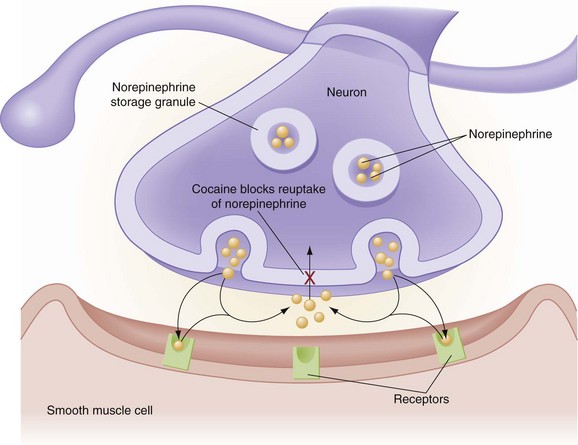
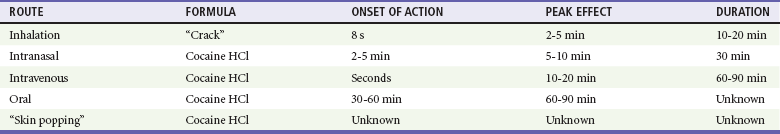
Chapter 154 Cocaine, a naturally occurring plant-derived alkaloid, has been used for centuries as a medicinal product. For thousands of years in South America, the leaves of the coca plant (Erythroxylon coca) have been chewed for treatment of various ailments. In 1860, the pure alkaloid form was isolated and became a popular constituent of various beverages, pharmaceuticals, and therapeutic tonics, but it was banned from these products in the United States in 1914. At the peak of the cocaine epidemic in the early 1990s, it was estimated that 5 million people used cocaine regularly in the United States.1 The drug is still popular, with up to 1.6 million current users of cocaine reported as of 2009.2 This is a decrease from 2.3 million users in 2003,3 but the consequences of recreational cocaine use are still profound. Cocaine is implicated in violent deaths and was detected in 25% of autopsies of fatal injuries in adults aged 15 to 44 years.4 In 2009, 39% of drug misuse deaths were due to cocaine.5 According to the Drug Abuse Warning Network, there were more than 423,000 cocaine-related emergency department (ED) visits representing 52% of drug abuse or misuse cases.6 As of 2009, cocaine ranked within the top three causes of illicit drug–related deaths at various cities across the United States.7 Amphetamines are stimulants originally designed for use as decongestants and dietary aids that became popular as recreational drugs in the mid-20th century. By modification of the amphetamine molecule, illicit “designer” amphetamines are inexpensively produced. The enhanced effects from these alterations add to the popularity of drugs such as 3,4-methylenedioxymethamphetamine (MDMA) and methamphetamines. Cocaine, amphetamines, and derivatives of amphetamines are called sympathomimetics (Box 154-1). These agents cause central nervous system (CNS) stimulation and a cascade of adrenergic physiologic effects. As of 2009, there were 502,000 methamphetamine current users in the United States.2 Acute cocaine use causes release of dopamine, epinephrine, norepinephrine, and serotonin. These neurotransmitters act on different receptor subtypes to cause many effects, but the most important is adrenergic stimulation by norepinephrine and epinephrine (see Box 154-1). Norepinephrine causes vasoconstriction by stimulation of alpha-adrenergic receptors on vascular smooth muscle. Epinephrine increases myocardial contractility and heart rate through stimulation of beta1-adrenergic receptors. In addition to catecholamine release, the reuptake of these stimulatory neurotransmitters from synaptic clefts is inhibited, altering the normal balance between excitatory and inhibitory tone in the CNS. Subsequent stimulation propagates peripheral catecholamine release (Fig. 154-1). Reuptake of serotonin is similarly inhibited and can cause serotonergic excess as well. Cocaine also is a local anesthetic agent, slowing nerve impulses from neuronal pain fibers by blocking the inward movement of sodium across cell membranes (phase 0 of the action potential).8 Sodium channel blockade across myocardial cells, similar to the class IA antidysrhythmics, is responsible for the occasional conduction abnormality with acute cocaine toxicity. Cocaine metabolism occurs in the liver and the plasma. In the liver, the drug is metabolized primarily to the active metabolite norcocaine, which potentiates the parent drug. In the plasma, cocaine is metabolized to ecgonine methyl ester through pseudocholinesterase (plasma cholinesterase). This difference may account for the differences in duration of action with different routes of administration.9 Ecgonine methyl ester may be protective because it is a vasodilator. Genetic differences in the phenotypic expression of plasma cholinesterases may account for individual differences in susceptibility to cocaine toxicity.10 Benzoyl ecgonine, a metabolite found in the plasma, is produced primarily from nonenzymatic reactions. It is the metabolite identified by urine toxicology screens. Methylecgonidine and its metabolite ecgonidine are products of cocaine pyrolysis (crack). Although it is less commonly assayed, methylecgonidine also can be identified in the urine. The use of ethanol with cocaine forms cocaethylene, a metabolite that may potentiate the drug’s stimulatory effects and lengthen the duration of its effects.11 Unpurified cocaine paste is converted to usable forms of cocaine. The crystallized freebase of the cocaine alkaloid is known as crack cocaine. It is inhaled with use of a special “crack pipe” designed to tolerate the high temperature required to volatilize pure cocaine. The high lipid solubility and rapid transport from the lungs into the brain contribute to crack’s rapid onset of action (Table 154-1). The water-soluble salts of cocaine (cocaine hydrochloride and cocaine sulfate) are available as a white crystalline powder that is insufflated intranasally or dissolved and injected intravenously. Oral administration is rare except for patients who are smuggling or concealing drugs. Death due to acute cocaine overdose is significantly higher on days with ambient temperatures higher than 88° F.12,13 The profound diaphoresis associated with cocaine may be absent or limited in cooler environments or if the patient is excessively salt and water depleted. Acute psychomotor agitation with delirium increases the risk of hyperthermia.14 Cocaine toxic patients have increased motor tone and generate heat. Vasoconstriction and salt and water depletion can compromise cooling, resulting in life-threatening hyperthermia with core temperatures exceeding 106° F (41.1° C). Delay in recognition and management increases the likelihood of death. Even with a normal temperature, increased motor tone can release intramuscular creatine kinase, with rhabdomyolysis and its attendant renal and electrolyte complications.15 Acute cocaine-induced hypertension can seriously injure the cardiovascular system and CNS. Reported sequelae include aortic dissection,16 pulmonary edema,17 myocardial ischemia and infarction,18 intracranial hemorrhage,19 strokes,20 and infarction of the anterior spinal artery.21 Vasospasm can also compromise perfusion to various organs. Intestinal infarctions and mesenteric ischemia can occur, particularly in body packers with large oral ingestions.22,23 Other local ischemic events include retinal vasospasm, renal infarctions, and placental insufficiency and infarction in the gravid uterus.24 Although sinus tachycardia is most common, atrial fibrillation and other supraventricular tachycardias can occur as a result of the surge in catecholamines. A life-threatening dysrhythmia may not be noted until cardiac output abruptly diminishes and the patient suddenly loses consciousness. Torsades de pointes25 or wide-complex tachycardias from blockade of fast sodium channels on the myocardium may deteriorate into poorly perfusing or fatal ventricular rhythms.8 Transient conduction abnormalities consistent with a Brugada-type pattern are associated with cocaine.26,27 Hyperkalemia from rhabdomyolysis and myocardial ischemia can also cause dysrhythmias. A patient occasionally has “crack dancing,” a transient choreoathetoid movement disorder probably related to abnormalities in dopaminergic tone.28 Deep venous thrombosis is reported with cocaine use, probably secondary to effects on coagulation. Paranoia, either drug induced or from underlying psychiatric illness, may occur even after the acute effects of the drug subside. The neuropsychiatric effects of cocaine can alter behavior and judgment, increasing the risk of violent injuries. Complications also arise from the route of administration of cocaine. Inhalation of crack cocaine may cause oropharyngeal burns from the high temperature required to volatilize the drug.29 Pneumothorax, pneumopericardium, and pneumomediastinum occur from inhalational barotrauma.30 Intranasal cocaine use is associated with sinusitis and nasopalatine necrosis or perforation.31 Intravenous users have a high risk of infection with blood-borne viruses, local abscesses, and systemic bacterial infections, including botulism and endocarditis.32 Transdermal injection of cocaine, or “skin popping,” has similar types of complications, especially of skin abscesses. For a chronic user, addiction, or psychological dependence, is mediated through specific dopaminergic neurotransmitter pathways. Although there are no well-defined syndromes constituting cocaine withdrawal, patients have strong cravings for the drug or a general feeling of dysphoria that is not physiologically life-threatening.33 In 2009, as much as 69% of cocaine imported into the United States contained levamisole, a veterinary anthelmintic agent.34 Agranulocytosis, vasculitis with thrombosis, dermal ulcers, and purpura, often affecting the earlobes, occurred as a result of the unintentional exposure to levamisole.34–37 The reason for this adulteration of cocaine with levamisole is not clear. An electrocardiogram (ECG) screens for dysrhythmias and conduction abnormalities from ischemia, hyperkalemia, or, more precipitously, QRS prolongation from sodium channel blockade. This blockade slows myocardial depolarization and results in a wide-complex tachycardia. The axis may be indeterminate or have a terminal rightward axis deviation similar to cyclic antidepressant toxicity. Cyclic antidepressants and cocaine share class IA antidysrhythmic effects. Evaluation of chest pain is challenging because ST segment elevation is confounded by the presence of early repolarization.38,39 Serial ECGs may be helpful. Creatine kinase (CK), a nonspecific marker for muscle injury, is often elevated with cocaine use. The serum CK-MB fraction, troponin I, and troponin T are more specific in patients with atherogenic coronary disease but less certain in patients with cocaine-related chest pain.33,39,40 Some patients with elevations in CK-MB have normal troponin I or troponin T levels.40 Patients presenting with positive troponin I and chest pain after cocaine use have a higher incidence of angiographic findings,41 but up to 18% of patients may have normal angiograms in the setting of positive biomarkers for myocardial infarction (MI).42 Although the sensitivity and specificity of troponin and other serum enzyme markers are still being investigated for cocaine-related chest pain, cardiac enzymes should be measured as is done for other cardiac patients. Data regarding the role of coronary computed tomography angiography (CTA) to identify patients with cocaine-related coronary disease are evolving.43,44 Until it is further studied, coronary CTA cannot be routinely recommended. In the rare event that a patient presents with agranulocytosis or vasculitis suggestive of levamisole, a special laboratory evaluation for urine levamisole by gas chromatography–mass spectrometry may be requested. The sample is ideally obtained within 48 hours after last use.37 Other infectious or rheumatologic causes of this presentation should also be considered. A differential diagnosis of acute cocaine toxicity includes the many causes of agitated delirium (Box 154-2). A thorough assessment of mental status, vital signs, and physical examination can help direct and narrow the differential diagnosis. Conditions that may be indistinguishable from cocaine toxicity include sedative-hypnotic withdrawal, toxicity from amphetamines and amphetamine derivatives, and heatstroke. Phencyclidine toxicity may be distinguished by the presence of multidirectional nystagmus, but the treatment is similar. Patients with anticholinergic poisoning typically have urinary retention, dry skin, and minimally reactive pupils as distinguishing factors. Infection should be considered in all hyperthermic patients. A severely poisoned patient is combative and unable to cooperate in assessment of vital signs. Actions taken during these first stages of the encounter are crucial (Box 154-3). Because the cause of the patient’s state often is not clear, the initial priority is to recognize and treat the life-threatening agitated delirium.
Cocaine and Other Sympathomimetics
Perspective
Principles of Disease
Cocaine Formulations
Clinical Features
Hyperthermia
Hypertensive Emergencies
Cardiac Dysrhythmias
Other Complications
Diagnostic Strategies
Differential Considerations
Management
< div class='tao-gold-member'>

Full access? Get Clinical Tree