Consider Acupuncture as an Adjunct for the Prophylaxis and Treatment of Postoperative Nausea and Vomiting
Leena Mathew MD
Unfortunately, postoperative nausea and vomiting (PONV) is still a common side effect of anesthesia despite the availability of newer-generation antiemetics and shorter-acting anesthetics and opioids. PONV is one of the two most significant factors leading to patient dissatisfaction (the other, of course, being pain). The incidence of PONV is approximately 70% in those patients who are at high risk for this complication and 30% in the general population. Even though postoperative vomiting is self-limited, it can cause significant morbidity, including dehydration, wound dehiscence, aspiration, and electrolyte imbalance. PONV also increases costs since each episode of emesis in the postanesthesia care unit (PACU) delays discharge by an average of 20 minutes.
The following factors place a patient at high risk for PONV:
Patient-related factors: Female, nonsmoking, dehydrated, and with prior episodes of PONV.
Procedure-related factors: Ear, nose, or throat surgery, intra-abdominal surgery, laparoscopic surgery, strabismus repair, and obstetric or gynecologic surgery. A 30-minute increase in the duration of surgery increases the baseline risk for PONV by 60%. Any surgical procedure needing large fluid administration can cause gastrointestinal edema, which can also increase the incidence of PONV.
Anesthesia-related factors: The use of volatile agents, nitrous oxide, neostigmine (more than 2.5 mg) and long-acting opioids.
At present, the most common modalities for the prophylaxis and treatment of PONV include ensuring adequate, but not excessive, hydration; avoidance of risk factors; and the use of pharmacologic agents, such as metoclopromide, dexamethasone, and 5 HT 3 antagonists. Acupuncture is an additional approach that shows great promise in prophylaxis and treatment of PONV. In 1997, a National Institutes of Health Consensus Development Panel on acupuncture reviewed the available evidence from randomized controlled trials and concluded that clear evidence indicates that needle acupuncture is efficacious for postoperative and chemotherapy-related nausea and vomiting and probably also for pregnancy-related nausea.
Americans are now spending approximately $27 billion annually on complementary and alternative medical treatments. Statistical reports published as early as 1997 suggest that visits to complementary practitioners outnumber those to conventional practitioners by 12 to 1. Acupuncture is only one of many complementary and alternative modalities, but it is one that is already somewhat familiar to patients. A great degree of integration exists between “standard” medical techniques and acupuncture in the East, especially in China, and there is now a growing recognition of the need for such integration in the Western health system.
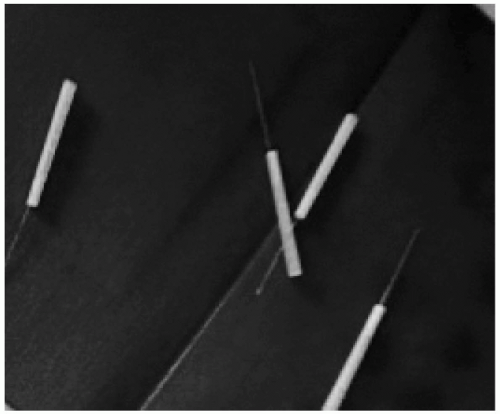
To review briefly, acupuncture is accomplished by stimulating acupoints. There are 14 major meridians corresponding to internal organs, along which there are a total of 365 acupoints. Acupuncture involves the placement of fine, disposable, stainless-steel needles (Fig. 113.1) at select acupuncture points. Acupuncture needles range from 1/4 inch to several inches in length and a few thousandths to several thousandths of an inch in diameter. One inch and 1.5 inch are the most commonly used lengths of needle. The vast majority of needles used in the United States are of stainless steel; however, copper, gold, and silver also are used. The placement of needles is followed by a stimulation technique done to the needle to elicit a characteristic sensation called De Qi. Stimulation is usually done by manual twirling or electrical stimulation but can also be done by laser or by moxibustion. Moxibustion involves the burning of fine herbs to apply gentle heat at the free end of the
needle. The choice of specific needle stimulation technique depends upon the therapist’s experience, preference, and patients’ concerns and condition.
needle. The choice of specific needle stimulation technique depends upon the therapist’s experience, preference, and patients’ concerns and condition.
Manual acupuncture involves manipulating the inserted needles by lifting, thrusting, twisting, twirling, or doing other complex combinations. It is a traditional method of acupuncture and is most commonly used in clinical practice.
Electroacupuncture (EA) is achieved by attaching the acupuncture needles to an electrical-pulse generator and stimulating the acupoints with electrical pulses. EA appears to be more consistent and to generate more reproducible results, and it is more efficacious than manual acupuncture. The procedure for EA is to insert the acupuncture needle as would normally be done, attain the De Qi reaction by hand manipulation, and then attach an electrode to the needle to provide continued stimulation. The benefits of using electrical stimulation are absence of prolonged hand maneuvering, reduction of total treatment time by providing continued stimulus, and better control of the frequency of the stimulus. It can also produce a stronger stimulation, without causing the tissue damage associated with twirling and lifting the needle.

Full access? Get Clinical Tree