Chronic Orthopedic Problems
Keith P. Mankin MD
Orthopedic Disorders
INTRODUCTION
Orthopedic disorders may be developmental and may lead to longstanding problems involving growth and normal physical activity. As with acute entities, the earlier these problems are recognized, the better they can be treated. Detection may be as early as birth in some cases, but other, more subtle problems may only become clear at major milestones like the onset of ambulation or during periods of rapid growth.
Although many of these entities may require a specialist’s evaluation, this chapter describes the role of the primary care provider in diagnosing and helping to instruct and support the family during the long and frustrating clinical course of managing chronic orthopedic problems.
Hip Disorders
Developmental dysplasia of the hip (DDH) is defined as disruption of the normal hip joint alignment and stability. In its most extreme state, the hip or hips may be completely dislocated, with almost no socket formation. Most frequently, there is only mild shallowness of the socket, and the hip may push out of the socket only in a stressed position. Unfortunately, the normal development of the hip depends on normal forces being applied throughout growth. Thus, even a mildly shallow hip may develop into severe hip disease early in adulthood.
EPIDEMIOLOGY
Developmental dysplasia of the hip is more frequent in girls, especially first-born (Weinstein, 1996). It is also associated with conditions that limit the room for the fetus, especially breech position and multiple births. There is a close association between DDH and other molding disorders, such as wryneck and foot deformities. However, there is a clear familial tendency to dysplastic hips, although the exact genetic basis is unknown.
HISTORY AND PHYSICAL EXAMINATION
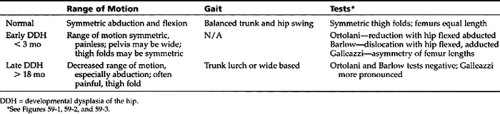
Early in development, even dysplastic hips tend to be free of symptoms. Because muscle development may be normal, children will not have delayed ambulation except in very extreme cases or in cases associated with neurologic disorders. Later, the child may complain of increased tiredness or stiffness. By the late teens to early adulthood, the hips may be painful, particularly with running and other strenuous activity. This probably indicates the early development of arthritis. Table 59-1 presents data regarding the examination of range of motion, gait, and specific tests for normal hips and early versus late DDH.
At birth, the hips may be innately loose, but the laxity should resolve by 2 to 4 weeks. In the nursery, laxity is felt by pushing the hips outward (Barlow test) or bringing them back to the socket (Ortolani test). Figure 59-1 illustrates these maneuvers. These tests typically elicit an emphatic “clunk.” More subtle noises, such as “clicks” or “pops” may represent insignificant ligamentous snapping. Other early signs include leg length discrepancy, as illustrated in Figure 59-2 by the Galleazzi test, asymmetry of thigh folds, as seen in Figure 59-3, or widening of the pelvis. For late physical findings see Table 59-1.
 Figure 59-1 Barlow (A) and Ortolani (B) tests for hip instability. The Barlow test pulls the flexed hip towards midline and a posterior force is applied. The Ortolani pushes the flexed hip outward. A palpable “clunk” is felt in a positive test. Adapted with permission from Morrissey, R.T., & Weinstein, S.L. (Eds.). (1996). Lovell & Winter’s pediatric orthopaedics (4th Ed.). (p. 75). Philadelphia: Lippincott-Raven. |
 Figure 59-2 The Galleazzi test demonstrates apparent femoral length difference in a child with dislocated hip. The test may be negative if both hips are dislocated. Adapted with permission from Morrissey, R.T., & Weinstein, S.L. (Eds.). (1996). Lovell & Winter’s pediatric orthopaedics (4th Ed.). (p. 912). Philadelphia: Lippincott-Raven. |
 Figure 59-3 Thigh-fold asymmetry in a child with posteriorly dislocated hip. Note also the apparent widening of the pelvis on the left, dislocated side. Adapted with permission from Morrissey, R.T., & Weinstein, S.L. (Eds.). (1996). Lovell & Winter’s pediatric orthopaedics (4th Ed.). (p. 76). Philadelphia: Lippincott-Raven. |
DIAGNOSTIC STUDIES
Because the proximal hip is entirely cartilage for the first 4 to 5 months, early radiographs may not reliably show the condition of the joint. Ultrasound is the most useful imaging modality in younger infants from birth to age 4 or 5 months (Harding et al., 1997). A good ultrasound image demonstrates not only the formation of the ball and socket, but also instability of the joint. To prevent false-positive studies due to the generalized joint laxity that is common in all newborns, ultrasound should be done no earlier than 2 weeks of age, except in extreme cases.
At older ages, the radiographs may show partial or complete migration of the hip from its socket. This is illustrated in Figure 59-4. The socket itself may be very shallow and oversized. Later radiographs may also demonstrate pressure areas, which may represent early arthritis.
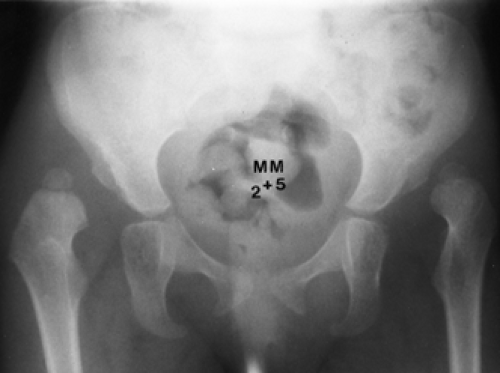 Figure 59-4 Radiograph of a 2-year-old child with bilateral hip dislocation. Note the shallow sockets as well as the abnormal placement of the femoral heads. Adapted with permission from Morrissey, R.T., & Weinstein, S.L. (Eds.). (1996). Lovell & Winter’s pediatric orthopaedics (4th Ed.). (p. 913). Philadelphia: Lippincott-Raven. |
MANAGEMENT
If detected early, mild to moderate cases of DDH can be treated in abduction braces, such as the Pavlik harness seen in Figure 59-5. This device directs the hip in a stable position and thus maximizes the child’s own developmental potential (Harding et al., 1997). This treatment is most effective under 3 months of age. Multiple diapers (triple or double) may have some benefit early on, particularly while waiting for a consultative appointment, but they do not provide enough stability to maintain a corrective position, so they are not definitive treatment. Beyond 6 months of age, more rigid immobilization, such as casting, and possibly surgical procedures, such as open hip reduction and realignment of
the bones of the hip and pelvis, more frequently become necessary.
the bones of the hip and pelvis, more frequently become necessary.
 Figure 59-5 The Pavlik harness is a flexible brace used to hold the hips pointing towards the hip socket. This enables the child to develop socket depth. The harness is best used on a child younger than 6 months. Adapted with permission from Morrissey, R.T., & Weinstein, S.L. (Eds.). (1996). Lovell & Winter’s pediatric orthopaedics (4th Ed.). (p. 922). Philadelphia: Lippincott-Raven. |
Because early diagnosis and treatment are essential for a good outcome, the provider should have a low threshold for obtaining ultrasound in any child with an abnormal hip examination or any risk factors (eg, family history, breech presentation, twins). Even without imaging, any child who has a suspicious asymmetry of the hips or demonstrates a gait problem should be referred to an orthopaedist as early as possible.
What to Tell Parents
The most important point to emphasize is the need for long-term observation. Late manifestations of even simple hip dysplasia are unfortunately not common, so children presenting in infancy may need follow-up throughout growth. However, few if any of these children will have special needs beyond yearly or biannual examinations. Children with dysplasia may participate in normal activities without increased risk to their hips. Most treatment is geared toward preventing hip problems (such as arthritis) in adulthood, and childhood functional problems are very unusual.
Knee Disorders
ANATOMY
The knee is not just a simple hinge joint; it is complicated by rotation and translation of the components. The forces across the knee may total up to eight times the body weight in running and on stairs (Simonsen et al., 1995), so even minimal pain or dysfunction can lead to disability. The distribution of force is reliant on muscle balance, bone alignment, and the condition of the soft-tissue stabilizers (ligaments and menisci).
PHYSICAL EXAMINATION
Gait should be assessed, with attention to alignment of the feet, rotation of the legs and thighs, and angulation of the knee itself. The knee should angle slightly inward (7–10 degrees) in stance. The knee is then observed and palpated
for swelling (or effusion). Normally there is dimpling at the joint lines, so loss of these contours points to fluid in the joint space. The joint lines and bones are palpated for tenderness or bony spurs. The patella is pushed downward to rule out grind pain suggestive of cartilage injury, as described in the following section.
for swelling (or effusion). Normally there is dimpling at the joint lines, so loss of these contours points to fluid in the joint space. The joint lines and bones are palpated for tenderness or bony spurs. The patella is pushed downward to rule out grind pain suggestive of cartilage injury, as described in the following section.
Stability of the knee is tested with simple provocative maneuvers. With the knee at a 30-degree angle, the examiner must first stabilize the femur with one hand while pulling on the tibia with the other hand. The knee is then pushed inward and outward from the side to rule out varus or valgus laxity (collateral ligament injury). With the knee flexed to 90 degrees, the Drawer test is performed by pulling the tibia. The knee is then pushed back to test anterior-posterior laxity. The Lachman test for anterior cruciate instability is performed by pulling forward on the tibia with the knee at 30 degrees flexion. The examiner then needs to push inward and outward on the side of the kneecap in extension and flexion to assess patellar stability.
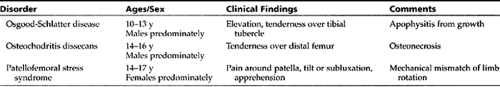
There are three major causes of nontraumatic knee pain in children (Table 59-2):
Osgood-Schlatter disease (refer to Chap. 44)
Osteochondritis dissecans (OCD) of the distal femur
Patellar disorders
▪ Osteochondritis Dissecans
PATHOLOGY
Osteochondritis dissecans is thought to represent chronic fatigue injury or disruption of the blood supply to the bone (Schenck & Goodnight, 1996). The resultant collapse of the bone directly beneath the joint surface can lead to chronic pain or mechanical symptoms, such as snapping or giving way of the knee. Seldom will the pain be severe or acute, although it may crest.
The risk of chronic cartilage damage without treatment is high, so the provider should have a low threshold for obtaining radiographs of the knee and orthopaedic referral.
EPIDEMIOLOGY
The age range of presentation is from 10 to 16 years, with boys having a higher prevalence for uncertain reasons. As is frequently the case, younger children do best clinically. Older children may have long-term chronic pain and are more likely to need surgery. Young adults may progress to arthrosis or arthritis and may need cartilage transplantation or bony reconstruction. OCD may be bilateral in up to 40% of cases (Schenck & Goodnight, 1996).
PHYSICAL EXAMINATION
The knee may show signs of generalized inflammation, including slight effusion and pain on extremes of motion, especially flexion, but will demonstrate no instability. There is tenderness at the joint line, especially over the distal end of the femur.
• Clinical Pearl
The location for findings differentiates OCD from Osgood-Schlatter disease, which is localized on the front of the tibia over the tibia tubercle and represents irritation of the growth center in that location. The provider should refer the patient to a pediatric orthopaedist for diagnosis and management of suspected OCD.
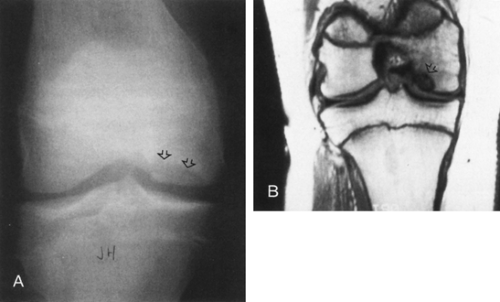
DIAGNOSTIC STUDIES
Radiographs of the knees will show a characteristic defect on the lower end of the femur, usually the lateral side of the medial femoral condyle. A rim of reactive or sclerotic bone, which indicates that the lesion is healing, may surround the area of collapsed bone. There is usually no collapse of the joint itself, except in older teens with large lesions. Figure 59-6 illustrates this finding.
• Clinical Pearl
Magnetic resonance imaging (MRI) can be helpful in assessing the extent of the lesion and the degree of cartilage involvement but is not needed for diagnosis. Radiologic studies can help the pediatric orthopaedist in determining prognosis and the need for active therapy in a given case.
MANAGEMENT
Management is normally provided by a pediatric ortho-paedist. Bracing or a short period of casting may reduce painful symptoms and help promote healing. Short-term activity modification is also frequently necessary. Surgical intervention, including arthroscopic drilling or bone or cartilage transplants, is seldom required before early adulthood.
What to Tell Parents
Many of these children will present with long-term pain that disrupts their normal activities. Emphasis should be made that a short term of bracing or modification of activity should lead to full recovery.
A small subset of children may have continuous problems, so the seriousness of this entity must be stressed. After healing of the lesion, continued exercise and fitness are important to prevent recurrence, so the child and parents should understand the level of commitment required. The provider can assist the family by referring the child to a certified athletic trainer, because this health professional specializes in health-maintaining exercise and activities. Alternatively, a physical therapist may be involved, provided he or she specializes in health and fitness.
▪ Patellofemoral Stress Syndrome
Patellofemoral stress syndrome (PFSS) is sometimes known as chondromalacia patellae (CMP). PFSS is a common disorder of teenagers, occurring late in the adolescent growth spurt and continuing into maturity. Girls are more frequently affected, possibly due to their growth-induced changing distribution of weight and muscle tone.
PATHOLOGY
The PFSS appears to arise from an imbalance in the muscles of the front of the thigh, with much stronger pull laterally than medially. This is often accentuated by residual inward rotation of the hip and a relatively externally rotated lower leg. The knee angles more inward (or valgus), leading to increased lateral pull and increased stress on the kneecap itself.
HISTORY AND PHYSICAL EXAMINATION
Although the natural history of PFSS is most often resolution of the symptoms, pain may be extreme enough to significantly limit a young teenager’s lifestyle. Fortunately, even minimal intervention may improve the symptoms.
Clinically, PFSS covers a spectrum, ranging from vague discomfort or tiredness in the knees to recurrent dislocation of the kneecap. Children with PFSS are frequently loose-jointed and very flexible.
• Clinical Pearl
On walking, the patient with PFSS will have relative external rotation of the lower leg with respect to the thigh, and the kneecap may be observed to swivel or jump at the end of extension (the so-called J-sign).
In flexion, the kneecap will be tilted laterally or even pulled to the outside by muscle forces. There may be tenderness along the borders of the kneecap with apprehension of dislocation on lateral stress. Patellar grind is frequently positive and indicates cartilage injury (or chondromalacia). Feet are generally flat and externally rotated. Hips will most frequently demonstrate increased internal rotation.
DIAGNOSTIC CRITERIA AND STUDIES
The diagnosis of CMP, which is a pathologic diagnosis, is based on clinical, radiologic, or surgical demonstration of cartilage damage.
Radiographs of the knees are not routinely ordered in the initial workup, except to differentiate OCD or Osgood-Schlatter disease. Radiographic studies may show tilt or even lateral subluxation of the kneecap in its groove. Findings can be confirmed on cross-sectional imaging studies, such as computed tomographic (CT) or MRI scans. Radiographic studies are useful for differentiating subluxation from lateral tilt and for ruling out cartilage damage. Study findings govern the treatment approach (Fulkerson, 1994).
MANAGEMENT
Treatment may often be initiated by the primary care provider. Acute-phase management should be aimed initially at reconstituting muscle balance through rest; appropriate applications of moist ice or heat (depending on response to the specific modality) for 20 to 30 minutes at a time, with a full 60 minutes elapsing before reapplying the modality; and exercise of supporting musculature. The kneecap can be centralized with bracing or taping. Referral to an athletic trainer or a physical therapist may assist the youngster in attaining a satisfactory muscle-strengthening response.
Medial shoe supports (arch supports) that will help balance the rotation of the leg segments and decompress the kneecap can be designed by either a podiatrist or an orthopaedist. If all these efforts fail, surgical rebalancing or reconstruction of the kneecap mechanism may be necessary.
• Clinical Pearl
Most adolescents will have some level of knee pain from time to time. Those whose pain chronically restricts their activity for greater than 6 months should be evaluated and treated. Referral should be made to an orthopaedist for patients who do not improve rapidly with conservative therapies or for those who have recurrent knee instability.
Delay in adequate treatment for PFSS may lead to cartilage damage (true CMP), which carries a far worse prognosis.
What to Tell Parents
Although PFSS may be very frustrating at times, it is useful to stress the overall favorable course with growth and therapeutic exercises. Again, emphasis must be placed on the need for continued exercise and fitness throughout adolescence and into adulthood.
Foot and Gait Disorders
The foot reflects muscle balance and nerve function in the infant and growing child; therefore, close attention should be paid to any deformity or perceived malformation. Fortunately, foot abnormalities either are self-limited, remodel with normal growth, or do not lead to any physical disability.
• Clinical Pearl
The provider can feel confident in recommending that a child without foot pathology can safely wear garden-variety footwear of any brand. The single most important rule is that the growing child needs to be fitted to a shoe that accommodates normal foot length, with the toes in an “uncurled” position. Generally, the shoe should allow for about one adult thumbnail length’s room at the tip of the great toe. This extra room will provide for short-term growth, while also comfortably accommodating the foot. Leather shoes are not preferable to canvas-type shoes, including those that are inexpensive.
PHYSICAL EXAMINATION
The feet should be carefully examined in the newborn nursery and in subsequent well child visits. Note should be made of the position and size of the toes. The presence or absence of a longitudinal arch may be noted, although the arch generally does not form fully until age 6 years.
The most important examination point is in assessing the flexibility of the foot, particularly rolling inward and outward of the hindfoot. Rigid abnormality of the hindfoot, whether outward into valgus or inward into varus, is most suggestive of a severe foot anomaly, such as vertical talus or clubfoot.
By walking age, the foot position during gait should be assessed. Presence of the arch in both standing and sitting positions should be noted. The alignment of the legs and thighs is very critical to the function of the knee and is best judged in ambulation. Finally, it is essential that the provider assess flexibility of the foot while making careful note of any tender or painful areas.
▪ Flatfoot
The longitudinal arch of the foot forms around age 6 years, so many children may appear to have flatfoot in early ambulation. In some children, particularly those with generalized ligamentous laxity, the flatness may persist into adulthood. Flatfoot seldom causes severe pain or functional problems, probably owing to improvements in all types of shoes. The days of the “fallen arch” syndrome seem to be past.
PHYSICAL EXAMINATION
Examination of the flatfoot is made to determine if there is a flexible arch that reappears when the foot is unloaded, as seen in Figure 59-7. The provider should note whether there is any bony tenderness suggestive of some other process. The foot should be observed in stance and with the child sitting. In true flexible flatfoot, the arch will be present when the foot is lifted off the ground. These children may show other signs of hyperlaxity, including increased hip rotation, hyperextension of the elbows, and sometimes looseness of the shoulders.
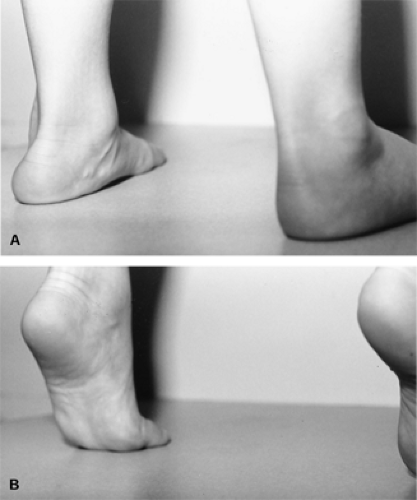 Figure 59-7 Flexible flatfoot. Note how in stance (A) the medial arch is flattened to the floor and the foot rolls outward. When the foot lifts off the ground (B), the longitudinal arch reconstitutes. Adapted with permission from Morrissey, R.T., & Weinstein, S.L. (Eds.). (1996). Lovell & Winter’s pediatric orthopaedics (4th Ed.). (p. 1086). Philadelphia: Lippincott-Raven. |
Although rare, flatfeet may be the first presenting sign of Marfan syndrome or other abnormalities of collagen and soft tissues. Therefore, the spine should be checked for scoliosis, and careful observation of limb lengths must be made. Refer to Chapter 56 for more information on Marfan syndrome.
DIAGNOSTIC STUDIES
Radiographs do not add to the diagnostic or treatment plan and are not routinely needed.
Any flatfoot that has sharp or localizing pain or is rigid may be the cause of bony pathology. In this instance, radiographs should be obtained.

Full access? Get Clinical Tree