CHAPTER 16
Corneal Abrasion
Presentation
The patient may complain of eye pain or a sensation of the presence of a foreign body after being poked in the eye with a finger, twig, or equivalent object. The patient may have abraded the cornea while inserting or removing a contact lens. Removal of a corneal foreign body produces some corneal abrasion, but corneal abrasion can occur without any identifiable trauma. There is often excessive tearing, blurred vision, and photophobia. Often the patient cannot open her eye for the examination because of pain and blepharospasm. Abrasions are occasionally visible during sidelighting of the cornea. Conjunctival inflammation can range from minimal to severe conjunctivitis with accompanying iritis.
What To Do:
 Instill topical anesthetic drops to eliminate any pain or blepharospasm and thereby permit examination (e.g., proparacaine [Ophthetic], tetracaine [Pontocaine]).
Instill topical anesthetic drops to eliminate any pain or blepharospasm and thereby permit examination (e.g., proparacaine [Ophthetic], tetracaine [Pontocaine]).
 Perform a complete eye examination (including assessment of best-corrected visual acuity, funduscopy, anterior chamber bright-light examination, and inspection of conjunctival sacs for a foreign body).
Perform a complete eye examination (including assessment of best-corrected visual acuity, funduscopy, anterior chamber bright-light examination, and inspection of conjunctival sacs for a foreign body).
 Perform the fluorescein examination by wetting a paper strip impregnated with dry, orange fluorescein dye and touching this strip into the tear pool inside the lower conjunctival sac. After the patient blinks, darken the room and examine her eye under cobalt-blue filtered or ultraviolet light. (The red-free light on the ophthalmoscope does not work.) Areas of denuded or dead corneal epithelium will fluoresce green and confirm the diagnosis.
Perform the fluorescein examination by wetting a paper strip impregnated with dry, orange fluorescein dye and touching this strip into the tear pool inside the lower conjunctival sac. After the patient blinks, darken the room and examine her eye under cobalt-blue filtered or ultraviolet light. (The red-free light on the ophthalmoscope does not work.) Areas of denuded or dead corneal epithelium will fluoresce green and confirm the diagnosis.
 If a foreign body is present, remove it and irrigate the eye.
If a foreign body is present, remove it and irrigate the eye.
 When a corneal abrasion is present, treat the patient with antibiotic drops, such as trimethoprim plus polymyxin B (Polytrim), 10 mL, 1 drop q2-6h, while awake. Some physicians prefer ophthalmic ointment preparations, which may last longer but tend to be messy. If ointment is preferred, erythromycin 0.5%, 3.5 g, or polymyxin B/bacitracin, 3.5 g, applied inside the lower lid (1- to 2-cm ribbon) qid is effective and least expensive. In patients who wear contact lenses or who were injured by organic material (such as a tree branch), an antipseudomonal antibiotic (e.g., ciprofloxacin [Ciloxan] 0.3%, 1 to 2 drops q1-6h, or ofloxacin [Ocuflox] 0.3%, 1 to 2 drops q1-6h, should be used. Contact lens wearing should be discontinued until the abrasion is healed.
When a corneal abrasion is present, treat the patient with antibiotic drops, such as trimethoprim plus polymyxin B (Polytrim), 10 mL, 1 drop q2-6h, while awake. Some physicians prefer ophthalmic ointment preparations, which may last longer but tend to be messy. If ointment is preferred, erythromycin 0.5%, 3.5 g, or polymyxin B/bacitracin, 3.5 g, applied inside the lower lid (1- to 2-cm ribbon) qid is effective and least expensive. In patients who wear contact lenses or who were injured by organic material (such as a tree branch), an antipseudomonal antibiotic (e.g., ciprofloxacin [Ciloxan] 0.3%, 1 to 2 drops q1-6h, or ofloxacin [Ocuflox] 0.3%, 1 to 2 drops q1-6h, should be used. Contact lens wearing should be discontinued until the abrasion is healed.
 Analgesic nonsteroidal anti-inflammatory drug (NSAID) eye drops of diclofenac (Voltaren), 0.1%, 5 mL, or ketorolac (Acular), 0.5%, 5 mL, 1 drop instilled qid, provide pain relief and do not inhibit healing.
Analgesic nonsteroidal anti-inflammatory drug (NSAID) eye drops of diclofenac (Voltaren), 0.1%, 5 mL, or ketorolac (Acular), 0.5%, 5 mL, 1 drop instilled qid, provide pain relief and do not inhibit healing.
 If iritis is present (as evidenced by consensual photophobia or, in severe cases, an irregular pupil or miosis and a limbic flush in addition to conjunctival injection), consult the ophthalmologic follow-up physician about starting treatment with topical mydriatics and steroids (see Chapter 20).
If iritis is present (as evidenced by consensual photophobia or, in severe cases, an irregular pupil or miosis and a limbic flush in addition to conjunctival injection), consult the ophthalmologic follow-up physician about starting treatment with topical mydriatics and steroids (see Chapter 20).
 Even when there are no signs of iritis, one instillation of a short-acting cycloplegic, such as cyclopentolate 1% (Cyclogyl), will relieve any pain resulting from ciliary spasm.
Even when there are no signs of iritis, one instillation of a short-acting cycloplegic, such as cyclopentolate 1% (Cyclogyl), will relieve any pain resulting from ciliary spasm.
 Although not likely to be available to the non–contact lens user, a soft, disposable contact lens (e.g., NewVue, Acuvue) in combination with antibiotic and nonsteroidal antiinflammatory drops can provide further comfort as well as the ability to see out of the affected eye. As with any contact lens worn overnight, there is probably an increased risk for infectious keratitis; so, this should be provided in concert with an ophthalmologist.
Although not likely to be available to the non–contact lens user, a soft, disposable contact lens (e.g., NewVue, Acuvue) in combination with antibiotic and nonsteroidal antiinflammatory drops can provide further comfort as well as the ability to see out of the affected eye. As with any contact lens worn overnight, there is probably an increased risk for infectious keratitis; so, this should be provided in concert with an ophthalmologist.
 Prescribe analgesics (e.g., oxycodone, ibuprofen, naproxen) as needed, and administer the first dose when appropriate. Most abrasions heal without significant long-term complications; therefore pain relief should be our primary concern with uncomplicated abrasions. This treatment of pain should be guided by an individual patient’s age, concomitant illness, drug allergy, ability to tolerate NSAIDs, potential for opioid abuse, and employment conditions, such as driving and machine operation.
Prescribe analgesics (e.g., oxycodone, ibuprofen, naproxen) as needed, and administer the first dose when appropriate. Most abrasions heal without significant long-term complications; therefore pain relief should be our primary concern with uncomplicated abrasions. This treatment of pain should be guided by an individual patient’s age, concomitant illness, drug allergy, ability to tolerate NSAIDs, potential for opioid abuse, and employment conditions, such as driving and machine operation.
 Warn the patient that some of the pain will return when the local anesthetic wears off.
Warn the patient that some of the pain will return when the local anesthetic wears off.
 Make an appointment for ophthalmologic or primary care follow-up to reevaluate the abrasion the next day. If the abrasion has not fully healed, the patient should be evaluated again 3 to 4 days later, even if he feels well.
Make an appointment for ophthalmologic or primary care follow-up to reevaluate the abrasion the next day. If the abrasion has not fully healed, the patient should be evaluated again 3 to 4 days later, even if he feels well.
 Instruct patients about the importance of wearing eye protection. This is particularly needed for persons in high-risk occupations (e.g., miners, woodworkers, metalworkers, landscapers) and those who participate in certain sports (e.g., hockey, lacrosse, racquetball). Other preventive measures include keeping the fingernails of infants and children clipped short and removing objects such as low-hanging tree branches from the home environment.
Instruct patients about the importance of wearing eye protection. This is particularly needed for persons in high-risk occupations (e.g., miners, woodworkers, metalworkers, landscapers) and those who participate in certain sports (e.g., hockey, lacrosse, racquetball). Other preventive measures include keeping the fingernails of infants and children clipped short and removing objects such as low-hanging tree branches from the home environment.
What Not To Do:
 Do not be stingy with pain medication. The aforementioned treatments may not provide adequate analgesia, and supplementation with NSAIDs or narcotic analgesics may be necessary for a day.
Do not be stingy with pain medication. The aforementioned treatments may not provide adequate analgesia, and supplementation with NSAIDs or narcotic analgesics may be necessary for a day.
 Do not give the patient any topical anesthetic for continued instillation.
Do not give the patient any topical anesthetic for continued instillation.
 Do not miss anterior chamber hemorrhage or other significant eye trauma that is likely to cause immediate visual impairment.
Do not miss anterior chamber hemorrhage or other significant eye trauma that is likely to cause immediate visual impairment.
 Do not use a soft contact lens if bacterial conjunctivitis, ulcer, or abrasions caused by contact lens overwear are present.
Do not use a soft contact lens if bacterial conjunctivitis, ulcer, or abrasions caused by contact lens overwear are present.
 Do not use an eye patch. Although eye patching traditionally has been recommended in the treatment of corneal abrasions, studies now show convincingly that patching does not help healing or pain, interferes with binocular vision, and may even hinder corneal repair.
Do not use an eye patch. Although eye patching traditionally has been recommended in the treatment of corneal abrasions, studies now show convincingly that patching does not help healing or pain, interferes with binocular vision, and may even hinder corneal repair.
Discussion
Corneal abrasions constitute a loss of the superficial epithelium of the cornea (Figure 16-1). They are generally painful because of the extensive innervation in the affected area. Healing is usually complete in 1 to 2 days unless the abrasions are deep, there is extensive epithelial loss, or there is underlying ocular disease (e.g., diabetes). Larger abrasions that involve more than half of the corneal surface may take 4 to 5 days to heal. Scarring will occur only if the injury is deep enough to penetrate the collagenous layer.
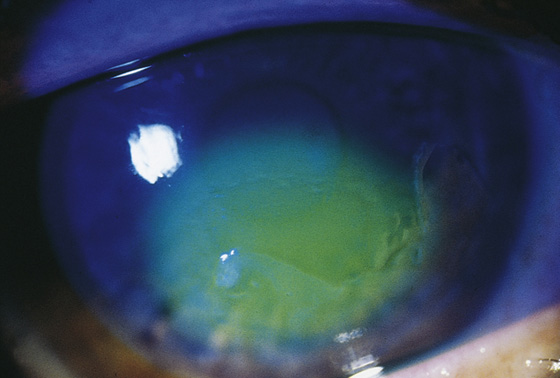
Figure 16-1 Corneal epithelial abrasion showing fluorescein uptake. (From Goldman L, Ausiello D: Cecil Textbook of Medicine, ed 22. Philadelphia, 2004, Elsevier.)
Fluorescein binds to corneal stroma and dead or denuded epithelium but not to intact corneal epithelium. Collections of fluorescein elsewhere—pooling in conjunctival irregularities and in the tear film—are not pathologic findings.
The traditional use of eye patching has been shown to be unnecessary for both corneal reepithelialization and pain relief. Prophylactic antibiotic treatment is used because concomitant infection can cause slower healing of corneal abrasions; however, there is no strong evidence for their use.
Continuous instillation of topical anesthetic drops can impair healing, inhibit protective reflexes, permit further eye injury, and even cause sloughing of the corneal epithelium.
With small, superficial abrasions, ophthalmologic follow-up is not required if the patient is completely asymptomatic within 12 to 24 hours. With deep or larger abrasions or with any worsening symptoms or persistent discomfort, ophthalmologic follow-up is necessary within 24 hours because of the risk for corneal infection or ulceration. Ophthalmologic follow-up is also required for recurrent corneal erosions—repeated spontaneous disruptions of the corneal epithelium. This can occur in corneal tissue weakened by abrasion months or years earlier. Symptoms are the same as those for corneal abrasions but occur spontaneously on awakening and opening the eyes or after simply rubbing the eyes. Lesions usually are found near the original abrasion.
Patients who wear contact lenses should also be reevaluated in 24 hours and again 3 to 4 days later, even if they feel well. Hard and soft contact lenses can abrade the cornea and cause a diffuse keratitis or corneal infiltrates and ulcers (see Chapter 15).
In follow-up examination of corneal abrasions, inspect the base of the corneal defect, ensuring that it is clear. If the base of the abrasion becomes hazy, it may indicate the early development of a corneal ulcer and demands immediate ophthalmologic consultation.

Full access? Get Clinical Tree


