(1)
Aschaffenburg, Germany
5.1 Introduction
5.3 Epidemiology
5.5 Diagnostics
5.5.5 Differential Diagnosis
5.6 Classification
5.8.1 History
5.8.2 Informed Patient Consent
5.8.3 Instruments
5.10 Results
5.1 Introduction
Posttraumatic dystrophy was first completely described by Sudeck in 1900 and 1902. Apart from four cardinal symptoms, he also mentions secondary symptoms and the term “reflectory trophoneurosis”. This pain syndrome thus can justly be called Sudeck’s dystrophy or Sudeck’s disease, a term only rarely found in Anglo-American literature. In French literature it has been called “algodystrophie reflexe” (Bircher 1981) and in English literature “reflex sympathetic dystrophy” (RSD, Lankford 1993), whereas the internationally acknowledged term “reflex regional pain syndrome” (CRPS I) is used. In contrast, the causalgia first described by Mitchel et al. (1864) has since been called CRPS II. Nevertheless, we should not forget the names of both distinguished and prominent authors, and we should further on use them.
Until today, Sudeck’s dystrophy has been regarded as a “mysterious” disease. Aetiologically quite completely analysed in the meantime, but in pathogenetical aspect it was only agreed upon the fact the disease is based on a vasomotoric dysfunction of the sympathetic nerve system (Leriche 1923; Lankford 1993).
Though local results of this dystrophy already received extensive scientific and clinical examination, still the question remains why identical outer conditions lead to the disease in one patient, at the same time sparing another patient. Only a so-called individual predisposition for Sudeck’s dystrophy has been found in literature as hypothesis for this striking fact (Blumensaat 1956) or the “incalculable phenomenon” as postulated by Hackethal (1958).
An elevated sympathetic activity prior to the start of dystrophy can be evaluated as a predisposing factor, found in diligent examination of the upper extremity, especially in diverse pain localizations, trigger points and disturbances of sensibility. A satisfactory solution of these problems is, however, not given. Searching for further predisposing factors, parallels to the symptoms of a “thoracic outlet syndrome” (TOS) were found. Thus, the application of diagnostic tools used for TOS made sense in Sudeck’s dystrophy as well. This is especially true for the functional phlebography of the subclavian vein, since both diseases are characterised by edema, among others (Wilhelm and Wilhelm 1985).
The phlebographic examinations performed since the beginning of 1982 showed a more or less dominant impairment of venous run-off in Sudeck’s dystrophy, seen even more clearly the higher the arterial run-in is in the upper extremity Wilhelm and Wilhelm 1985.
This disturbance leads to an impairment of the venous backflow, mainly causing edema in TOS and in Sudeck’s dystrophy, also after injury and surgical procedures. Pathogenesis of idiopathic median nerve compression is also based on edema, as histologically shown in the meantime, and also proved by postoperative results (Wilhelm and Wilhelm 1985; Fig. 5.1).
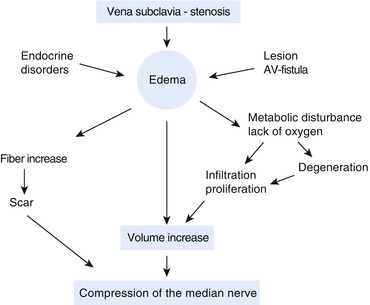
Fig. 5.1
Schematic presentation of aetiology and pathogenesis of median compression caused by edema (ideopathic). (From Wilhelm and Wilhelm 1985, with kind permission from Thieme)
Improvement rates in median compression after surgical treatment of TOS are 81 % (64 out of 79 cases (Chap. 5, Table 5.2).
Phlebographic proof of subclavian vein stenosis also found in Sudeck’s dystrophy is the “second key” (Lankford 1993) being searched for all over the world for solution of this disease.
5.2 Surgically Relevant Anatomy and Physiology
Transaxillary decompression of the nerve-vessel bundle originally developed and described by Roos (1977) for the treatment of thoracic outlet syndrome is also used for the treatment of therapy-resistant dystrophy with the precondition of exact knowledge about the anatomy of the axillary region.
According to von Lanz and Wachsmuth (1959), the axillary region in an abducted arm is a four-sided pyramid with its peak behind the middle of the clavicle. The shape of this pyramid changes depending on arm position. Its floor is the axillary fascia.
Superficially the major pectoral muscle and in the depth the minor pectoral muscle and the subclavian muscle constitute the front wall of the axilla. The back wall consists of three muscles, being the subscapular, the teres major and the latissimus dorsi muscle, whereas the medial wall of the pyramid consists of the lateral serratus muscle and the convex thoracic wall below. The lateral wall is the most narrow one, only developed at the base of the pyramid. The inner side is bordered by the coracobrachial muscle, the short head of the biceps muscle, as well as the humerus.
Muscles of the front and the back wall meet at the shoulder joint; thus, the pyramid at its peak is only bordered on three sides.
If the axillary fascia is cut at the 3rd costa in vertical direction, you find the thoracoepigastric vein and its lymphatic vessels in the middle part of the superficial axillary filling tissue layer and medially the lateral thoracic vessels. The thoracodorsal nerve and its vessels are found in a deeper layer at the upper rim of the dorsal latissimus muscle. In further preparation, you reach the lateral serratus muscle in the depth and above it laterally and vertically the long thoracic nerve.
The intercostobrachial nerve with its fibres branching from the intercostal nerve II and III (Fig. 5.25) is found in further proximal direction at the height of the middle axillary line.
The superior thoracic vessels are situated in further laterocranial direction, running into the first intercostal space and coming from the lower side of the subclavian vessels. After ligature and cutting of the superior thoracic vessels and extension of the arm in abduction, you see the first costa and above it the vessels leading to the arm as well as the brachial plexus. In the anterior area of this region, internationally called thoracic outlet, there is a strikingly tendinous origin of the subclavian muscle from the bone-cartilage border of the 1st costa, grasping the subclavian vein in bow shape at the lower and frontal side (Fig. 5.25). This muscle inserts at the lower side of the clavicula, and it can compress the subclavian vein also from cranial direction if developed strongly. Behind the subclavian vein the anterior scalene muscle is situated. It divides the subclavian vein from the subclavian artery. The originating portion of this muscle can be tendinous at the back rim but also at the entire width, in functional stress of the shoulder joint leading to an irritation of the subclavian artery and the sympathetic fibres running peripherally, coming from the stellate ganglion (Figs. 5.25 and 5.27).
Usually the brachial plexus (C4–Th 1) runs next to the subclavian artery in the gap bordered by the anterior and medius scalene muscles, called hiatus scalenorum. Division of both structures is frequently accomplished by the minor scalene muscle or its ligamentary rudiment. These structures can also lead to irritation (Fig. 5.25).
The minor scalene muscle normally arises from the transverse process of the 7th cervical vertebra connecting at the inner side of the 1st costa. Its origin can additionally reach up to the height of the 5th vertebra. The relatively broad muscle in this case sometimes connects with the cupula pleurae as the so-called scalenopleural muscle (Fig. 5.2).
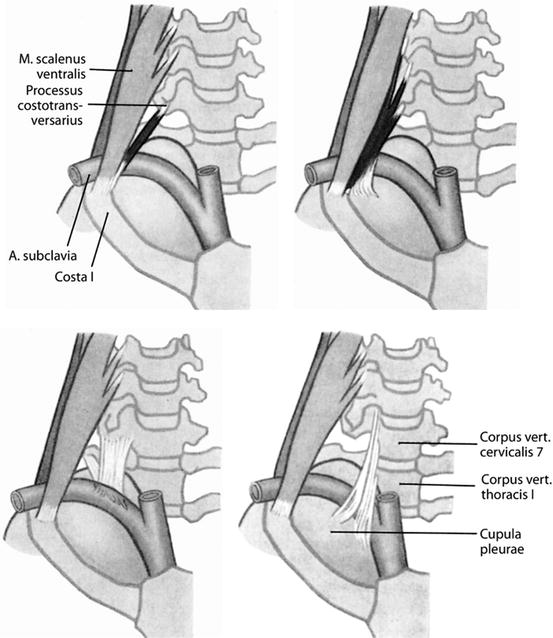
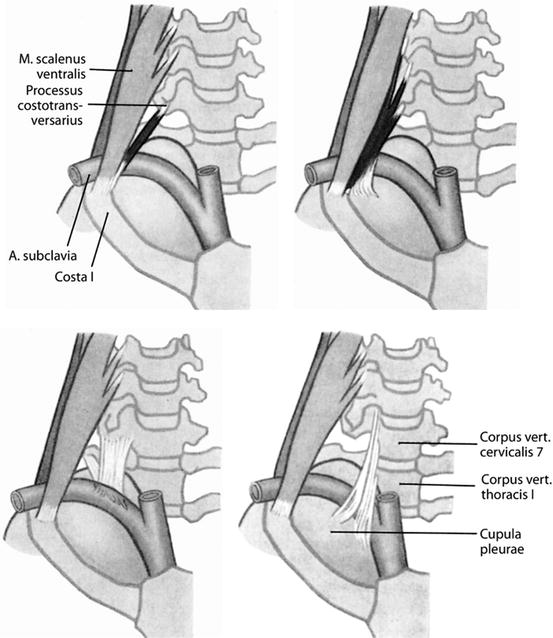
Fig. 5.2
Varieties of scalenus minimus muscle and pleurovertebral ligament. (From von Lanz and Wachsmuth 1955)
Retaining ligaments coming from the side of the cervical vertebra can also start behind the subclavian artery. Sometimes they radiate in front of the subclavian artery as pleurovertebral ligament, hindering the vessel. Most frequent special cases of the minor scalene muscle and the pleurovertebral ligament are compiled in Fig. 5.2 .
The anterior scalene muscle comes from the 3rd to the 6th, the median scalene muscle even from the 2nd to the 7th transverse process. Behind the median scalene muscle, there is the posterior scalene muscle arising from the transverse processes of the 4th–6th cervical vertebrae and in contrast to the muscles mentioned before only connecting to the 2nd costa.
In preoperative presentation of the anterior scalene muscle according to von Lanz and Wachsmuth (1955), seven varieties are found:
1.
The muscle can be missing altogether, also together with both other scalene muscles.
2.
The muscle can connect to the 1st costa behind the subclavian artery melted with the median scalene muscle.
3.
Even if there is a scalene hiatus, the subclavian artery can perforate and split the muscle.
4.
The muscle can also originate from long neck costae.
5.
The anterior scalene muscle can exchange its bundle of origin with the median scalene muscle.
6.
The origins can be tightly connected to the intertransverse muscles.
7.
If the minor scalene muscle is missing, it might be replaced by a band-like structure coming from the costotransversal process of the 7th cervical vertebra or from the neck of the 1st costa as pleurocostal ligament, then connecting at the site of the cupula pleurae.
Most of the structures mentioned can only be seen after dissociation of the anterior and median scalene muscles from the 1st costa.
Resection of the 1st costa is necessary in order to exactly judge the conditions at the cupula pleurae, simultaneously decompressing the nerve-vessel bundle. Here the parietal pleura is additionally protected by a loose membrane from the chest wall (so-called endothoracic fascia). This fascia is also additionally secured at the cupula pleurae by a suprapleural membrane, also called Sibson fascia.
If developed strongly, this membrane can lead to compression of the subclavian vein in posterior-anterior direction (Fig. 5.10) and, in enclosure of the internal thoracic vessels and the phrenic nerve, even lead to a stripe-shaped stenosis of the vessel (Fig. 5.12).
The topographic anatomic findings at the back wall of the subclavian vein and the structures behind it in the upper thoracic opening can only be seen after blunt loosening and pushing down the cupula pleurae.
The phrenic nerve (C3–5) runs along the frontal area of the anterior scalene muscle (leading muscle!), crossing the origin of the internal thoracic artery and then normally running medial of this vessel at the back part of the subclavian vein into the upper thoracic aperture. There are diverse variations to be noticed. Rarely the phrenic nerve can run along the front side of the subclavian vein, or it can enclose this vessel with anterior and posterior portions. Also it can perforate the vein centrally in a button hole. Very rarely there is an additional (side) phrenic nerve coming from C8 and Th1, connecting with the main stem of the phrenic nerve below this vessel. A side phrenic nerve is found in 10 % (von Lanz and Wachsmuth 1955).
There is an open view of the upper thoracic vertebra, after having taken into account the anatomic topographic conditions of the upper thoracic aperture and loosening pushing down the cupula pleurae until below the subclavian vein. After removing the filling tissue, there is the upper sympathetic thoracic bundle with its communicating branches and ganglia, stored in the lamellae of the prevertebral fascia.
Regularly there is a caudal cervical ganglion, frequently melted with the first thoracic ganglion into a relatively large irregular starry shaped structure, the stellate ganglion. It is found in a dimple between the transverse process of the 7th cervical vertebra and the neck of the 1st costa (Fig. 5.3, von Lanz and Wachsmuth 1959).
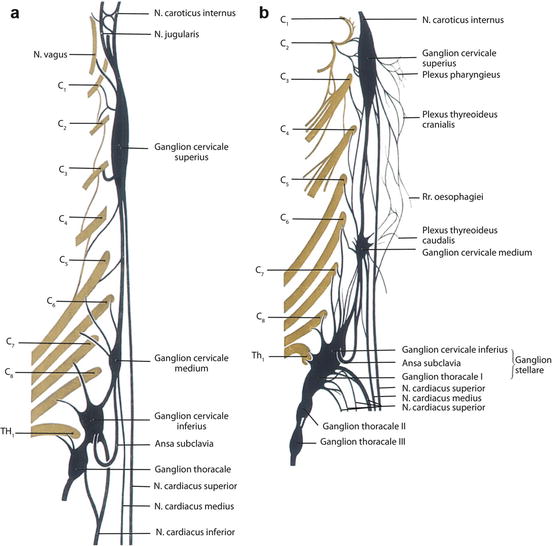
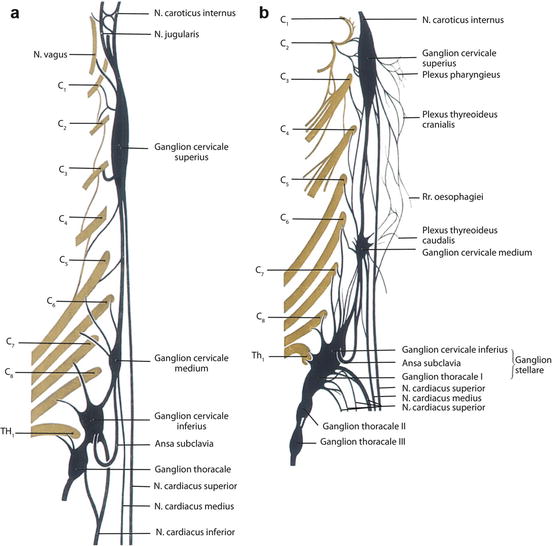
Fig. 5.3
(a) Inferior cervical and thoracic ganglion not melted, (b) inferior cervical ganglion and thoracic ganglion melted into stellate ganglion. (From von Lanz and Wachsmuth 1955)
It is easier to first look for the 3rd or 2nd thoracic ganglion and put it in a rubber band or cut and then dissect it further in cranial direction. In a stellate ganglion not only the communicating branches but also the fibres of the inferior cardiac nerves should be dissected in order to preserve them if there is a sympathetic resection by resection of the stellate ganglion inferior part. This is not always possible in an isolated ganglion T1 (Fig. 5.3). In order to be complete, it needs to be mentioned that the stellate ganglion provides a quite strong branch to the subclavian artery surrounding it in peripheral direction in plexus shape. A stronger branch innervates the coracoid region and the subcoracoid space (Wilhelm 1958; 1972).
5.3 Epidemiology
CRPS I is most frequently found after surgical treatment and after trauma of the upper extremity, independent of its severity. As already known, an abnormal sympathetic activity is the cause (Leriche 1923).
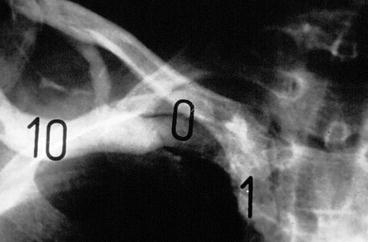
As second key giving a clue for pathogenesis, we found a disturbance of venous flow at the subclavian vein, also shown in phlebography (cf. 5.4, Figs. 5.5, 5.9, 5.10, 5.11, 5.12, 5.13, 5.14, 5.15, 5.16, 5.17, 5.18 and 5.19). Venous stenosis without simultaneous sympathetic hyperactivity only leads to a hand-finger syndrome (Figs. 5.5 and 5.6).
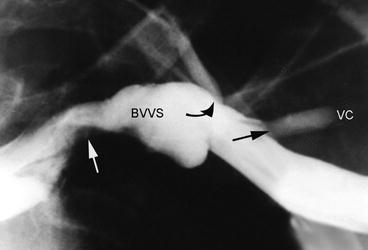

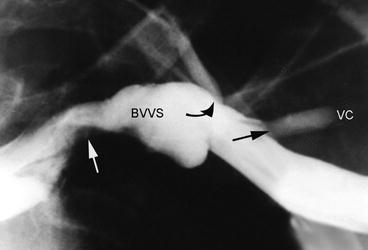
Fig. 5.5
Functional phlebography of left subclavian vein with 80 % stenosis (white arrow) and collateral blood flow (bended arrow) and reflux into the cephalic vein (VC, black arrow). BVS valvular bulb of subclavian vein. (From Wilhelm and Englert 1989, with kind permission from Thieme)

Fig. 5.6
Hand edema due to stenosis of subclavian vein after surgery for Dupuytren contraction. (From Wilhelm and Englert 1989, with kind permission from Thieme)
The incidence of this dystrophy is hard to judge as mainly minor and milder atypical forms are not immediately recognised and diagnosed.
Further on edema, damage by immobilisation and also artefacts are falsely interpreted as dystrophy.
In literature the risk of suffering from CRPS I is estimated to range between 0.05 and 5 % (according to Bär et al. 2002).
Algodystrophy is far more frequently found in females, the dominant arm being affected slightly more. This dystrophy can also occur bilaterally in rare cases. The existence of a bilateral subclavian vein stenosis is responsible. In severe dystrophy there might also be slighter symptoms.
A striking increase of this dystrophy in typical radial fracture has been analysed by now. There is a further pathogenetic factor being the compression of the deep radial branch by the supinator arcade under tension in immobilisation in forearm pronation (Werner 1979).
Family history of frequent CRPS I has also been solved pathogenetically. The cause is a disturbance of sympathetic function and a stenosis of the subclavian vein with impairment of venous flow. These factors are inheritable, whereas trauma only triggers CRPS I.
5.4 Aetiology and Pathogenesis
Aetiology is still seen as an unsolved problem, even though the significance of an elevated sympathetic tonus has been known as a neural cause since Leriche (1923). The same is true for triggering and favouring factors.
Strikingly the development of dystrophy does not depend on the severity of trauma; on the contrary, this disease often develops after minor injuries, such as contusions of the hand or shoulder region or contortions, the delayed course until the complete expression of dystrophy often lasting 1–3 months, thus diagnostically judged only sophistically in the initial phase. First increase of edema and impairment of hand function are diagnosed (Table 5.1).
Table 5.1
CRPS I (1984–1991 and 2000–2002): cases resistant to therapy
Pat. no. | Triggering causes | Pat. no. | Triggering causes |
|---|---|---|---|
1 | Radius fracture | 11 | Radius fracture |
2 | Tennis elbow | 12 | Crush injury |
3 | Shoulder contusion | 13 | Fracture MC II |
4 | Hand contusion | 14 | Bowling |
5 | Surgery of scaphoid bone | 15 | Rupture extensor tendon |
6 | Radius fracture | 16 | Radius fracture |
7 | Palmar phlegmon | 17 | TE surgery, according to Hohmann |
8 | Fracture MC II–IV | 18 | TE surgery, according to Hohmann |
9 | Hand contusion | 19 | Sudoriparous abscess |
10 | Cut | 20 | r/o scaphoid bone fracture |
The frequency of CRPS I is striking in radial fracture, where mainly pressure damage by plaster cast is accused. Remember the fact that in the immobilisation of fracture in pronation according to findings concerning pathogenesis of tennis elbow, the deep branch of the radial nerve is under permanent pressure by the supinator arcade, being 40–50 mmHg according to the findings of Werner (1979). This pressure suffices to cut off the intraneural blood flow and the axonal flow, resulting in pain afferences.
These dystrophies also occur frequently after arthroscopy (2.3 %) of the wrist and after median decompression, in 5 %, being a milder form of reflex dystrophy. Inflammatory processes, especially at the hand, can cause dystrophy (Figs. 5.36 and 5.37). Further predisposing and triggering factors are foramen stenosis at the lower cervical spine and cervical disk prolapse. Iatrogenous causes are also paravascular injections of contrast media, cytostatics, other medications and the accidental injection into a nerve, for example, the median nerve. Predisposing factors in internal medicine are hemiplegia and predominantly myocardial infarction.
The proof of the “second key” (Lankford 1993) was the missing link for the solution of CRPS I pathogenesis.
First hints were found in the beginning of the 1980s in the shape of a phlebographic proof of subclavian vein stenosis (Wilhelm and Wilhelm 1985), finally responsible as the supraordinate cause of a peripheral vascular disturbance.
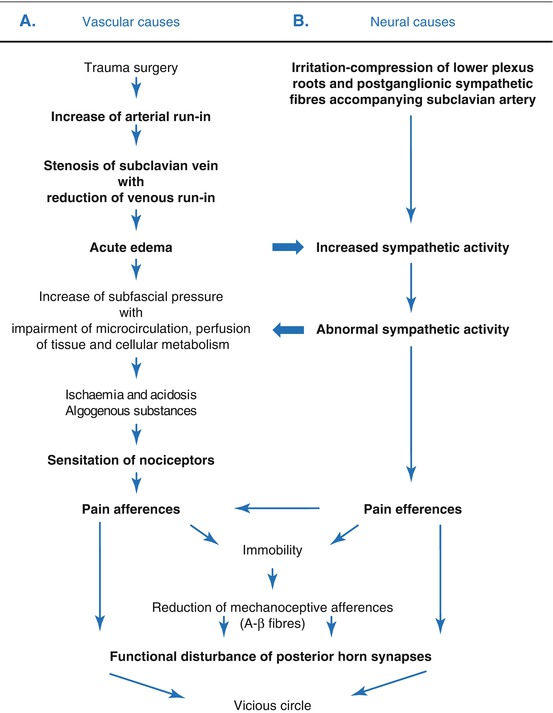
In simplified presentation pathogenesis of Sudeck’s dystrophy is essentially based on a superior vascular and neural cause (Fig. 5.4). First hints at the significance of an impairment of venous run–in for this dystrophy were already described by Sudeck in 1931 as a result of a femoral vein thrombosis.
In the meantime it was detected that the primary cause of painful edema is not found at the hand, where up to now an impairment of venous run-in, caused by sympathetically regulated tightening of venules, but further proximally at the upper thoracic aperture in form of a subclavian vein stenosis. The venous run-in is already more or less impaired depending on the amount of run-off disturbance, resulting in venous stasis and then in acute edema by sudden increase in arterial run-in after trauma and surgical procedures, finally leading to an increase in subfascial pressure (Grünert 1993).
Results of edema only lead to abnormal sympathetic reaction if prior to the start of the disease the patient already had an increased sympathetic activity.
Apart from central mechanisms causes are mainly irritations and compressions of the lower plexus roots by the inner rim of the 1st costa, by fibromuscular structures as well as by the postganglion sympathetic fibres accompanying the subclavian artery.
Abnormal sympathetic activity then, due to vasoconstriction, leads to further deterioration of microcirculation, perfusion of tissue and cell metabolism already worsened by edema. The results are ischemia and acidosis, and as an effect of the algogenic agents that develop, it leads to an increase of irritability of nociceptors with consecutive increase of pain afferences.
Sudeck’s dystrophy manifests as soon as the sum of pain afferences and efferences leads to an “overstress” and to immobilisation with resulting reduction of pain-inhibiting mechanoceptive afferences. A “vicious circle” results (Zimmermann and Handwerker 1984).
Now both of the most important causal factors of SD are known and can be localised and documented by phlebography and arteriography. The so-called individual predisposition for Sudeck’s dystrophy (Hackethal 1958) then is primarily based on an impairment of venous run-off at the subclavian vein, resulting in a disbalance of arterial run-in and venous run-off at a simultaneously elevated sympathetic activity. In a normal sympathetic regulation of reflexes, venous stenosis under identical external conditions (surgery, trauma, etc.) only leads to an edema of the hand. Figures 5.5 and 5.6 show an example.
Finally Sudeck’s dystrophy can be calculated by the introduction of functional phlebography, being significant not only in forensic and legal (insurance) respect.
Taking into account the anatomic, topographic and pathophysiologic facts, SD might be interpreted as the most severe presentation of TOS and TIS.
5.5 Diagnostics
Diagnostic judgement on a therapy–resistant dystrophy depends on exact anamnesis, also focusing on predisposing causes, such as surgical procedures; injuries at work, in sports, traffic or accidents at home; inflammatory process; and cardiac disease. The development of the disease from the view of the patient, the duration of the symptoms and the kind of treatment received are important. It has to be found out whether the patient is sufficiently treated with pain medication or whether medication is only provided on demand, as this is essential for the prognosis of the disease. Invasive procedures as acupuncture, blockades of the brachial plexus and the stellate ganglion and i.v. regional blockades with guanethidine (Hannington-Kiff 1977) have to be inquired about as well.
5.5.1 Tabular Documentation of Pathologic Findings at the Upper Extremity
In order to compile a complete evaluation of all pathologic findings at the shoulder girdle, the region of the elbow and the forearm as well as the hand and to document the important preoperative findings essential for follow-up, the development of a tabular documentation is highly recommended (Fig. 5.7). It should include all pain localizations, neurological findings and other results of examination, such as articular function, comparing circumferences, examination of the volume of both hands (dip test) and the venous run-in pressure. Apart from colour of the skin and temperature and also strength and the extent of edema, different qualities of pain including allodynia and results of different tests and sympathetic block should be documented.
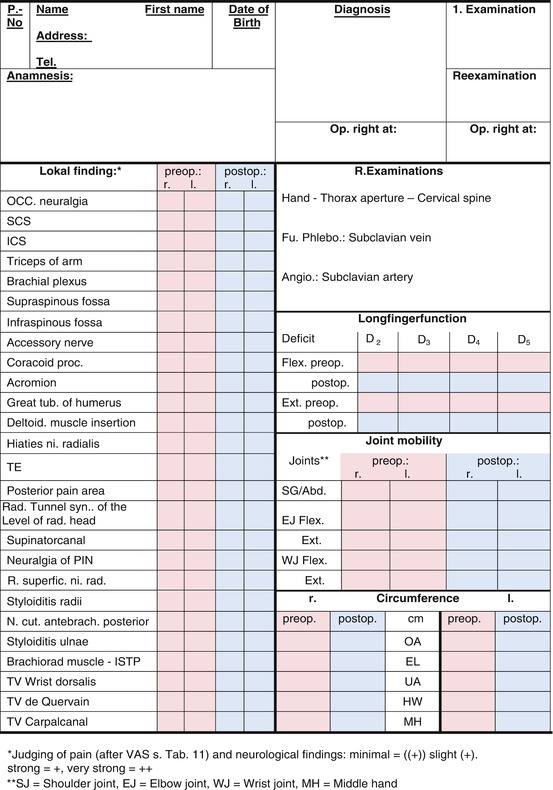
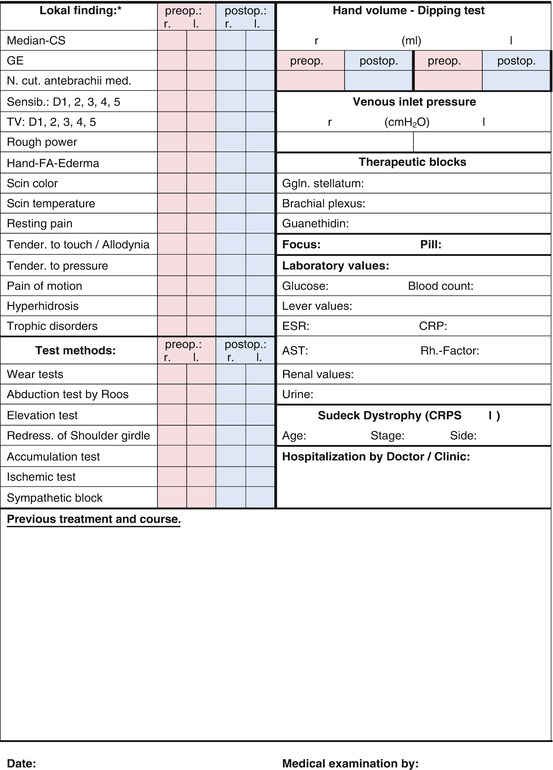
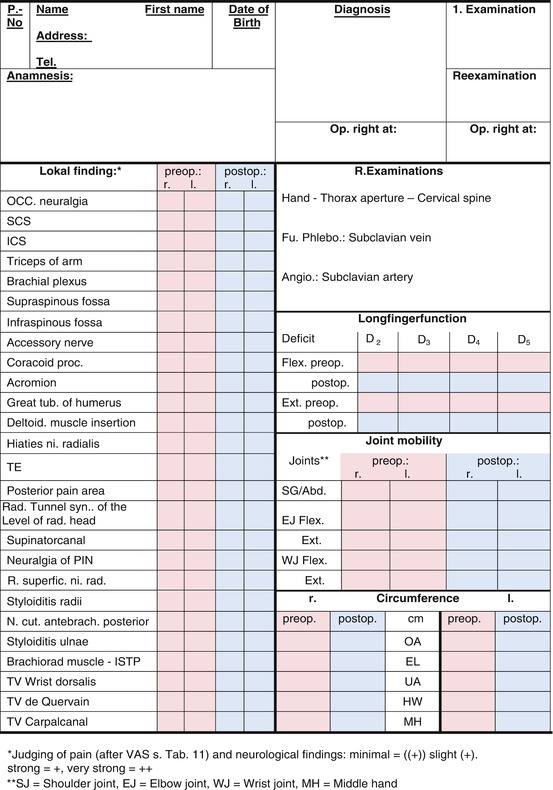
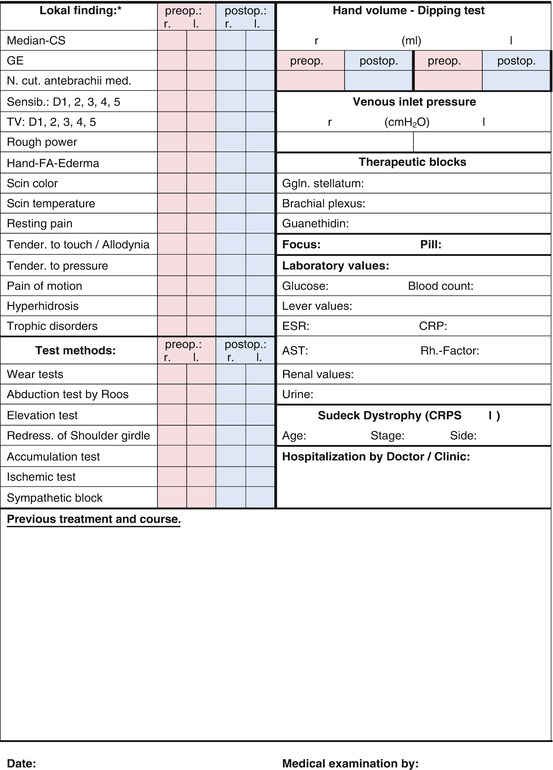
Fig. 5.7
Examination sheet for patients with TOS and CRPS I
In acute dystrophy with strong pain, the test for damming and ischemia should only be performed exceptionally if essential for diagnostic reasons. For determination of stadium II and III of dystrophy, these examination methods are advisable.
The diagnosis of a neurogenous origin of Sudeck’s dystrophy needs a diligent systematic examination of the upper extremity including the neck region. The most important examination results and the corresponding postoperative findings are presented in Tables 5.2, 5.3 and 5.4.
Table 5.2
CRPS I (1984–1991): shoulder girdle
Preoperative findings | n | Postoperative results | |||
|---|---|---|---|---|---|
N P = 10 – follow-up – N OP = 10 | Excellent | Good | Fair | Unchanged | |
Occipital headache | 4 → | 2 | – | 1 | 1 |
Upper cervical syndrome | 5 → | 3 | – | 2 | − |
Lower cervical syndrome | 8 → | 5 | 1 | 1 | 1 |
Trapezius muscle | 9 → | 6 | 2 | 1 | – |
Brachial plexus | 9 → | 5 | 3 | 1 | – |
Supraspinous fossa | 2 → | 2 | – | – | – |
Infraspinous fossa | 4 → | 3 | – | – | 1 |
Accessory nerve | 3 → | 2 | – | – | 1 |
Coracoid process | 6 → | 3 | – | 2 | 1 |
Acromion | 3 → | 3 | – | – | – |
Greater tuberosity of humerus | 6 → | 4 | 2 | – | – |
Deltoid muscle insertion | 4 → | 3 | 1 | – | – |
Total | 63 = 100 % | 41 = 65.1 % | 9 = 14.3 % | 8 = 12.7 % | 5 = 7.9 % |
Table 5.3
CRPS I (1984–1991): elbow and forearm
Preoperative findings | n | Postoperative results | |||
|---|---|---|---|---|---|
N P = 10 – follow-up – N OP = 10 | Excellent | Good | Fair | Unchanged | |
Radial tunnel—proximal part | 3 → | 2 | 1 | – | – |
Radial tunnel—intermediate part | 9 → | 4 | 3 | – | 2 |
Radial tunnel—distal part | 9 → | 3 | 3 | 1 | 2 |
Lateral epicondylitis | 10 → | 4 | 3 | 1 | 2 |
Interosseous neuralgia | 7 → | 4 | 1 | 1 | 1 |
Radial styloiditis | 7 → | 5 | 2 | – | – |
Medial epicondylitis | 1 → | 1 | – | – | – |
Medial cutaneous nerve | 3 → | 2 | 1 | – | – |
Ulnar styloiditis | 4 → | 3 | 1 | – | – |
Brachioradialis muscle insertion | 6 → | 3 | 2 | 1 | – |
De Quervain disease | 3 → | 2 | – | 1 | – |
Total | 62 = 100 % | 33 = 53.2 % | 17 = 27.4 % | 5 = 8.1 % | 7 = 11.3 % |
Table 5.4
CRPS I (1984–1991): hand
Preoperative findings | n | Postoperative results | |||
|---|---|---|---|---|---|
N P = 10 – follow-up – N OP = 10 | Excellent | Good | Fair | Unchanged | |
Trophic and secretory disturbance | 10 → | 5 | 3 | 2 | – |
Hand edema | 10 → | 8 | 2 | – | – |
Increased | 6 → | 6 | – | – | – |
Skin temperature | |||||
Decreased | 4 | 1 | 2 | 1 | – |
Sensory disorders | 10 | 6 | 4 | – | – |
Tactile pain | 5 → | 3 | 1 | 1 | – |
Palpation pain | 10 → | 8 | 1 | 1 | – |
Pain on movement | 10 → | 8 | 2 | – | – |
Rest pain | 10 → | 8 | 2 | – | – |
Decreased | 5 → | 2 | 1 | 2 | – |
Crude strength | |||||
Not examined* | 5 → | 2 | 1 | 2 | – |
Median nerve compression | 7 → | 4 | 2 | 1 | – |
(No. 3, 4 and 7 not examined) | 3 → | 2 | 1 | – | – |
Soft tissue atrophy | 1 → | – | 1 | – | – |
Bone atrophy | 9 → | 5 | 3 | 1 | – |
Total | 106 = 100 % | 68 = 64.1 % | 26 = 24.5 % | 11 = 10.4 % | 0 |
Mainly in peripheral nerve compression syndromes and out of reasons of differential diagnostics, there is an indication for neurological examination.
In order to confirm the diagnosis in any case after finishing the examinations, a sympathetic block as stellate or plexus anaesthesia with naropine should be performed, at the same time demonstrating the possible extent of a pain elimination by transaxillary decompression of the neurovascular bundle by additional sympathetic resection. X-rays of the hand in two levels and of the lower cervical spine in a.p. and half oblique are necessary as a standard. Here decalcifications of the hand bones and possible foramen stenoses can be seen. Special pictures of the upper thoracic aperture are important for surgery in order to see a cervical rib, an unusually long transverse process of the 7th cervical vertebra and a steep position or a hypoplasia of the 1st costa on time, as these structures might promote a compression of the brachial plexus and the subclavian artery.
A cervical rib or its fibrous and cartilaginous insertion at the first rib can even reduce the posterior scalenus gap leading to a shifting of the brachial plexus and the subclavian artery. A relieving high shoulder position already clinically hints at a cervical rib. Figure 5.8 gives a survey on varieties of cervical rib development.
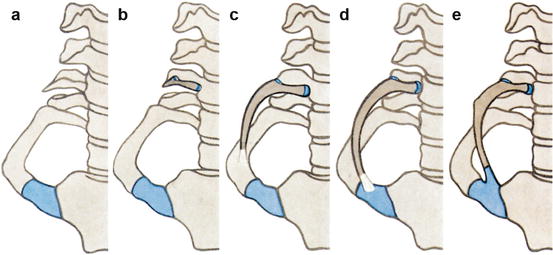
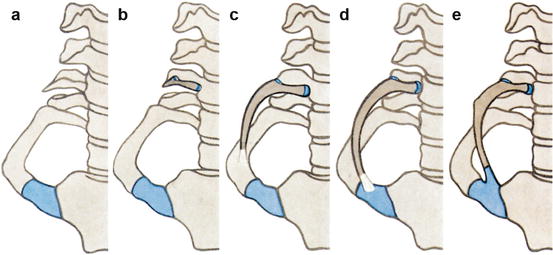
Fig. 5.8
(a) Varieties of cervical ribs, unusually long transverse process of the 7th cervical vertebra. (b) The front section of the costotransverse process forms a rib brace, connected to the transverse process and the vertebra. (c) The rudimentary cervical costa exceeds the transverse process ending free; only in 5 % there is a connection to the first costa. (d) The cervical costa reaches the 1st costa in fibrous, cartilaginous or osseous manner. (e) The cervical costa behaves like a thoracic costa. It reaches the sternal manubrium by its cartilage melted with the 1st costa. (From von Lanz and Wachsmuth 1955)
Three-phase bone scintigraphy can be a helpful tool at the initial state I of the disease, but it is not specific! Other diseases as well can cause an accumulation in bone scan, like, for instance, inflammatory, infectious and tumour processes. But above all, this examination method cannot provide reliable information concerning prognosis, and it also cannot show whether the patient is suitable for a conservative or rather for a surgical therapy.
As the symptoms of Sudeck’s dystrophy are strikingly similar to those of TOS, a functional phlebography, as obligatory in this syndrome, was also introduced as a diagnostic tool in Sudeck’s dystrophy to check the conditions of run-in at the subclavian vein in this disease as well, hoping to find a logical explanation for the acute edema in this dystrophy.
In this disease functional phlebography is performed considering the pain limit in adduction and abduction of the arm, if possible in 0–60–0° in lying or sitting position. Pictures in elevation are not essential in Sudeck and should be avoided due to the strong pain connected.
Ultravist 300 is used as contrast medium in a bolus of 30 ml/contrast series.
Injection follows after the application of a tourniquet into the basilica vein in order to not endanger the judgement of reflux into the cephalic vein in an essential disturbance at the subclavian vein.
In 25 out of 26 patients with resistant dystrophy surgically treated by the author, a striking impairment of the venous run-in at the subclavian vein with reflux into the cephalic vein and in massive changes also in combination with a collateral circle was seen in phlebography.
The venous stasis can be determined numerically by measuring the venous run-in pressure in the sitting patient (Dunant 1987). First the pressure in the axillary vein compared to the level of the atria is determined using an infusion machine for saline solution. After pushing forward the catheter pressure conditions at the subclavian stenosis and finally of the brachiocephalic vein are determined. Here prestenotic pressures up to 35 cm H2O can be found if a collateral circle is missing, whereas pressure can fall down to 0 cm H2O in the stenotic area. Pressures in the upper vena cava in a healthy patient are up to −3 cm H2O and below. In a massive collateral circle, even a lower pressure of run-in can be found (Fig. 5.9). There also is a slighter hand edema in these cases.