provided essential components of burn care—including airway support, temperature control, and aggressive fluid resuscitation—are instituted immediately and continued through surgery. Close coordination between the burn center and trauma center will optimize outcome for these patients. Following initial evaluation, the primary focus of early burn treatment is fluid resuscitation. The goals of resuscitation are to support organ function while avoiding complications of over- or underadministration of fluid.34 This task can be challenging given the huge fluid shifts and cardiovascular effects of acute burns. Development of effective protocols for resuscitation represents one of the major advancements in burn care in this century. The magnitude of fluid shifts following a major burn can exceed those of any other injury. At the cellular level, burn injury immediately impairs membrane adenosine triphosphatase (ATPase) activity and reduces transmembrane potential,35,36 resulting in increased intracellular sodium and extracellular potassium concentrations, cellular swelling, and acidosis. Fluid resuscitation only partially corrects these abnormalities, which may require several days to resolve completely as local inflammation subsides. These events present clinically as a profound inflammatory response, causing increased capillary permeability and massive tissue edema at the expense of intravascular volume. Immediate release of histamine and serotonin increase local perfusion, initiate capillary leakage, and potentiate vasoconstriction caused by massive catecholamine secretion.36–38 Tumor necrosis factor (TNF)-α produces myocardial depression and activates a number of other vasoactive mediators.39 Prostaglandins, leukotrienes, oxygen radicals, products of platelet activation and coagulation, and a cascade of cytokines also contribute to these abnormalities.40,41 Alterations in local blood flow increase arteriolar tone and pressure and dilate postcapillary venules, causing local capillary perfusion to become less selective and increased, favoring extensive edema formation. The forces that control transcapillary fluid flux are summarized in Starling’s equation42; their alterations in burn injury have been reviewed by Demling43 (Table 67.2). The greatest edema formation occurs almost immediately within the wound, caused by near-total permeability to even very large (35 nm) molecules,44 and permitting protein-rich plasma to pour into the interstitium.45 Maximum protein extravasation occurs within the first hour of injury, and both its duration and magnitude are proportional to burn size.46,47 Table 67.2 Starling Forces and Capillary Permeability* *See discussion in Demling RH: The burn edema process: Current concepts. J Burn Care Rehabil 2005;26:207-227. Adapted with permission from Ryan CM, Schoenfeld DA, Thorpe WP, et al: Objective estimates of the probability of death from burn injuries. N Engl J Med 1998;338:362-366. Copyright ©1998, Massachusetts Medical Society. All rights reserved. Even after local capillary integrity normalizes within 8 to 12 hours, edema formation continues in unburned as well as burned tissues.48 Depletion of intravascular proteins, further diluted by crystalloid resuscitation,49 eliminates the oncotic pressure gradient (see πp − πi in Table 67.2), which maintains intravascular volume. Hypoproteinemia alone can mimic burn edema, and infusions of colloid can almost completely prevent edema in unburned tissues.50,51 Progressive edema also alters the configuration of interstitial collagen and hyaluronic acid, which are normally densely coiled to limit fluid influx.52 Burn injury disrupts this “safety valve” configuration, increasing compliance, producing osmotically active molecular fragments, and generating negative (“sucking”) interstitial pressure53 and extremely rapid fluid sequestion.48 Though this gradient is neutralized within a few hours, compliance continues to increase as interstitial gel is hydrated, allowing liters of fluid to accumulate with little change in hydrostatic pressure54 and permitting edema to persist for weeks following injury. Cardiac output falls within minutes of injury, reaching 50% to 60% of normal within an hour, although systemic vascular resistance (SVR) increases dramatically. Both changes occur far faster than the depletion of intravascular volume45,55 and regardless of fluid resuscitation. Release of catecholamines and other vasoactive mediators clearly increases SVR, but the decrease in cardiac output is harder to explain. Researchers have long postulated the existence of a “myocardial depressant factor,”56 though no such substance has been isolated. It seems more likely that cardiac output is impaired by the combination of increased SVR, volume depletion, and actions of TNF-α, endotoxin, and other chemicals. One clinically important side effect of capillary permeability is hemoconcentration—a marked rise in hematocrit as plasma is sieved out of the bloodstream into the interstitium—which increases blood viscosity and further impairs cardiac output. Cardiac output begins to recover within a few hours of injury and requires 12 to 24 hours to normalize, even with vigorous resuscitation. SVR follows an opposite course, peaking quickly and then declining to near-normal within 24 to 48 hours (Fig. 67.5). Following these initial changes a chronic hyperdynamic circulation is maintained, with cardiac output persisting well above normal, and marked vasodilation and decreased SVR often persisting even after wound coverage is attained. Before World War II, patients with even moderate burns usually died within a few days because of progressive shock and renal failure. In 1942, surgeons Oliver Cope and Francis Moore designed the first formal resuscitation regimen to treat victims of the Cocoanut Grove nightclub fire, with substantial improvements in survival.36 With continued refinements, today almost all patients can be resuscitated successfully, and renal failure complicating burn injury is rare. A host of formulas have been developed, almost all based on body weight and burn size, and utilizing various combinations of crystalloid and colloid solutions. The archetype and most widely used of such regimens is the Parkland formula, designed by Baxter.35 He demonstrated that a volume of lactated Ringer’s (LR) solution equal to 4 mL per kilogram body weight for each percent TBSA burned (4 mL/kg/%TBSA), given in the first 24 hours after injury, would maintain urine output of 50 to 70 mL/hour, replete blood volume, and restore cellular transmembrane potential and cardiac output in most patients. Half this calculated volume is given in the first 8 hours after burn, the remainder over the next 16 hours. The intravenous rate is adjusted hourly to maintain urine output and is decreased gradually until a “maintenance” rate is reached at approximately 24 hours. Maintenance requirements for burn patients are also increased due to ongoing evaporative and metabolic losses, and continued fluid support is essential even after resuscitation is complete. A popular formula to estimate these requirements is that developed by Warden:57 In this equation, This experience forms the basis of modern burn resuscitation. But despite widespread acceptance of the principles of fluid replacement, disagreement persists over almost every aspect of practical management, and the practice of resuscitation varies significantly among units. One example exists in defining the end points of resuscitation. Successful resuscitation requires meticulous monitoring and adjustment of resuscitation based on patient response. Traditional resuscitation relies almost exclusively on hourly urine output for this purpose, so the amount of fluid required for resuscitation depends partly on the urine output targeted. Baxter used an output of 50 to 70 mL/hour; several other formulas that accept outputs of 0.5 mL/kg/hour (1.0 mL/kg/hour in children) call for LR infusion rates between 2 and 3 mL/kg/%TBSA, and are also in widespread use.34,36 Clinicians have long accepted the consensus that patients should receive as little fluid as possible to maintain organ perfusion.58 But several patient groups routinely require more resuscitation fluid than predicted by the Parkland formula, including patients with inhalation injury,59 those with multiple trauma and electrical burns, patients in whom resuscitation is substantially delayed,4 and patients with alcohol or drug abuse.60 Inexperienced clinicians often make substantial errors in estimating burn size, which can result in significant under- or overestimation of fluid requirements.11 Careful monitoring of resuscitation and individualized fluid therapy can often obviate these problems. But in recent years a widespread tendency for patients to receive increasing quantities of resuscitation fluid has been observed, a phenomenon dubbed “fluid creep” by Pruitt.61 Cancio and associates found that 63% of their recent patients required a mean of 6.1 ± 0.22 mL/kg/%TBSA for resuscitation despite very modest urine output.62 Others have documented such increased fluid requirements in up to 100% of patients.63–65 The potential complications of fluid creep are far from benign, including extremity and abdominal compartment syndromes, worsening pulmonary dysfunction, and more frequent and prolonged endotracheal intubation. Figure 67.6 illustrates the actual resuscitation of a child who required an excessive amount of crystalloid to achieve successful resuscitation and maintain adequate urine output. This departure from tradition is probably due to several influences. First, the successful resuscitation of patients with massive burns appears to routinely require increased fluid volumes.62 In Baxter’s initial report of 277 patients, 89% of those with burns 60% TBSA or greater died.45 However, modern survival is much better and owes some of its success to persisting with aggressive fluid resuscitation beyond the confines of the Parkland formula. Second, it appears that fluid creep perpetuates itself. Overly zealous initial fluid administration—often performed in the field—increases serum protein depletion, generating a vicious circle of reduced oncotic pressure and enhanced edema, which in turn increases crystalloid requirements. This mechanism also helps explain the occurrence of resuscitation failure, in which fluid requirements actually escalate despite adequate—or excessive—crystalloid administration.66 The use of colloid-containing fluids can arrest this cycle and restore oncotic pressure but adds to overall fluid requirements as well. Fluid creep has probably also been encouraged by resuscitation trends in other ICU populations. Traditional burn resuscitation formulas permit significant deficits in vascular volume and cardiac output to persist until the end of 24 hours.45 The routine observation of hematocrits as high as 70% during resuscitation is consistent with this concept. Both lactic acid (LA) and base deficit (BD) remain elevated throughout traditional resuscitation,67 which also fails to reflect changes in cardiac output and oxygen delivery (VO2).68 In contrast, resuscitation in other shock states has been increasingly directed at normalizing LA and BD, and optimizing cardiac output, VO2, and pulmonary wedge pressure.69,70 As this concept gained acceptance in critical care, burn clinicians have become more inclined to monitor these parameters and to respond to abnormalities by increasing fluid support. However, this approach may not be valid in burns. Although it is accepted that patients’ ability to achieve optimal values of cardiac output and VO2 correlates strongly with outcome, it is less clear whether exaggerated fluid infusion, invasive monitoring, and inotropic support can change nonresponders into responders and thus improve survival.71 Optimizing VO2 and improved survival in one group of patients with severe burns,72 but both Kaups and colleagues64 and Choi and coworkers65 were unable to determine if resuscitation aimed at normalizing elevated BD was effective or beneficial. In other studies of goal-directed therapy in burns, attaining target values of cardiac output, VO2, or wedge pressure routinely required more fluid—as much as four times Parkland calculations—without obvious improvement in survival,73,74 and potential increase in edema-related complications, which appear directly related to the fluid volume administered.75,76 Crystalloid solutions remain the mainstay of all resuscitation regimens as they are inexpensive, well tolerated, readily available, and easily mobilized and excreted. The effective component of crystalloid is sodium,77 which has led to the use of hypertonic saline solutions to satisfy capillary and cellular leakage while minimizing fluid volume and edema.78,79 Solutions containing as much sodium as 300 mEq/L result in delivery of almost identical quantities of sodium as LR solution with substantially less volume.80 Hypertonic saline resuscitation has been advocated for children81 and the elderly,82 who tolerate under- and overresuscitation poorly, as well as for patients with head injuries,83 and for field and combat resuscitation when the weight of available solutions must be minimized.84,85 Hypertonic saline resuscitation carries the risk of significant hypernatremia, hyperchloremia, acidosis, and hyperosmolarity, and requires careful monitoring. In addition, savings in initial fluid requirements may be balanced by increased free water retention later.86 Hypertonic saline has been associated with increased mortality risk in at least one study, possibly related to increased renal failure.86 However, it is still used selectively in some burn centers79,87 and remains an option in acute burn management. Because of the indiscriminate nature of early postburn capillary leakage, colloids are not superior to crystalloids in initial burn resuscitation.55 For this and other reasons, colloid use in resuscitation of all types has been condemned.88 However, capillary integrity is largely restored by the end of 24 hours after injury, and colloids given at this time can effectively restore oncotic pressure, expand plasma volume, and reduce secondary edema in unburned tissue,35,51 including possible prevention of abdominal compartment syndrome.89 Colloids used in burn resuscitation have included albumin, plasma protein fraction (Plasmanate), fresh frozen plasma, and the synthetic colloids dextran and hetastarch. Routine albumin administration is a component of the traditional Evans and Brooke formulas36,55 and was originally used at the end of Parkland resuscitation.35 In a widely quoted randomized trial, Goodwin and associates found that albumin-based resuscitation required less total fluid than solution alone but was associated with a sustained increase in extravascular lung water.90 Critics have also pointed out that routine albumin supplementation has no apparent benefits.91 Nonetheless, albumin remains a popular colloid; its current use varies among burn centers from routine administration within 8 to 12 hours of injury,50,57 to selective use as “rescue” in problem resuscitations, to near-total interdiction. Fresh frozen plasma has also been used successfully92; its colloid effect probably explains much of the efficacy of plasma exchange therapy in complex burn resuscitations.93 Both low-molecular-weight dextran and hetastarch have been used in burn resuscitation and appear as effective as albumin in maintaining oncotic pressure and limiting edema in unburned tissues.51,94,95 They offer advantages of long shelf life, availability, freedom from disease transmission, and lower cost. However, hetastarch has been associated with rare anaphylaxis and dose-dependent coagulopathy and bleeding, which limits is use in large volumes.96 Colloid is probably unnecessary for resuscitation of most patients with uncomplicated injuries. With increasing burn size, the benefits of colloid administration, restricted to use after the first 8 to 12 hours after burn, may be significant in reducing total fluid requirements and edema-related complications. Many centers now utilize LR solution for the first hours after injury, followed by hypertonic saline, colloid, or both to reduce edema as resuscitation is completed.57 The patient illustrated in Figure 67.6 would be a very appropriate candidate for this form of “rescue” therapy, which would likely have reduced his ongoing fluid requirements. This area of resuscitation is extremely controversial and will benefit from randomized multicenter trials. Improved understanding of the pathophysiology of burn shock has led investigators to attempt to reduce its severity by blocking some of its specific chemical mediators. These efforts have included use of vasodilators such as hydralazine, histamine blockade using cimetidine, the serotonin antagonist ketanserin, and anti-inflammatory drugs such as hydrocortisone and ibuprofen.43,55,97–99 Large doses of the antioxidant vitamin C has been shown to decrease fluid requirements in clinical burn resuscitation.100 Many of these efforts have shown modest benefits, though none has found its way into widespread clinical use. The possibility of developing an effective “cocktail” to ameliorate the effects of burn shock holds promise for the future. An example of the protocol used at the University of Utah is included in Figure 67.7. The protocol is based on the Parkland formula, but contains an option for the use of LR/albumin to arrest escalating fluid requirements. It requires nurses to adjust infusions based on hourly urine output, but mandates that physicians be contacted if worrisome parameters develop. We have found this protocol effective in resuscitating the vast majority of patients without frequent input from physicians. Similar protocols are in use in a number of burn centers. Full-thickness facial burns can swell massively and produce complete airway obstruction within an hour or 2 of injury, as illustrated in Figure 67.2. As discussed under initial assessment, endotracheal intubation is essential in this setting and should be performed early and electively. Elevated intraocular pressures (IOPs) have been documented in burn patients and appear to correlate with resuscitation volume. No data exist on the consequences of this phenomenon, but the risk of optic nerve ischemia and permanent visual loss may exist. Lateral canthotomy has been recommended for patients with persistently high IOPs.101,102 Measurement of IOP during acute burn resuscitation may be warranted in patients with severe facial injuries and eyelid edema. Swollen extremities should be initially treated with elevation and avoidance of constricting dressings. Classic findings of pain, paralysis, pallor, paresthesia, pulselessness (the “five Ps”) may be difficult beneath burn injuries or in intubated patients, and may not develop until irreversible ischemia has occurred. Similarly, limb-threatening compression can exist despite persistent palpable or Doppler pulses.103 For these reasons, some authorities perform escharotomies based on a general impression of extremity swelling, or even prophylactically. Alternatively, many clinicians monitor intramuscular pressure to determine the need for decompression. This procedure is easily done by inserting a large-bore (18-gauge) needle attached to a pressure transducer through the eschar into the underlying muscle. Pressures that exceed 30 cm H2O in the relaxed extremity indicate compromised capillary perfusion and mandate decompression.104 Measurements should be repeated following escharotomy; pressures that remain elevated indicate the need to deepen or extend incisions or to proceed with fasciotomy. This may be particularly likely in patients with very deep burns, associated trauma, or electrical injury (Fig. 67.8). Escharotomies can often be done at the bedside using electrocautery and appropriate analgesia. Longitudinal incisions should run the length of the burn wound, be placed medially and laterally on the supinated limb to avoid major nerves and vessels, and facilitate resurfacing with skin grafts. Incisions must penetrate through the burn until the wound edges “pop open,” and pressure is clearly relieved. Incisions in burned hands should extend at least to the metacarpophalangeal joints; performance of individual digit escharotomies has some support105 but is often omitted. As an alternative, the use of enzymatic debriding agents to provide chemical escharotomy is popular in some centers.106
Critical Care Management of the Severely Burned Patient
Introduction
Incidence and Survival from Burn Injury
Acute Care of the Burned Patient
Initial Assessment
The Primary Survey and Inhalation Injury
Carbon Monoxide Poisoning
Upper Airway Injury
Indications for Intubation
Pulmonary (“True”) Inhalation Injury
Begin Resuscitation
The Secondary Survey
Burns and Multiple Trauma
The Resuscitation Phase
Burn Shock
Fluid Resuscitation of Burn Patients
The Phenomenon of “Fluid Creep”
Hypertonic Resuscitation
Crystalloid Versus Colloid
Pharmacologic Manipulation of Resuscitation
Practicing Effective Resuscitation
Complications of Edema
Facial Swelling
Ocular Swelling
Extremity Compartment Syndromes
Critical Care Management of the Severely Burned Patient