Chronic Pulmonary Disease
Suzette Gjonaj MD
Carol Green-Hernandez PHD, FNP-C
Daniel Z. Aronzon MD, FAAP
Jean Lavelle RN, MSN, FNP
Mardhie E. Coleman RN, PhD(c)
Hendrika J. Maltby RN, PhD, FRCNA
Linda J. Kristjanson RN, PhD
Suzanne M. Robinson RN, MSC, PhD(c)
PART 1 Chronic Lung Diseases: Asthma and Cystic Fibrosis
Suzette Gjonaj MD
Carol Green-Hernandez PHD, FNP-C
Daniel Z. Aronzon MD, FAAP
INTRODUCTION
The lung is a remarkable organ that primarily serves as a unit of gas exchange. Asthma and cystic fibrosis (CF) are chronic lung diseases frequently seen in the pediatric population. Either of these lung diseases can impact a child’s pulmonary function and, especially in the case of CF, other organ systems. This chapter provides pediatric primary care clinicians with content on the diagnosis and management of asthma and comanagement (with pediatric pulmonologists) of CF. It will examine quality of life issues, because children with these diseases face many challenges.
ASTHMA
Asthma, a chronic disorder of the airways, is characterized by inflammation that leads to hyper-responsiveness of the airways. Airflow limitation results from bronchoconstriction, mucus plugs, and increased inflammation (U.S. Department of Health and Human Services, 1997). Airflow limitation is reversible or partially reversible. Upon receiving a bronchodilator, pulmonary function improves to normal or near normal. Left untreated or undertreated, remodeling of the airways occurs with permanent changes (Laprise, Laviolette, Boutet, & Boutet, 1999).
Pathology
Although asthma exacerbations are episodic, the pathologic feature of the disease is chronic airway inflammation. Attacks often present with symptoms of coughing, wheezing, chest tightness, and difficult breathing. Histologic features of asthma include subepithelial fibrosis, collagen deposition, epithelial shedding, goblet cell metaplasia, smooth muscle hypertrophy, and infiltration of the submucosa by eosinophils (Djukanovic et al., 1990). Mucosal edema often results from microvascular leakage and hypersecretion of mucus from goblet cells, thereby causing mucus plugging of the peripheral airways and focal atelectasis.
Six risk factors exist for the pathogenesis of asthma:
Respiratory infections. Rhinoviruses, respiratory syncytial virus (RSV), and influenza and parainfluenza are the most common responsible viruses. Evidence has shown that respiratory illnesses in childhood may predispose to airway reactivity. Fifty percent of children with RSV bronchiolitis continue to have airway hyper-responsiveness and abnormal pulmonary function tests (Rooney & Williams, 1971; Welliver, 1995; Sigurs et al., 1995). Recent long-term studies have shown that wheezy infants may have narrower peripheral airways, predisposing them to wheeze with viral infections (Martinez et al., 1995). These children, however, may “outgrow” wheezing as they grow older and their airways enlarge.
• Clinical Pearl
In children, the most common trigger for an asthmatic episode is a viral illness.
Parental smoking and other indoor environmental pollutants. Maternal smoking during the perinatal period or thereafter (Murray & Morrison, 1986; American Academy of Pediatrics [AAP], 1999) and other indoor pollutants, such as wood stove smoke and dust mite exposure, have been shown to increase the severity of symptoms in children with asthma. Response to parental smoking is worse in males and older children with asthma (Murray & Morrison, 1989). The duration of the fetus’s exposure and the number of cigarettes the mother smokes also play a role. Intrauterine exposure to cigarette smoke increases immunoglobulin E levels in the fetus and airway responsiveness at birth. These factors place the infant at risk for developing atopy and asthma in childhood (Young et al., 1991).
Atopy. Most patients with asthma exhibit atopy (Gergen & Turkeltaub, 1992). Exposure to inhaled allergens in early life increases the risk of developing asthma. Studies show a correlation between the level of exposure to dust mites in early infancy and the age at which wheezing subsequently develops (Sporik, Holgate, Platts-Mills, & Cogswell, 1990). The link between food allergy and asthma is controversial. It is rare for a pulmonary reaction to occur secondary to food allergen exposure.
Genetics. Evidence suggests that genetic factors play a role in asthma. One or both parents with asthma have a greater risk of having an asthmatic child than when neither parent is affected (Horwood, Fergusson, Hons, & Shannon, 1985). Seventeen percent of parents and 8% of siblings of asthmatic children have asthma themselves (Sibbald, Horn, Brain, & Gregg, 1980).
Infants of mothers who are heavy smokers have an increased incidence of wheezing and nonwheezing lower respiratory illnesses, even if they do not attend day care. Children with atopic dermatitis are more likely to develop asthma if their mother is a smoker.
Air pollution. Controversy exists as to whether a child’s exposure to sulphur dioxide (SO2) and consequent decreased oxygen (O2) and increased ozone levels lead to exacerbation of asthma symptoms. Epidemiologic evidence, however, demonstrates increased incidence in regions and countries with decreased air quality (1999) AAP.
Socioeconomic factors. Individuals of African American heritage and lower socioeconomic status have a higher incidence of asthma. It appears that this may be due to the environmental factors associated with poverty and inner-city living (Weitzman, Gortmaker, & Sobol, 1990).
Epidemiology
Asthma is a common pediatric disease. Its incidence and prevalence are increasing throughout the world despite the improved understanding of its pathogenesis. The prevalence of asthma in the United States has increased from 31 per 1000 in 1980 to 54 per 1000 in 1994 (Centers for Disease Control and Prevention [CDC], 1998). Both incidence and prevalence are higher in African Americans compared with Caucasians (CDC, 1998; Lang & Polansky, 1994). Trend in mortality also increased by 6.2% per year during the 1980s (Weiss & Wagnerer, 1990). This trend continued into 1990s, with a higher mortality among individuals of African American heritage (Oliverti, Kercsmar, & Redline, 1996). Unlike other racial and ethnic groups, lifetime incidence of asthma and associated emergency care in African Americans does not change with improved socioeconomic status. Reasons for this epidemiologic fact are not yet clear (Miller, 2000).
Estimated health care costs (inpatient and outpatient) associated with asthma exceed $4 billion per annum (Taylor & Newacheck, 1992). Developed countries have a higher prevalence than third world countries, with less than 1% in some developing countries versus greater than 20% in some developed countries (Valacer, 2000; Newacheck & Halfon, 2000).
History and Physical Examination
When examining the child, the provider should obtain a careful history, paying attention to the following recurrent signs and symptoms:
Wheezing
Cough, especially worse at night
Difficulty breathing
Chest tightness
Sinusitis
Allergic rhinitis or atopic dermatitis
Symptoms of wheezing, chest tightness, shortness of breath, or cough worsening when exposed to airborne allergens or irritants or during or after exercise (AAP, 1999).
In addition, the provider should document a family history of asthma, allergies (including atopic skin disease), sinusitis, or rhinitis (AAP, 1999).
The clinician should ask whether symptoms tend to worsen when the child is exposed to exercise, viral infections, animals with fur, dust mites, tobacco smoke, pollen, changes in temperature, strong emotional expression (laughing or crying hard), or exposure to aerosolized chemicals. The provider also should ask about self-treatment, including over-the-counter herbal remedies or asthma, cough, or cold medications. Display 55-1 provides a format for taking a comprehensive history for asthma.
DISPLAY 55–1 • Format for a Comprehensive History in the Diagnosis of Asthma
Features to Note in an Asthma History
Nature of symptoms (wheeze, cough, chest tightness, dyspnea)
Pattern of symptoms (seasonal, diurnal variation, severity, frequency, triggering factors)
Frequency of hospitalizations, pediatric intensive care unit admissions, emergency room visits
Previous and current drug therapy, including over-the-counter drugs
Atopic history and environmental history
Impact of disease on child (school performance and attendance)
Family history
General medical history
Most children older than 3 years with asthma are atopic, so the provider should obtain a comprehensive environmental history. A sample format for an environmental history can be found in Display 55-2.
DISPLAY 55–2 • Sample Environmental History Format
History of smokers (including family members and patient)
Heating system (forced air, wood burning stove, kerosene heater)
Humidity of home (> 50% allow dust mites to thrive)
Presence of carpets, fabric upholstery, uncovered mattress, and pillow are sites where dust mites live
Presence of animals (cats, dogs)
Use of humidifiers (source of mold spores)
Seasonal worsening of symptoms (trees, grasses, weeds)
Physical examination should include observation of the child’s pulse rate and rhythm, resting respiratory rate, signs of respiratory distress, evidence of cyanosis in lips and nail beds, signs of nail clubbing, and use of accessory muscles and chest circumference. The provider should auscultate the heart and examine the abdomen. He or she should inspect the skin for signs of atopic skin disease (AAP, 1999).
The provider can perform chest percussion in the older toddler and older children in general. Hyper-resonance indicates air entrapment, while any areas of percussed dullness can be mapped out for discerning mucous plugs versus areas of consolidation. If the provider suspects the latter, he or she should assess for “e” to “a” changes over the areas of dullness. The provider needs to pay special attention to the I:E ratio, normal being 2:1. He or she should auscultate over each lung area for a complete respiratory cycle, being careful to listen for full end-expiratory sounds.
• Clinical Pearl
Expiratory phase prolongation is one of the earliest signs of bronchial narrowing.
Diagnostic Criteria
The provider must consider many differential diagnoses before making the final determination that the patient has asthma. Display 55-3 provides the differential diagnosis for the conditions that are most closely associated with recurrent wheezing symptomatology in children. Because many of these problems present with similarities on physical examination, the clinician must carefully weigh these findings in tangent with diagnostic studies and laboratory tests.
DISPLAY 55–3 • Differential Diagnosis of Cough and Wheeze in Infants and Children
Cystic fibrosis and immotile cilia syndrome
Foreign body
Recurrent aspiration
Vascular anomalies
Tracheomalacia
Bronchiolitis obliterans
Immune deficiency states
Bronchopulmonary dysplasia
Left ventricular failure
Mediastinal masses
Clinicians should note that in children younger than 5 years, wheezing may occur with acute upper respiratory infections. These patients are often diagnosed as having bronchitis, bronchiolitis, or pneumonia, with the result that
they do not receive appropriate therapy for what is in reality asthma. Providers should follow the diagnostic criteria listed in Display 55-3, with the exception that spirometry is not feasible in these young patients (AAP, 1999).
they do not receive appropriate therapy for what is in reality asthma. Providers should follow the diagnostic criteria listed in Display 55-3, with the exception that spirometry is not feasible in these young patients (AAP, 1999).
• Clinical Pearl
A diagnosis of asthma is not required to begin treatment with asthma therapy. If effective, a trial plan using asthma medications will assist the pediatric provider in making the diagnosis of asthma (AAP, 1999).
In children 5 years old and younger who have wheezing in association with an acute upper respiratory viral infection, two general patterns of asthma occur:
Symptom remission during the preschool years
Persistence of asthma, continuing throughout childhood (AAP, 1999)
Diagnostic Studies
Spirometry and peak expiratory flow may show reversible and variable airflow limitation. Pulmonary function tests (eg, body plethysmography) can be done in specialized laboratories in children as young as 3 years (Kanengeiser & Dozor, 1994). Infant pulmonary function tests can be done in specialized laboratories, but in most cases, such testing is expensive and impractical. A more useful approach for the primary care provider is to test the effectiveness of bronchodilators in infants and young children. If a child shows a clinical response to this medication, the provider can presume that the patient has reversibility of bronchoconstriction. In the office, providers may use peak flow meters; however, peak flow has its limitations, as it only evaluates large airway flow. Peak flow is also an extremely effort-dependent test; many children have difficulty performing it. Spirometry can be done in an office setting. If abnormal, the provider can administer a bronchodilator and repeat spirometry to evaluate the patient’s response to the bronchodilator.
Chest radiographs also may be useful. Asthmatic lungs may show hyperinflation. Radiographs also may help in narrowing the differential diagnosis by detecting parenchymal disease, congenital anomaly, or foreign bodies.
Management
The goals of asthma management are to minimize or abolish symptoms by selecting appropriate medications and to identify and avoid known triggers. Achieving these goals is important for the child to maximize lung function, minimize exacerbations, prevent limitations on activity, and avoid side effects to medications.
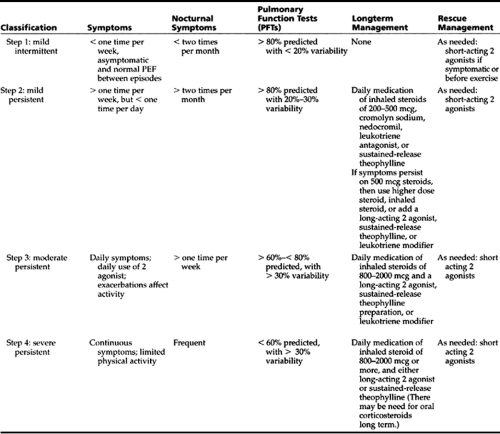
Table 55-1 provides the classification of asthma severity and peak flow and management information. Once asthma has been classified, current therapy follows a “step-wise” approach to asthma treatment. The patient is placed on appropriate medications for that step, and once control is obtained and maintained for about 3 months, there is a step-down in medications to the least required to control symptoms. Table 55-1 also delineates medications and guidelines for their use in asthma therapy.
There are two groups of asthma medications: reliever and controller medications. As Table 55-1 illustrates, patients in step 2 and above will benefit from controller medications.
Controller medications include the following:
Corticosteroids
Sodium cromoglycate
Nedocromil
Long-acting β2 agonists
Leukotriene modifiers
Sustained-release theophylline
The reliever medications include the following:
Short-acting β2 agonists
Anticholinergics
Short-acting theophylline
Epinephrine injections
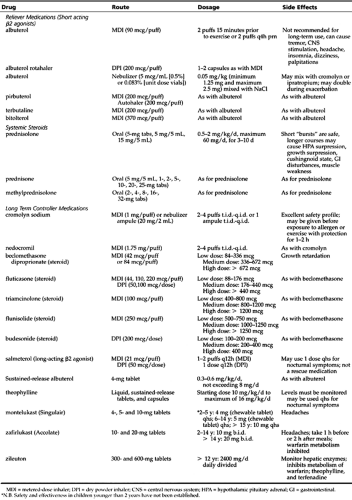
Table 55-2 provides a synopsis of controller and reliever medications used in the treatment of asthma. The following discussion provides more in-depth information about these drugs.
Controller Medications
Inhaled Steroids
Since asthma has been recognized as an inflammatory disease, inhaled corticosteroids have played a vital role in its management (Barnes, 1993). Data suggest, however, that inhaled corticosteroids may have significant effects on a child’s growth velocity (Witzmann & Fink, 2000).
Inhaled steroids have a broad mechanism of action, which may account for their significant efficacy as a controller medication. Steroids prevent exacerbations of the child’s asthma, while decreasing airway hyper-responsiveness, improving pulmonary function tests, reducing asthma severity, and preventing airway remodeling (Vathenen, Knox, Wisniewski, & Tattersfield, 1991).
Administration by the inhaled route has aided greatly in the management of asthma. There is high topical anti-inflammatory effect with limited systemic absorption. Long-term use of inhaled steroids reduces airway inflammation and bronchial reactivity (Juniper et al., 1990). Steroids block the late phase of asthma very well. Administration of steroids just prior to exercise does not block exercise-induced symptoms, but regular use does decrease the severity of exercise-induced asthma (Hendricksen & Dahl, 1983).
In Canada and many other countries, as well as in Europe, inhaled steroids are given by metered-dose inhalers (MDI), dry powder delivery systems, or nebulized solutions. This last delivery method is not yet approved for use in the United States, although that is expected to change. The dose of steroids ranges from low dose (200–500 mg/d) to high dose (800–2000 mg/d). One study suggests that doses over 400 mg/m2 per day may cause adrenal suppression (Oriftis, Milner, Conway, & Honour, 1990).
Because of the possible impact inhaled corticosteroids can have on a child’s linear growth velocity, the primary care provider should record the patient’s height and compare to standard growth charts at each 6-month visit until completion of growth. If there is any question as to the child’s growth trajectory, the provider should refer the patient to a pediatric endocrinologist for evaluation (Witzman & Fink, 2000; Littlewood, Johnson, Edwards, & Littlewood, 1988; AAP, 1999).
Some reports indicate that patients may have “catch-up” growth once steroids are discontinued. Other possible side effects of high-dose inhaled steroids include bone resorption and demineralization (Ali, Capewell, & Ward, 1991), cataracts (Karim, Thomson, & Jacob, 1989), and skin atrophy (Capewell, Reynolds, Shuttleworth, Edwards, & Finlay, 1990). Candida
infection of the oropharynx is rare in children (Shaw & Edmunds, 1986). Risks for Candida are decreased further with the use of spacer devices, mouth rinsing after taking the drug, and less frequent dosing schedules (Toogood et al., 1984). Oral steroids are rarely needed in the control of asthma in children. They are extremely useful, however, for short bursts of 4 to 6 days or so, until inhaled steroids can take effect. If a child needs oral steroids, then providers should prescribe the lowest dose possible, preferably on a once daily schedule. There may still be adrenal suppression with alternate-day dosing (Dolan et al., 1987).
infection of the oropharynx is rare in children (Shaw & Edmunds, 1986). Risks for Candida are decreased further with the use of spacer devices, mouth rinsing after taking the drug, and less frequent dosing schedules (Toogood et al., 1984). Oral steroids are rarely needed in the control of asthma in children. They are extremely useful, however, for short bursts of 4 to 6 days or so, until inhaled steroids can take effect. If a child needs oral steroids, then providers should prescribe the lowest dose possible, preferably on a once daily schedule. There may still be adrenal suppression with alternate-day dosing (Dolan et al., 1987).
Providers should note that not all inhaled steroids are equally potent. Some factors that affect efficacy are topical potency, lipophilicity, receptor binding affinity, and receptor binding half-life. Fluticosone has the greatest topical potency of the corticosteroids, being twice as potent as beclomethasone and about four times more potent than flunisolide and triamcinolone. Fluticasone also has the longest elimination half-life and the greatest adrenal-suppression effect. Because it has the least gastric and pharyngeal absorption, however, its potential for true adrenal suppression may not really be an issue.
Sodium Cromoglycate (Cromolyn)
Sodium cromoglycate (CS) is strictly a preventive drug and has no bronchodilating effects. Because it is an anti-inflammatory agent, it inhibits both early and late phases of asthma. Although CS is expensive, it has few side effects (Murphy, 1988; AAP, 1999). The patient must be an active participant in its use, starting with a four times daily regimen, which then may decrease to three times a day. If used less than three times a day, CS has no effect. CS may be of greater value when it is administered using a nebulizer. It blocks both allergy- and exercise-triggered symptoms well. It also may be used 15 to 20 minutes prior to exposure to allergen or exercise. For seasonal allergy, it is beneficial to start CS several weeks before and continue throughout the expected allergy season. About 66% of patients gain benefit from CS; however, CS is of no value in any child with asthma who is steroid dependent.
Nedocromil
Nedocfomil (NC) has an anti-inflammatory action similar to CS. It inhibits inflammation by blocking the chloride channels, modulating mast cell mediator release, and recruiting eosinophils. NC reduces bronchospasm triggered by cold dry air and exercise. It has been shown to decrease the need for quick-reliever medications, improving peak flow and reducing asthma symptoms. Some adult (Bone et al., 1990) and pediatric (Kemp, 1992) studies show a synergistic effect with inhaled corticosteroids, while other work does not support this effect (Boulet et al., 1990; Goldin & Bateman, 1988). The disadvantage of NC use is that 20% to 30% of users report an unpleasant taste, which may affect a child’s willingness to use the medication.
Long Acting b2 Agents
As with the short-acting β2 agonists, long-acting β2 agents work by relaxing smooth muscles in the airway. They are often used in conjunction with anti-inflammatory medications. Recent studies suggest that this combination is better than doubling the dose of the steroid (AAP, 1999). The combination is used as a controller medication and is often helpful for nocturnal and exercise-induced symptoms. Recent case reports of sudden death while using these long-acting drugs have not been supported in more controlled studies.
Leukotriene Modifiers
This new line of medications blocks the steps that involve cysteinyl leukotrienes in the inflammatory cascade. Montelukast (Singulair) and zafirlukast (Accolate) work by blocking leukotriene D4 receptors, whereas zileuton inhibits the 5-lipoxygenase enzyme, thereby inhibiting the production of various leukotrienes (eg, B4, C4, D4, and E4). A modest increase in forced expiratory volume (FEV1) by 10% to 15% was seen in clinical trials (Locker, Lavins, & Snader, 1995). In mild to moderate asthmatics, there was a reduction in β2 agonist use. The ease in taking an oral medication once or twice daily is certainly an advantage, as it will enhance compliance. The disadvantages are possible systemic side effects and drug–drug interactions.
Zileuton affects the metabolism of warfarin, theophylline, and terfenadine and can affect liver function. Zafirlukast also affects the metabolism of warfarin and requires liver function monitoring. Zafirlukast and montelukast have both been implicated in unmasking or causing Churg-Strauss syndrome. This syndrome is a vasculitis characterized by peripheral eosinophilia, pulmonary infiltrates, sinus complications, neuropathy, and asthma symptoms (eg, cough).
Theophylline
The use of theophylline is somewhat outdated. Its disadvantages include no sustained decrease in airway hyper-reactivity, high incidence of side effects, and possible behavioral and learning disturbances in some children.
Although theophylline is no longer a first-line medication, it is useful in selected cases. In patients who are inadequately controlled with long-acting β2 agonists and inhaled steroids, the addition of theophylline may be beneficial. For patients who are hospitalized with nocturnal symptoms, a dose at bedtime may help (Barnes, Greening, Neville, Timmers, & Poole, 1982). Patients who are unable to participate in a regimen that includes inhaled medications may tolerate theophylline.
Serum levels of theophylline should be between 12 and 15 mg/L to minimize the risk of side effects. Once therapeutic levels and control of symptoms are achieved, then serum levels should be monitored every 6 to 12 months.
If the patient has fever or is on erythromycin, the provider should lower the dose of theophylline by about 50% because the metabolism of theophylline may be affected. Chronic long-term use of theophylline may carry an added risk of mortality.
Reliever Medications
Short Acting β2 Agonists
This class of medications is the most potent of the bronchodilators. Short-acting β2 agonists include albuterol, pirbuterol, bitolterol, fenoterol, metaproterenol, isoetharine, and terbutaline. Their duration of action is between 4 and 8 hours. This class of medications also increases mucociliary clearance and has some anti-inflammatory effects. The typical side effects of these medications include tachycardia, tremor, and hypokalemia. Most children, however, experience few or minimal side effects.
Short-acting β2 agonists should be used as rescue treatment, because studies suggest that there may be down-regulation
of receptors with frequent use of these drugs (Lipworth, 1997). Recently, the FDA has approved the use of levalbuterol in patients with asthma. In racemic albuterol, it is the (L)-albuterol that has bronchodilator effects. The (S)-albuterol has no therapeutic benefit and is responsible for the side effects. It appears that levalbuterol has a better therapeutic index than racemic albuterol (Gawchik, Saccar, Noonan, Reasner, & DeGraw, 1999). Whether the increased cost of levalbuterol justifies its decreased rate of side effects, however, remains to be seen. Its niche may be as a short-term reliever in children who have severe side effects with albuterol.
of receptors with frequent use of these drugs (Lipworth, 1997). Recently, the FDA has approved the use of levalbuterol in patients with asthma. In racemic albuterol, it is the (L)-albuterol that has bronchodilator effects. The (S)-albuterol has no therapeutic benefit and is responsible for the side effects. It appears that levalbuterol has a better therapeutic index than racemic albuterol (Gawchik, Saccar, Noonan, Reasner, & DeGraw, 1999). Whether the increased cost of levalbuterol justifies its decreased rate of side effects, however, remains to be seen. Its niche may be as a short-term reliever in children who have severe side effects with albuterol.
Anticholinergics
Ipratropium bromide has a slower onset of action but a longer duration of action than β2 agonists; however, ipra-tropium bromide has less bronchodilating properties. In status asthmaticus, the addition of ipratropium bromide provides additional bronchodilation of airways (Rowe, Travers, Holroyd, Kelly, & Bota, 1999). There is no defined role for ipratropium bromide in the maintenance management of asthma. Side effects are not common.
Goals of Asthma Management
The goals of asthma management include the following:
Minimizing chronic symptoms
Decreasing exacerbations
Minimizing use of rescue β2 agonists (see Table 55-2)
Preventing exercise limitations
Promoting normal pulmonary function
Preventing adverse side effects from medications
The child should see the provider every 1 to 6 months, depending on response to therapy (AAP, 1999). During these visits, providers should review therapy goals with the child and parent. They should examine attainment of goals and address concerns. The provider must review the management plan with the patient and family. Children with moderate-to-severe asthma need to monitor their peak flows. The child or parent should perform a return demonstration of peak flow measurement and inhaler use at the time of each office visit. The pediatric provider should then make adjustments in the teaching and treatment plan, based on need (AAP, 1999).
If the patient remains stable for 3 months, then the provider should follow a step down in long-term treatment. If symptoms are not subsequently controlled, the clinician should review content with the parents, teaching them to assess whether the child is using medications as prescribed, while also reviewing proper techniques of medication administration with spacer devices. The provider should review environmental control measures, ensuring that they are in place. If the family indeed understands and is following the management plan, then the provider should consider a step up in preventive medications. The following discussion describes different methods for providing medication to the child with asthma.
Drug Delivery Systems
Inhalation is the preferred route to administer medications in asthma. Inhaled medication can be deposited directly in the airways, where it has a shorter onset of action. The child needs lower doses when inhaling a medication and thus experiences fewer side effects. Three inhalation routes are available:
Nebulizer
MDI
Dry powder
Nebulizer
An advantage of this system is that it does not require patient coordination, so young patients and those who are very ill can easily use it. Its disadvantages are that nebulizers are generally expensive, not very portable (except for the ultrasonic nebulizers), and overall, very inefficient. Up to 60% of the nebulized drug may be lost with this method of administration (Salzman, Steele, Pribble, Elenbaas, & Pyszczynski, 1989). A nebulizer can deliver several short-acting β2 agonists, anticholinergics, cromolyn, and corticosteroids. Of these, corticosteroids are not yet available in the United States for nebulization, although they are available in several other western countries.
Metered-Dose Inhalers
The MDI devices are portable and inexpensive. They require ideal inhalation technique if used without a spacer device. Even with optimum technique, MDIs deposit most of the medication in the oropharynx, with only about 10% reaching the airways. Because of the difficulty in otherwise achieving therapy results, spacer bars are recommended for MDIs.
Spacers and breath-actuated devices increase deposition of drug in the airways. The better spacers have large volumes and the added advantage of reducing oropharyngeal candidiasis. Cromolyn, ipratropium bromide, nedocromil, and a variety of β2 agonists and steroids are available in MDI form.
• Clinical Pearl
The provider should review MDI technique with a spacer device at every visit. He or she should encourage its use at every opportunity. The provider should also teach the patient how to use the rolled-up fist as a “built-in” spacer if one is lacking or the child refuses to carry or use it in front of friends.
Dry Powder Inhalers
This line of medications requires less coordination from patients, but an adequate inspiratory flow rate (>60 L/min) is necessary. This method of delivery may be inadequate in acute exacerbations when the flow rate is reduced. Single- and multiple-dose inhalers are available. A variety of steroids and β2 agonists are available in this form.
What to Tell Parents
Providers should instruct parents and all caregivers that they need to report all asthma episodes to them immediately. Additional office visits may be warranted if instability is noted. In the event that practice coverage is not available, providers should instruct all caregivers to follow up immediately with an emergent provider. In the event that emergency transport to a care center is needed, providers should instruct caregivers to use ambulance rather than private transportation services. Such arrangements are vital should a child’s airway be lost while en route for emergent treatment. The goal of therapy must be prevention to minimize
the need for emergent intervention, whose positive outcomes cannot always be guaranteed.
the need for emergent intervention, whose positive outcomes cannot always be guaranteed.
Concerns in Infants and Young Children
Infants and young children are prone to have wheezing episodes for a multitude of reasons:
Increased compliance of their chest wall
Lower elastic recoil of the lung
Increased resistance of peripheral airways
Increased fatigability of the diaphragm muscles
Some infants will be transient wheezers and by ages 3 to 5 years, have no further symptoms (AAP, 1999). This group presents a challenge to providers. The diagnosis of asthma is made on clinical grounds. Viral infections rather than allergen exposure trigger most episodes, the latter of which is seen in the older child. Infant pulmonary function tests can be done; however, they are expensive and difficult to obtain and require specialized laboratories. These problems make infant pulmonary function testing generally impractical.
• Clinical Pearl
The diagnosis of asthma is confirmed when the patient responds favorably to a trial of bronchodilators.
An even greater challenge is to administer medications, although these are usually given by nebulizer. If a child needs preventive medications, few data in this population exist about the use of asthma drugs in infants. An effective method of drug delivery can pose another challenge, because parental and caretaker participation in the prescribed regimen typically requires them to give lengthy and multiple nebulized treatments daily. Conversely, they may struggle with giving the child an MDI with a spacer, which may be less effective than in the older child who is often better able to tolerate this method of delivery.
Parents and caretakers need clear teaching about asthma and how to use medications. The provider also should give consistent support and ongoing review about medications and their administration, virus and other episodic illness guidelines, and environmental control measures.
Concerns in Older Children and Adolescents
Older children and adolescents with asthma can present a special challenge for practitioners. These children are developmentally inclined to deny the chronicity of their asthma and to ignore or deny symptoms. They may be angry about their disease, believing that they can ignore symptoms without consequences.
The older child or adolescent may begin smoking, have poor relationships with authority figures, and may abuse their MDIs. With the wide variety of medications and delivery systems available, a mutual decision between provider and patient can assist in developing a partnership that will help the older child or adolescent, while supporting parents in their concerns. In many ways, the older child with asthma behaves as any other adolescent living with chronic disease, whether it be diabetes, cancer, or any other serious health concern. The reader is referred to Chapter 12 for a review of the developmental sequellae of this age category and its meaning in primary care.
Cough
Cough-variant asthma is seen in some patients. These patients may have cough as their only symptom of asthma. Abnormalities typical of reversible obstructive airway disease include reduced large and small airway flows, increased thoracic gas volumes, and residual volumes that are reversible or partially reversible after a bronchodilator. Although cough is often a challenge to treat, standard asthma management is typically quite successful.
Exercise and Sports Participation
Exercise-induced asthma occurs with most children. A peak in airway obstruction occurs about 15 minutes after exercise begins, but there also may be a delayed phase, occurring a few hours after exercise. Symptoms are more severe when exercising in cold, dry air. The provider should stress the importance of pretreatment with a β2 agonist or cromolyn 15 to 20 minutes before exercise. The clinician needs to emphasize that some children will still need a rescue inhaler with them while exercising. Therefore, the β2 agonist may be a better inhaler choice, especially for youngsters who are unwilling to carry more than one inhaler with them. In any event, pretreatment before exercise may prevent symptoms.
• Clinical Pearl
With proper medication, support, and education, most children with asthma can engage in physical activities, including endurance sports. Only patients with the most severe form of asthma need to modify their participation in sports and physical activity (AAP, 1999).
Immunizations
All children and adolescents with asthma should receive influenza prophylaxis. Patients with severe asthma are candidates for the pneumococcal vaccine.
Nocturnal Asthma
Nocturnal asthma is seen in some children. Wheezing and coughing may occur at night or in the early morning. The provider should reassure parents that initial management aims at optimizing overall control of asthma.
If nocturnal symptoms persist, the clinician should prescribe a nighttime dose of sustained-release theophylline or a leukotriene modifier. Either medication may alleviate the patient’s nocturnal symptoms.
Emergencies
Acute exacerbations of asthma are quite common and can be potentially life threatening. Asthma accounts for many emergency room (ER) visits and a large percentage of hospitalizations. Most severe episodes can be prevented if they are recognized early and treated aggressively. The use of β2 agonists and systemic steroids in the early stages of an exacerbation can halt the episode. If the patient is not responding to these medications at home, the provider should refer him or her to an ER for further evaluation and management. Display 55-4 illustrates the pathology of an acute asthma episode.
DISPLAY 55–4 • The Pathology of an Acute Asthmatic Episode
Triggers: Viral infections, pollutants, allergies, exercise, sinusitis, aspirin
Airway obstruction: increased airway obstruction, reduced flow rates (FEV1, PEFR), hyperinflation, air trapping, increased resistance, decreased compliance
V/Q mismatching: some airways overventilated; others underventilated
Full access? Get Clinical Tree