Chronic Ventilator Facilities: Introduction
Chronic ventilator facilities (CVFs) are meant to be “protected” environments for the treatment of patients who require prolonged mechanical ventilation. Numerous words are included under the umbrella of CVFs: long-term acute care facilities, respiratory special care units, chronic ventilator-dependent units, regional weaning centers, ventilator-dependent rehabilitation hospitals, prolonged respiratory care units, noninvasive respiratory care units, high-dependency units, and respiratory intensive care units. And this is without even considering nursing homes and hospice care.
A 16-year study showed that the number of acute care hospital beds in the United States has decreased over time, but the number of critical care beds has increased progressively in both absolute and proportional terms. Indeed, the total number of non–critical care beds decreased by 31%, whereas critical care beds increased by 26%1; nevertheless, admissions to an intensive care unit (ICU) are very strongly influenced by bed shortages. Most beds in an ICU are occupied by patients requiring mechanical ventilation. A subset of patients receiving mechanical ventilation may have weaning difficulties, so that the duration of ventilation may be abnormally prolonged (commonly defined as greater than 15 days). Several reports indicate that these ICU patients are affected by complex cardiopulmonary disease or multisystem problems and have a relatively poor outcome.2–6
Of 6,469,674 hospitalizations in six American states, 180,326 (2.8%) received invasive mechanical ventilation. A total of 44.6% had at least one major comorbidity condition. The most common comorbidities were diabetes (13.2%) and pulmonary disease (13.2%), and only 30.8% of patients were discharged to home from the hospital, while the others ultimately required care in a skilled care facility.7
Increased life expectancy has dramatically increased the age of patients requiring critical care. Medical ICU admission is associated with a high long-term mortality even in healthy elderly patients, while most of the oldest survivors undergo prolonged mechanical ventilation, which is often a marker not only of respiratory system insufficiency, but also a multisystems insufficiency caused by many factors, including a chronic underlying disease, infections, malnutrition, complications, invasive procedures, and medications.8,9
Prolonged mechanical ventilation is not just a “medical” problem; it also has social and economic impact. Costs for mechanical ventilation in the United States are estimated to be $27 billion, representing 12% of all hospital costs. Incidence, mortality, and cumulative population costs rise significantly with age.7 Each year in the United States, approximately 300,000 patients receive prolonged life support in an ICU, and this number is likely to double within a decade, with associated costs of more than $50 billion.10
These patients, once discharged from the ICU, have a readmission rate of 67% and spend an average of 74% of all days alive in a hospital or in an acute care facility, or receiving home health care. Indeed, patients who survive for 1 year are left with a serious burden of pervasive and persistent disability despite aggressive care that cost 306,135 $ for cohort members.11 The burden of prolonged mechanical ventilation also affects the families because of financial implications, disruption of family routine, and uncertainly of the future, as well as community financial resources. Even after these “chronically ill” patients are discharged from the ICU, which occurs once the precipitating cause of their acute episode of respiratory failure has been reversed, they still require mechanical ventilation. Thus, they either require transfer to a long-term care or rehabilitation facility.12
Rationale
At the time of ICU discharge, patients who still need dedicated care or mechanical support are usually in a phase of clinical stability, but they have several “open” problems that prevent them being transferred to a regular ward or directly to home. Several reasons justify their transfer to a dedicated CVF.
First, weaning from prolonged mechanical ventilation is a complex, time-consuming process that involves not only the selection of the best ventilation method for a particular patient, but comprehensive procedures, such as protocol-driven weaning, have the potential for improving clinical outcome through increased use of efficacious weaning methods, such as daily weaning screening, spontaneous breathing trials, and management of the ventilator and sedation.13 Rapid turnover in a busy ICU and its clinical burden does not always allow devoting the necessary time for these procedures, and discontinuation of mechanical ventilation is not always a priority.14
Second, given the nature of critical illnesses and the modalities used to manage them, prolonged bed rest, with well-known adverse physiologic effects, is the rule in the ICU. Rehabilitation has the potential to restore lost function. Yet, with few exceptions,15 it traditionally does not start until after ICU discharge. Critically ill patients are often viewed as “too sick” to tolerate physical activity in the early phase of their illness, frequently prolonging immobilization.
Third, psychiatric symptoms are quite common in chronic patients who survive an ICU stay and in their relatives at the time of ICU discharge, as well as 90 days later.16 Open visiting hours for family members and comfort among patients and caregivers may be enhanced by return to a more physiologic circadian rhythm as opposed to that found in a typical ICU. Delirium, probably the most common psychiatric problem in critically ill patients, may still occur after discharge from an ICU, albeit with a lower incidence. The environment and the strategy of care adopted in CVFs seems to positively affect the recovery from a delirious state.17
Fourth, sleep disruption is a well-documented problem during ICU stay and it persists at ICU discharge.18 Sleep deprivation can have significant consequences and has been shown to impair cognitive function, increase protein catabolism, decrease immune function, and alter respiratory mechanics that could eventually impact weaning from mechanical ventilation. A more “natural setting,” like a CVF, may minimize the number and intensity of some environmental factors, involved in the genesis of poor sleep, such as noise and light intensity.19
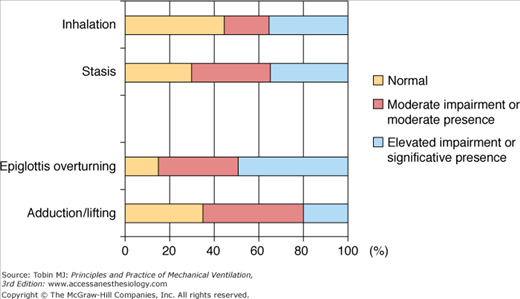
Fifth, aspiration is common in patients with tracheostomies receiving prolonged ventilation and with advanced age the risk of aspiration increases. Swallowing problems are seldom assessed with the appropriate technique (i.e., videofluoroscopy) in the ICU, and the most important specific rehabilitative therapy is rarely started. Figure 33-1 illustrates the incidence and types of swallowing dysfunction in a cohort of 188 patients admitted to a CVF after ICU discharge.
Figure 33-1
Incidence and types of swallowing dysfunction in a cohort of 188 patients admitted to a chronic ventilator facility after discharge from an ICU (Ceriana et al, unpublished data). Epiglottic overturning refers to the backward movement of the epiglottis during closure of the laryngeal vestibule. Adduction/lifting refers to the adduction of the vocal folds and movement of the larynx observed during inspection when the patient is requested to phonate and swallow.
Sixth, the number of tracheotomies has dramatically increased over the last few years, not only because of increasing numbers of difficult-to-wean patients, but also because of early timing of the procedure. The vast majority of these patients are discharged with a tracheal tube still in place, even when they no longer need ventilator support. A Spanish study shows that lack of tracheostomy decannulation in the ICU is associated with markedly increased ward mortality, at least in a large subset of these patients. The increased ward mortality may have resulted because the care of a tracheotomy is suboptimal outside a specialized environment.20 Ceriana et al21 highlighted the possibility of safely removing the tracheotomy cannula from almost 80% of patients breathing autonomously among a group of seventy-two patients recovering from weaning in a CVF, while decannulation was achieved in approximately 40% of patients transferred to a similar environment in the United States.22
Seventh, the interaction between ICU physicians and patients or their surrogates is far from optimal, especially when discussing the problem of prolonged ventilation including its outcome. A lack of prognostication, discordance between surrogates and physicians about potential outcomes, and unreasonably optimistic expectations of surrogates are potentially modifiable factors in surrogate–physician interactions. A less stressful environment than the ICU, combined with fewer sedative drugs and more comprehensive teamwork—nurses, respiratory therapists, psychologists, and clergy—typical of a CVF, may improve the patient–clinician relationship so that expectations and outcomes may be better defined and discussed.23
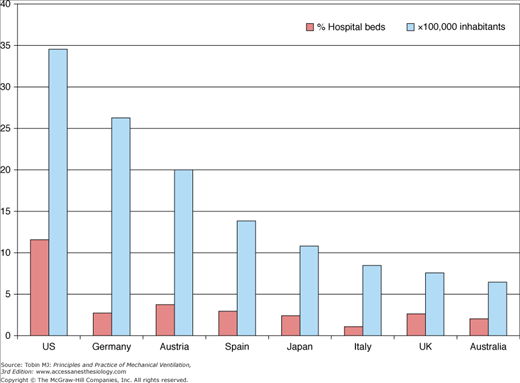
Overall, the disproportionate number of days of care required by chronically ventilated patients contributes to overcrowding despite the limited availability of ICU beds.24 As Figure 33-2 shows the number of ICU beds, in several countries. The demand for ICU beds far exceeds their availability in many European and non-European countries, so that many patients are denied ICU admission because the ICU beds are already fully occupied.25 Consequently, many critically ill patients are cared for in non-ICU beds throughout the hospital. The outcome of patients who fit ICU admission criteria but who are hospitalized in regular wards was assessed in a study performed in Israel.26 Early survival advantage in an ICU suggests that a window of critical opportunity exists for these patients. Given economic constraints and the dearth of ICU beds, it is possible that increased turnover of patients in an ICU, thus providing an opportunity for more needy patients to avail of the early benefits of intensive management, may be advantageous. This study highlights both the risk of not admitting critically ill patients to the ICU and the advantages of early discharge from the ICU for the subset of patients not in immediate life-threatening situations, but yet not ready for discharge to a nonprotected environment.26
The paucity of ICU beds is not as dramatic in the United States as in Europe, but discharge of chronic ventilator patients is still problematic. There has been an increase in the number of facilities specializing in the care of chronically ventilated patients. In Massachusetts, for example, the estimated prevalence of prolonged ventilation increased from 2.8 per 100,000 inhabitants in 1983 to 7.1 per 100,000 inhabitants in 2006, and most of these ventilator-dependent patients are in long-term acute care facilities, large urban teaching hospitals, and at home. The number of long-term acute care hospitals in the United States increased at a mean rate of approximately 9% per year, from 192 in 1997 to 408 in 2006, which resulted in an increased incidence of long-term acute care utilization after critical illness from 38.1 per 100,000 in 1997 to 99.7 per 100,000 in 2006.27
Organization of Chronic Ventilator Facilities
The term CVF is not necessarily synonymous with the so-called intermediate care unit or high-dependency unit, which are meant for patients who do not require full ICU care but are thought to need more care than usually can be offered in a general ward.28–32 Not all patients in the latter units may be ventilator-dependent, but they may require either noninvasive monitoring or noninvasive mechanical ventilation. There is no agreement about the classification of facilities for patients needing prolonged mechanical ventilation because of geographic differences, lack of consensus regarding the appropriate timing of transfer from the ICU, and different criteria of admission. For example, the American College of Critical Care Medicine states in its guidelines for admission to and discharge from adult intermediate care units that “medically stable ventilator patients for weaning and chronic care” are the ideal candidates for these environments.33 Unfortunately, these units were described only generically as “progressive-care units or single-organ subspecialty floors or chronic ventilator respiratory-care units.” Details were not provided on how these units should be organized or financially reimbursed.
Timing of discharge from the ICU is also critical. Long-term ventilator patients are often old (i.e. >75 years) and have various underlying chronic comorbidities that may complicate or exacerbate their respiratory condition at any time after discharge from the ICU.34,35 The 6-month rate of readmission to an acute care hospital is close to 40%, and readmission is often within the first 2 months after discharge from the ICU.36 Surprisingly, this rate is not influenced by the initial discharge disposition; that is, it does not differ for patients discharged to a nursing home, a CVF, or their own home. These findings indirectly suggest that not all CVFs are presently prepared to cope with the burden of a new “acute exacerbation” in such patients. For example, Nasraway et al37 found that despite a 31-fold increase in the number of all adults transferred from ICUs to extended care facilities in the Boston area between 1990 and 1996, the level of care of these facilities varied greatly depending mainly on the availability of skilled nurses.
There is still disagreement about the definition of a ventilator-dependent patient. The ninth revision of the International Classification of Diseases38 defines long-term ventilation patients as those who have received 5 or more days of ventilation. Various authors, however, have used limits as short as 48 to 72 hours and as long as 40 days.39–41 Realistically, approximately 20% of patients in an ICU require mechanical ventilation for more than 1 week, and about half of them are weaned successfully over the following few days.42 Therefore, a limit of 2 weeks has been chosen by most authors to define the threshold for ventilator dependency. The Health Care Financing Administration43 has expanded this limit to 21 days of mechanical ventilation for at least 6 hours a day. A definition based only on time, however, does not consider that for a particular patient to be regarded as ventilator-dependent (and therefore eligible for transfer to a chronic care facility), the precipitating cause of the respiratory failure must have been reversed.
CVFs have been described in the literature only in North America,44 Europe,45 and Asia.46 Substantial differences exist in their organization, location, and criteria of admission. An editorial entitled, “The Challenge of Prolonged Mechanical Ventilation: A Shared Global Experience,”47 stressed the need for common international consensus. Yet international guidelines and/or “position papers” are lacking.
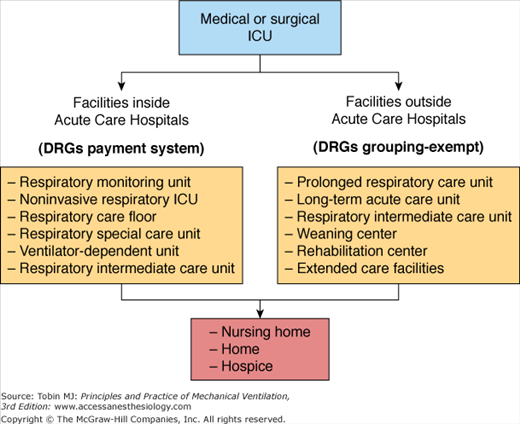
Given the confusion of terminology, we submit that the most logical classification of CVFs is one based on the location of the different facilities, specifically whether the facility is inside or outside a so-called acute care hospital. Figure 33-3 illustrates the possible sites of care for patients who are chronically ventilator-dependent. It should be borne in mind that access to these different environments may differ internationally or even regionally within the same country.
Mechanical ventilation is initiated outside the hospital in a relatively small proportion of patients; ventilation is mostly started and stabilized in an ICU.48 The timing of discharge of ventilator-dependent patients from the ICU is linked strictly to the criteria of admission of each single CVF, which are described in Chapter 34.
In the late 1980s, CVFs started to emerge in acute care hospitals as an attempt to provide an alternative therapeutic environment for ICU patients requiring prolonged mechanical ventilation. Krieger et al49,50 probably were the first to establish a CVF within an acute care hospital (Central Respiratory Monitoring Unit at Mount Sinai Medical Center, Miami, FL). They were followed shortly after by Elpern et al51,52 (Noninvasive Respiratory Care Unit of St. Luke’s Medical Center, Chicago, IL). These units were devoted mainly to patients requiring prolonged mechanical ventilation. In 1990, the Mayo Clinic opened a ventilator-dependent unit inside Saint Mary’s Hospital.53–56 Its mission was to create an environment conducive to the rehabilitation of patients with respiratory failure and also to lower the costs of ventilator-dependent patients.57 Shortly thereafter, new CVFs were opened. These went under different names at Saint Vincent’s Hospital and Medical Center in New York, (NY)58 (Nonmonitored Respiratory Care Floor) and at Cleveland Clinic Foundation in Cleveland, Ohio59 (Respiratory Special Care Unit). As discussed later (see “Outcomes and Effectiveness”), the overall rate of weaning success was high (>50%), with a mortality rate below 40%.
In Europe, the first report on this subject was published in 1995 by Smith and Shneerson60 from England. Rather than opening a special unit for patients requiring prolonged ventilation, they described the institution of a progressive-care multidisciplinary program carried out within the ICU by a dedicated team of respiratory physicians and nurses. As soon as patients were judged ready for discharge from the ICU, they were transferred to a respiratory unit, where they continued the multidisciplinary program. The program was very successful with regard to discharge to home (80% of the patients) and 1-year survival (76%). A survey45 of the European Respiratory Society on respiratory intermediate care units (RICUs) showed that during 1999, most (58%) of the 11,890 patients admitted to fifty-five RICUs received invasive mechanical ventilation. These units almost always (>90%) were inside an acute care hospital. Unfortunately, no data were available on how many of these patients actually were ventilator-dependent. Nevertheless, an Italian survey published in 200161 reported that 61% of patients receiving invasive mechanical ventilation in Italian RICUs were tracheotomized and therefore considered ventilator-dependent. The percentage is similar to that reported in Britain and Germany, where most patients survived to leave hospital, most having been weaned from the ventilator. Survivors were younger and spent less time ventilated in the referring ICU.62,63
Irrespective of location on either side of the Atlantic, the organization and staffing of CVFs inside acute care hospitals appear to be homogeneous and more similar to that of an ICU than to that of a CVF located outside an acute care hospital.64,65 Most of these CVFs provide noninvasive monitoring, the nurse-to-patient ratio is usually 1:2 to 1:4,45,51,53,58,59 and a lead respiratory therapist is assigned permanently and is present in the unit. General medical care is provided around the clock by medical house staff under the direction of an attending physician in either critical care or pulmonology. The nursing staff usually is specially trained through orientation and in-service programs to address the needs of this particular patient population. The approach to the patients is multidisciplinary, involving dieticians, psychologists, physical therapists, speech therapists, social workers, and clergy as needed. Because these CVFs are located within an acute care hospital, all the diagnostic (e.g., computed tomographic scans, nuclear magnetic resonance imaging) and therapeutic (e.g., major surgery) options are readily available. In Europe, the nurse-to-patient ratio varies slightly according to the three levels of care of RICUs.29,45 Because of the different education and responsibilities of the respiratory therapists (rarely present around the clock), an attending physician is always present in the units.66,67
This classification consists of several CVFs going under names such as regional weaning centers, prolonged respiratory care units, long-term acute care units, and RICUs inside rehabilitation hospitals. The need for these special facilities outside the acute care health system was recognized a long time ago in North America, but only recently in Europe. For example, the Comprehensive Critical Care of the British Department of Health68 stated that “the effectiveness of specialist weaning and progressive care programs for long-term ventilation of patients has been demonstrated by research, and NHS Trusts should review the need for provision of such services.”
The first experience of a CVF dedicated to the problem of ventilator-dependent patients was reported by Indihar,69–71 who described 10 years of activity, starting in 1979, of a unit located in Bethesda Lutheran Medical Center. In the late 1980s there was substantial growth of regional weaning centers in the United States. Examples include the Barlow Respiratory Hospital in Los Angeles,72,73 the Medical Center of Central Massachusetts,74 and the Hospital for Special Care, New Britain, Connecticut.75,76 Later, there was an impressive burgeoning of new long-term acute care units. By 1997, these had a capacity of about 15,000 patients per year.77 These units were established either as free-standing hospitals, as in the case of most regional weaning center, or within an acute care hospital but operating with total independence. As such, their governance is independent of the host hospital, and reimbursement is not based on a diagnosis-related grouping (DRG) system.
CVFs within a rehabilitation hospital are also popular in the United States and Europe, especially in Germany and Italy, where approximately 15% of RICUs are located inside rehabilitation centers.45,62,78,79
Unlike CVFs located within acute care hospitals, CVFs located outside appear to have a rather heterogeneous organization and staffing. This heterogeneity occurs despite these facilities espousing a program based on the common ideal of providing comprehensive medical, nursing, and respiratory care to ventilator-dependent patients. For example, New England37 has several “extended care facilities” outside acute hospitals; the skills and level of care vary dramatically among different centers. Despite the personnel being fully licensed health care practitioners, they may not all be completely familiar with the complexities of ventilator-dependent patients. Patient outcome is likely to depend on the different levels of care provided.
In most North American centers, the nurse-to-patient ratio is approximately 1:4 during the day and 1:8 at night and on weekends. A full-time respiratory therapist72,80 usually is present. The primary physicians are either internists or specialists in pulmonary and/or critical care medicine, whereas nighttime coverage commonly is provided by junior doctors. The comprehensive care team includes physical therapists, occupational therapists, speech and swallowing therapists, and clinical psychologists. Screening for admission is performed either by an attending physician or by a nurse in consultation with an attending physician.80 Weaning protocols and selection of ventilator settings during this process are implemented by respiratory therapists.81 Discharges are planned by nurses or social-work care managers. With the exception of a few facilities, which may have operating rooms for minor surgery, most CVFs located outside acute care hospitals cannot offer surgery or sophisticated diagnostic procedures.
In Europe, CVFs outside acute care hospitals are run mainly by full-time attending physicians who are specialists in respiratory and/or critical care medicine.29,45,61 These physicians are in charge of the admission and discharge of patients and the weaning protocols. They are on duty 24 hours a day. The doctor-to-patient ratio is at least 1:8. The nurse-to-patient ratio is usually similar to that of North American centers. Because of their different educational training, respiratory therapists in Europe tend to be involved mainly in rehabilitation programs, for approximately 8 hours a day (excluding Sundays and holidays), rather than in the weaning process.21 In common with North American facilities, most European CVFs do not offer major surgery.
Irrespective of their geographic location, CVFs located outside acute care hospitals are intended to provide privacy, rest, and longer visiting hours for relatives and friends. Above all, they provide physical and pulmonary rehabilitation, which has been shown to help in freeing patients from mechanical ventilation and restoring them to an acceptable level of autonomy.82
A small percentage of ventilator-dependent patients are discharged from an ICU36 directly to a nursing home. Nursing homes, however, are more likely to receive such patients once they have left a CVF. In 1991, a survey by the American Association for Respiratory Therapists83 found that nearly 30% of ventilator-dependent patients remained in CVFs for nonmedical reasons, such as reimbursement obstacles to discharge or lack of postdischarge placement options. Indeed, approximately 20% of patients cared for in a ventilator-dependent unit are transferred to a nursing home simply because they are not ready to go home.36
Nursing homes have been established all over the United States,84 either as independent units inside larger facilities or as stand-alone facilities. To the best of our knowledge, in Europe specialized units for the care of ventilator-dependent patients are very few.85 Apparently, there is no standardization of admission criteria, staffing, or organization of these units apart from the person needing “24-hour nursing care for a cognitive or a physical impairment.”86 Nurses working in this specialized area should be trained by respiratory therapists to perform specific procedures such as suctioning, tracheotomy care, and monitoring of ventilator parameters. In some cases, for example, Lakeside Hospital in Wisconsin, Eau Claire87 weekly care rounds led by a pulmonary physician with the participation of the care team, including not only the certified nurses but also respiratory therapists, dieticians, social workers, and, when possible, family members, have been introduced. In the very few observational studies performed in this kind of facility, weaning outcomes are very promising.87 Further studies are needed to define the characteristics of ventilator-dependent patients who are most likely to benefit from admission to this environment.
Criteria for Admission
Table 33-1 lists criteria for defining the “ideal” candidate for a CVF. The concept of ventilator dependency is the primary criterion for selecting admissions to a CVF. Accordingly, most centers accept only tracheotomized patients because tracheotomy per se is assumed as evidence of ventilator dependency. Significant differences on the best location of care at the time of ICU discharge between patients with and without tracheostomy has been demonstrated.88 Indeed, the dramatic increase in tracheotomies performed over the last 10 years89 suggests that ICU physicians tend to perform an early tracheotomy before trying to complete weaning. This change may reflect attempts to decongest busy ICUs more rapidly by allowing transfer of ventilator-dependent patients to extended care facilities. To avoid this problem, some units request proof that a patient has failed at least two weaning trials before being admitted.55 Other centers, however, accept patients based mainly on the availability of resources (bed and nursing staff) rather than on the basis of perceived ability to wean.62

Full access? Get Clinical Tree