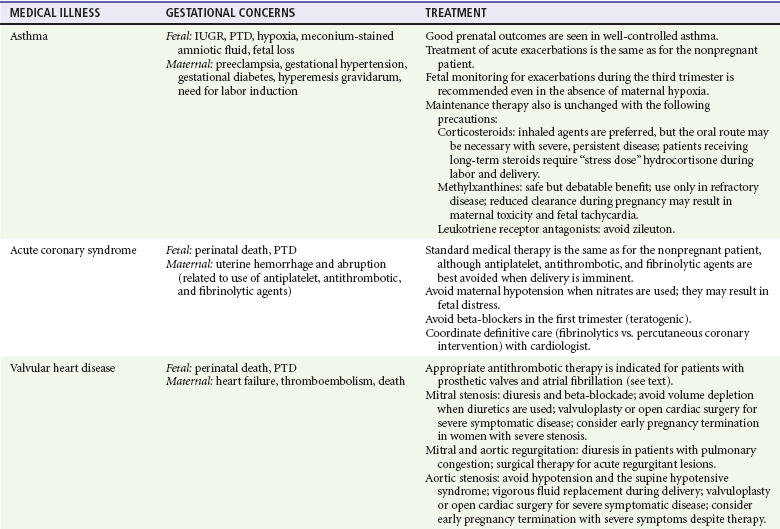
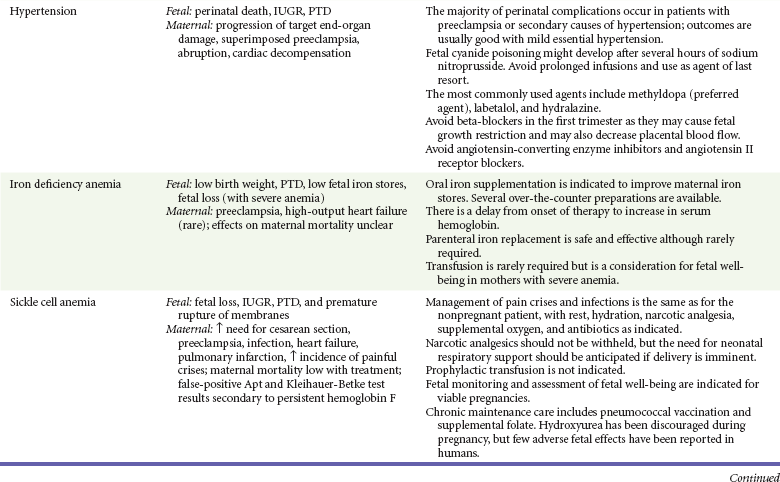
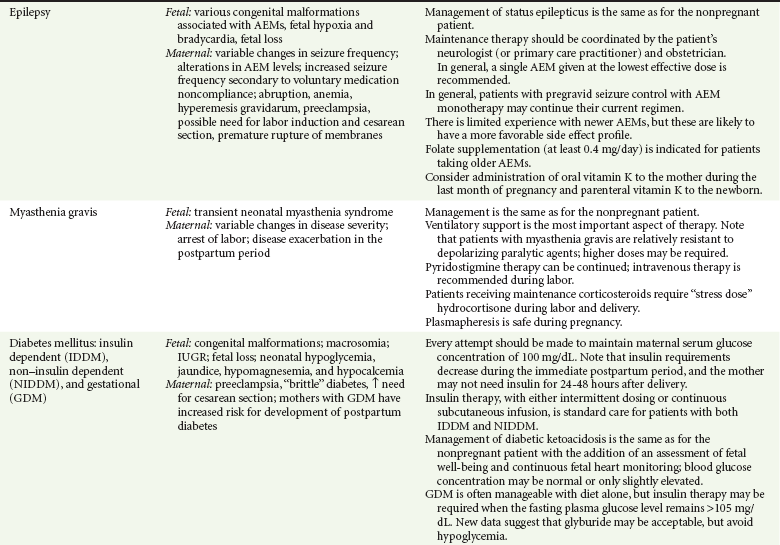
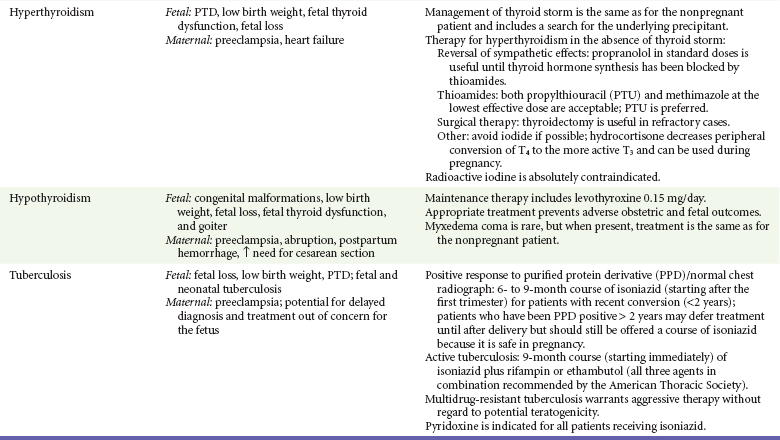
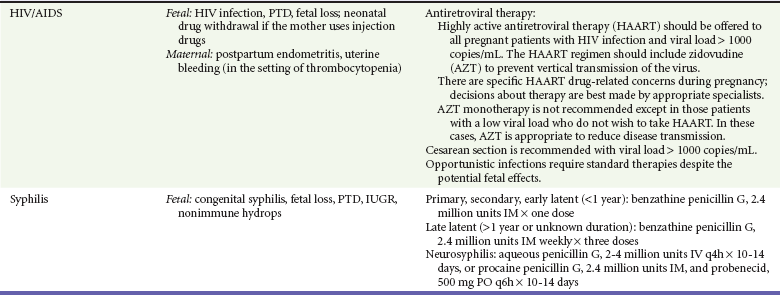
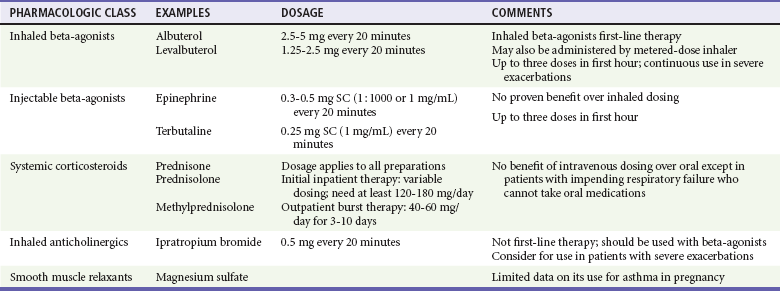
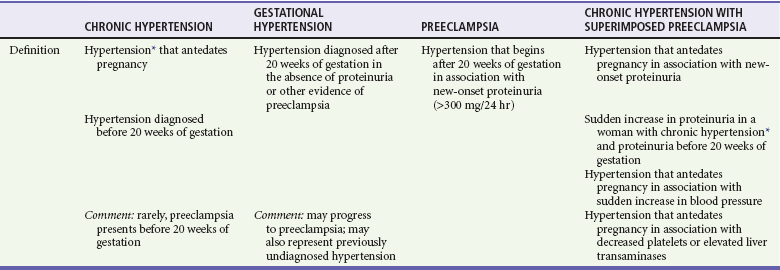
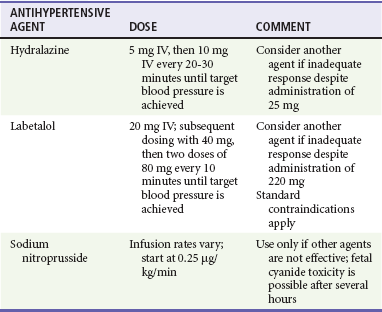
Chapter 179 Asthma is the most common pulmonary problem in pregnancy; it affects up to 8% of gestations, and the prevalence appears to be increasing.1 The overall effect of pregnancy on asthma seems to be that one third of patients will experience a worsening of the disease, one third will experience improvement, and the other third will remain unchanged.2 The exact effect of asthma on the fetus is likely to depend on the severity of disease and how well it is managed during pregnancy. Studies show that pregnant asthmatics have good perinatal outcomes in the setting of well-controlled symptoms.3–6 On the other hand, women with asthma exacerbations during pregnancy are at increased risk for complications, including congenital malformations and preterm delivery7–9 (see Table 179-1). Table 179-1 Gestational Effects and Treatment of Medical Illnesses during Pregnancy AEM, antiepileptic medicine; IUGR, intrauterine growth restriction; PTD, preterm delivery. Several changes in respiratory physiology during normal pregnancy affect the management of asthma in this context; both the tidal volume and the minute ventilation rise, increasing up to 50% by term. This increase in minute ventilation, or “hyperventilation of pregnancy,” lowers the resting PCO2 by an average of 8 to 10 mm Hg to a PCO2 of 32 mm Hg. In response to chronic hyperventilation, there is a compensatory increase in the renal excretion of bicarbonate, with serum levels averaging 19 mEq/mL (19 mmol/L). The net result is a slight respiratory alkalosis, with a serum pH ranging from 7.40 to 7.45. It is important to keep these “normal” values in mind in gauging the severity of an asthma exacerbation in the pregnant patient. Acute asthma exacerbations pose a significant maternal and fetal risk, and the pregnant patient should be managed as aggressively as the nonpregnant patient.10 The inhaled beta-agonist agents are generally considered safe in pregnancy (Tables 179-1 and 179-2). As in the nonpregnant patient, inhaled short-acting beta-agonists are first-line agents for acute asthma exacerbations.3,10 Long-acting agonists (in conjunction with inhaled corticosteroids) are also recommended for maintenance use in patients with moderate or severe disease.3,10 Selective agonists are preferred because nonselective agents such as epinephrine theoretically decrease uteroplacental blood flow through beta-mediated effects. In addition, although they are safe from a teratogenic perspective, beta-agonists are tocolytics and will usually halt active labor. Table 179-2 Drugs Used in the Treatment of Acute Asthma Exacerbations during Pregnancy Modified from National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program Asthma and Pregnancy Working Group: NAEPP Expert Panel Report. Managing asthma during pregnancy: Recommendations for pharmacologic treatment—2004 update. J Allergy Clin Immunol 115:34, 2005. Corticosteroids remain the core component for maintenance treatment of asthma in the pregnant patient. In fact, current data support the safety of inhaled corticosteroids,11 and their chronic use is recommended in all asthmatic patients except those with mild intermittent disease.3,10 Use of systemic corticosteroids is sometimes necessary on a chronic basis in patients with severe persistent asthma and as a short burst in patients with exacerbations that exhibit inadequate or poor response to initial beta-agonist therapy. The methylxanthine theophylline has been shown to be safe in pregnancy at therapeutic doses and is an acceptable alternative medication for maintenance therapy for patients with moderate to severe disease.3,10 There are limited data for cromolyn sodium, but this agent is considered class B (presumed safety) during pregnancy, and its use as an alternative agent is acceptable.10 Likewise, the leukotriene receptor antagonists (montelukast and zafirlukast) have not been widely investigated. However, an initial small study in pregnant women did not find a significant increase in adverse outcomes, and these medications are also considered class B in pregnancy.12 Magnesium sulfate has received a good deal of attention in the acute treatment of refractory asthma exacerbations because it has a wide safety profile and potent bronchodilator properties. Although large doses of magnesium have been used for the treatment of eclampsia, at this time there are insufficient data to support routine use of magnesium in this population of patients. Perhaps the most important tenet of treatment is that if the mother is hypoxic, the fetus is hypoxic as well. In addition, the fetus is more sensitive to hypoxia; thus normal maternal oxygen saturation does not preclude fetal distress. Supplemental oxygen should be administered to all pregnant patients with an acute asthma exacerbation, and assessment of fetal well-being is indicated for viable pregnancies.3 Chronic Hypertension and Hypertensive Emergencies Chronic hypertension is defined as elevated blood pressure that is present before the onset of pregnancy or that begins before the 20th week of gestation. It affects up to 7% of pregnancies and represents a significant source of maternal and fetal mortality and morbidity (see Table 179-1).13,14 The emergency physician may be required to provide therapy for hypertensive emergencies in patients with chronic hypertension and to differentiate between the various hypertensive disorders of pregnancy (Table 179-3).13–15 Table 179-3 Hypertensive Disorders of Pregnancy *Defined as blood pressure > 140 mm Hg systolic or > 90 mm Hg diastolic. Modified from Roberts JM, et al: Summary of the NHLBI Working Group on Research on Hypertension During Pregnancy. Hypertension 41:437, 2003; and the National Institutes of Health: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, Md, U.S. Department of Health and Human Services. In the treatment of chronic hypertension in pregnancy, the physician should try to balance the goal of reducing maternal blood pressure with the requirements to maintain cardiac output and to minimize adverse effects for both mother and fetus.13,14,16,17 Precipitous and marked decreases in blood pressure may significantly diminish uteroplacental blood flow. Treatment of patients with mild to moderate disease does not have an appreciable effect on perinatal outcomes, nor does it reduce the incidence of superimposed preeclampsia. In addition, these patients are likely to have a decrease in blood pressure without pharmacologic agents because of normal physiologic changes that occur in pregnancy, and they are often successfully managed without medications.13,14,17 On the contrary, patients with more severe hypertension, patients with evidence of end-organ damage, and patients taking more than one pregestational antihypertensive medication probably need maintenance medical therapy (see Table 179-1).13,17 Lifestyle modification is a potential mode of therapy, but it is unclear whether strict dietary and weight restrictions are appropriate in the gravid patient.18 Decisions about maintenance therapy are most appropriately made by the patient’s primary care practitioner in conjunction with her obstetrician. However, the emergency physician may be called on to make treatment decisions for patients with severely elevated blood pressure and for patients with superimposed eclampsia. Methyldopa remains the preferred maintenance agent, but nearly all of the major classes of antihypertensive agents are acceptable in the pregnant patient, with the exception of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers. Diuretics are considered second-line agents because of concerns about plasma volume constriction (see Table 179-1).13,14,15,17 Hydralazine and labetalol are the agents most commonly used for hypertensive emergencies associated with eclampsia and are also appropriate for such emergencies in the patient with chronic hypertension. Sodium nitroprusside can cause fetal cyanide toxicity after several hours of infusion and is considered a second-line agent (Table 179-4).13,17 Table 179-4 Antihypertensive Agents for Hypertensive Emergencies From the National Institutes of Health: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, Md, U.S. Department of Health and Human Services; August 2004. NIH Publication No. 04-5230. Patients with chronic hypertension are more likely to have preeclampsia, a situation that results in increased morbidity and mortality compared with either process in isolation. Coexistence of the two disorders should be suspected in the following situations: (1) new onset of proteinuria after 20 weeks of gestation in a patient with known hypertension and (2) pregnant patients with hypertension and proteinuria before 20 weeks of gestation who have thrombocytopenia, increased transaminase levels, or an acute increase in proteinuria or blood pressure (see Table 179-3).18 The cardiovascular changes associated with pregnancy and delivery are poorly tolerated in patients with pulmonary hypertension. Data for pregnancy in women with pulmonary hypertension are generally limited to case series, but maternal mortality rates have classically been reported to range from 30 to 56%, depending on the underlying cause (primary pulmonary hypertension, secondary vascular pulmonary hypertension, or Eisenmenger’s syndrome). Recent case series suggest that a lower mortality rate is possible in the setting of aggressive monitoring and care, including use of prostacyclin analogues and phosphodiesterase inhibitors.19,20 Unfortunately, however, a recent literature review shows that mortality remains unacceptably high (17-33%).21 Coronary artery disease is rare in pregnant women; a population-based study noted a diagnosis of acute myocardial infarction (AMI) in up to 6.2 per 100,000 deliveries.22 Prior mortality rates were reported to be approximately 20%, but more recent studies reveal rates ranging from 5 to 11%.22–24 Normal physiologic changes of pregnancy, such as increased cardiac output and reduced oxygen-carrying capacity secondary to physiologic anemia, have the potential to exceed the threshold for angina if a fixed coronary artery stenosis is present. Certain conditions are also associated with an increased risk of pregnancy-related AMI, including advanced maternal age, thrombophilia, hypertensive disorders, anemia, diabetes mellitus, and tobacco use.22,23 A review found that comorbid conditions such as tobacco use and diabetes are relatively common in gravid patients with AMI.24 AMI can occur anytime during the gestational period but peaks during the last trimester and peripartum period.22,23 Because increases in cardiac output peak during labor and delivery, maternal mortality from AMI is higher in the intrapartum period than during the antepartum or postpartum period.23,24 There are a number of potential causes of AMI in pregnant women. Despite their relatively young age, a review found that only 13% of gravidas with AMI have normal coronary arteries.24 Other pathophysiologic mechanisms besides atherosclerosis that cause AMI in the pregnant patient include coronary artery dissection, vasospasm, and coronary artery thrombosis in otherwise normal vessels. The relative significance of these lesions varies according to the gestational period. Atherosclerotic disease causes the majority of AMIs in the antepartum period, whereas coronary artery dissection is the most common causative lesion during the intrapartum and postpartum stages.24 Pulmonary embolus, reflux esophagitis, biliary colic, and aortic dissection are all more common than myocardial ischemia during pregnancy and need to be considered in the differential diagnosis. Unfortunately, some women continue to use illicit drugs during their pregnancy, and it is important to consider cocaine use in the pregnant patient presenting with chest pain. The diagnosis of acute coronary syndrome is similar to that in nonpregnant patients with certain exceptions. Electrocardiographic changes sometimes occur in normal pregnancies and delivery. These include T wave flattening and T wave inversion (mainly in lead III) and nonspecific ST changes during pregnancy as well as ST depression during labor induction for cesarean section.24 As a result, additional evaluation may be necessary. Echocardiography is useful in correlation of suspicious electrocardiographic findings with wall motion abnormalities. The enzymatic diagnosis of myocardial infarction is unchanged except during and immediately after delivery, when troponin is preferred to creatine kinase, which rises above baseline during this time. Angiography is appropriate in high-risk patients with acute coronary syndrome but is generally avoided in low-risk and stable gravidas.24 There have been reported cases of dissection resulting from percutaneous intervention during pregnancy.24 Radionuclide studies carry a lower radiation risk than does angiography but are also generally avoided in stable and low-risk patients. Treatment of AMI during pregnancy is similar in most respects to treatment of the nonpregnant patient. Survival of the mother is the primary concern, and therapy to improve maternal outcome should not be withheld. Standard treatment includes antiplatelet agents, nitroglycerin, beta-blockers, and antithrombotic agents. However, there are potential adverse effects of such therapy on the mother and fetus (see Table 179-1), and emergent consultation with a cardiologist is recommended. Regarding antiplatelet agents, aspirin remains the first-line agent. There is limited experience with clopidogrel and eptifibatide, but both have been used successfully and are considered safe from a teratogenic standpoint. Heparin has long been considered the antithrombotic agent of choice in pregnant patients, but newer low-molecular-weight agents, specifically dalteparin and enoxaparin, appear to be efficacious and safe and are deemed appropriate for use.25 Heparin is preferable for patients in the late third trimester because there is a more predictable response to protamine sulfate should labor begin. Experience with thrombolytic therapy in pregnancy is extremely limited; most experience has occurred in the setting of stroke, prosthetic valve thrombosis, and massive pulmonary embolism.26,27 The majority of pregnant patients receiving tissue plasminogen activator have had favorable maternal and fetal outcomes, but most were being treated for indications other than AMI.26 Reported adverse effects have included maternal hemorrhage, maternal death, placental abruption, preterm delivery, fetal death, and fetal intracranial hemorrhage, although the causal relationship in many of these cases is unclear because neither tissue plasminogen activator nor streptokinase crosses the placenta. Because thrombolytic therapy precludes major surgery and epidural anesthesia in the hours to days immediately after administration, the emergency physician must carefully consider whether to use these agents in pregnant women who are close to term, especially if the need for cesarean delivery is anticipated. In addition, the use of thrombolytics in coronary artery dissection is not advised. Because of the lack of data and potential risks of fibrinolytics in gravidas, emergent percutaneous intervention is the treatment of choice for definitive management of AMI.24,28 In the setting of peripartum AMI, labor should be conducted with continuous monitoring of both the mother’s hemodynamic status and fetal well-being. There are benefits and risks of both vaginal and operative delivery. Cesarean section avoids prolonged exertion by the mother but subjects the patient to general anesthesia if use of antithrombotic agents precludes epidural catheter placement. In addition, surgical delivery places the patient at risk for typical postoperative complications, such as infection, hemorrhage, and thromboembolism. Therefore, assisted vaginal delivery is preferred unless there is an obstetric reason for cesarean section.24 Resolution of angina may occur during the postpartum period as physiologic demands lessen, but its occurrence during pregnancy merits a complete cardiac evaluation for acute coronary syndrome. Maternal valvular heart disease can be congenital or acquired and is one of the leading causes of nonobstetric death. Acquired valvular disease is mainly the result of rheumatic fever and endocarditis. In the United States, most cases of significant congenital heart disease are identified and corrected surgically before puberty. The ability of patients to tolerate pregnancy without significant adverse effects depends on the type and severity of the lesion. Mild to moderate lesions (New York Heart Association classes I and II) are often associated with good outcomes. On the other hand, mitral stenosis (beyond class I), advanced aortic stenosis, aortic and mitral lesions associated with moderate to severe ventricular dysfunction or pulmonary hypertension, and mechanical prosthetic valves requiring anticoagulation can result in significant maternal mortality and require directed therapy (see Table 179-1).29 Mitral Stenosis: Mitral stenosis is the most commonly encountered valvular lesion in pregnancy and is also the most important lesion to detect in early pregnancy because maternal mortality is not insignificant.30 The increased resting heart rate and stroke volume in normal pregnancy increase the pressure gradient across the mitral valve. The result is high left atrial pressures, pulmonary vascular congestion, and the symptoms and physical findings typical of left ventricular failure. Patients may also develop atrial dysrhythmias that have the potential to decrease cardiac output and worsen symptoms.30 The likelihood of maternal symptoms and worsening of cardiovascular status is directly related to the severity of disease. Pregnancy in women with mild mitral stenosis is generally well tolerated.30 In patients with symptomatic mitral stenosis, treatment is aimed at reduction of the plasma volume and slowing of the heart rate (see Table 179-1). Surgical intervention is indicated in patients with refractory symptoms despite optimal medical management and in patients with pulmonary hypertension. The preferred procedure is percutaneous balloon valvotomy, which is associated with good maternal and fetal outcomes when it is performed in experienced centers.28–30 Aortic and Mitral Regurgitation: In most cases, chronic regurgitant lesions are well tolerated during pregnancy and may even improve as the reduced systemic vascular resistance of pregnancy allows more forward and less regurgitant flow. In addition, this effect is aided by the increase in heart rate and shortened diastole that occur in pregnancy.28–30 When necessary, medical therapy consists of diuresis, digoxin, and vasodilators. Patients with acute mitral regurgitation due to ruptured chordae do not fare as well and may require surgical therapy.28–30 Aortic Stenosis: Symptomatic aortic stenosis during pregnancy usually occurs in the setting of a congenital bicuspid valve.28,29 Patients with mild to moderate aortic stenosis tend to have uncomplicated pregnancies,30,31 and conservative management is often possible. Severely symptomatic patients may need percutaneous valvotomy in an experienced institution, although this procedure is risky for both the mother and the fetus.28,29 Prosthetic Heart Valves: Anticoagulation for the pregnant patient with a prosthetic heart valve is complicated. Warfarin is considered to be contraindicated during weeks 6 through 12 of gestation, although the risk of embryopathy is likely to be low when the dose is less than 5 mg/day.28,29 In addition, because warfarin crosses the placenta, there is a risk of fetal bleeding. If warfarin is used after the first trimester, it should be replaced by a heparin compound several weeks before anticipated delivery.29,32 Neither unfractionated heparin (UFH) nor low-molecular-weight heparin (LMWH) crosses the placenta or is teratogenic, but there are problems with their use in pregnancy. The response to UFH is more unpredictable in the pregnant patient, and aggressive dosing with frequent monitoring of the activated partial thromboplastin time is indicated.32 LMWH is an acceptable alternative to UFH in pregnant patients with thromboembolic disease, but there are still only limited data on its use in the gravida with a mechanical valve.29 In addition, there is an increased incidence of valve thrombosis in the setting of inadequate dosing and monitoring of anticoagulation.32 If the practitioner elects to use LWMHs, frequent monitoring of anti-Xa levels is recommended with the goal of achieving a level of approximately 1.0 unit/mL 4 hours after injection.29,32 In addition, intravenous UFH is substituted for LMWH 24 hours before delivery in anticipation of epidural or spinal anesthesia.32 Iron Deficiency Anemia: Iron deficiency anemia is common, occurring in approximately 20 to 25% of pregnancies in industrialized countries.33 Apart from chronically low or marginal iron stores in many women, diversion of maternal iron to the fetus for development of its own RBCs and iron stores and increased maternal demand for iron exacerbate the deficiency during pregnancy. Pregnant patients are also subject to other causes of iron deficiency anemia, such as malnutrition, chronic underlying disease, and blood loss from the gastrointestinal or genitourinary tracts. Anemia in pregnancy is defined by the World Health Organization as a hemoglobin concentration of less than 11 g/dL (110 g/L). Because of physiologic dilution, this level may be slightly lower after the 25th week of gestation. The risks of adverse pregnancy outcomes (see Table 179-1) have been noted to be related to the severity of the anemia. This generally is manifested as a proportionate increase in the risk of preterm delivery and low-birth-weight babies for women with mild to moderate anemia.33–35 Severe anemia (<6 to 7 g/dL or 60 to 70 g/L), especially occurring early in pregnancy, is associated with even higher rates of preterm delivery and low birth weights as well as increased fetal mortality, abnormal fetal oxygenation, premature rupture of membranes, gestational hypertension, and reduced volume of amniotic fluid.36,37 It is currently recommended that all pregnant patients be screened for iron deficiency anemia.36 The diagnosis is most accurately made in the very early stages of pregnancy because serum ferritin, the most sensitive and specific (and preferred) test, is affected by the dilutional effect of increased plasma volume occurring later in pregnancy. After the first trimester, other blood tests performed in combination may be necessary. The use of RBC indices is not a reliable screening tool because microcytosis and hypochromia are not reliably present in pregnant patients. Other supporting laboratory evidence includes low plasma iron levels, increased free erythrocyte protoporphyrin, and elevated total iron-binding capacity. Iron supplementation with non–enteric-coated preparations is recommended to increase maternal iron stores (see Table 179-1) in women with iron deficiency,36 even though it remains unclear whether such therapy improves perinatal outcomes.38 Patients with an uncomplicated physiologic anemia who are not iron deficient can be expected to have good obstetric outcomes without therapy and do not require treatment. The use of prophylactic supplementation in women with normal hemoglobin levels (>11 g/dL or 110 g/L) and normal iron stores (ferritin > 20 mg/dL or 20 µg/L) to prevent anemia in late pregnancy remains controversial. One randomized controlled trial found that iron supplements for such women before 28 weeks of gestation did not reduce the prevalence of preterm delivery or development of anemia later in pregnancy but did result in a decreased incidence of low-birth-weight infants.39 Another trial noted no effect on iron status but found that the incidence of both preterm delivery and low birth weight was reduced in women receiving prophylactic iron.40 On the other hand, a more recent randomized controlled trial found that nonanemic women receiving oral iron supplementation were more likely to have infants small for gestational age as well as hypertension during gestation.41 Other investigators have noted that pregnant patients with hemoglobin values typically considered “normal” in the nongravid patient have an increase in adverse outcomes, and the practitioner should consider that gravid patients with hemoglobin values of 13 to 15 g/dL (130 to 150 g/L) have inadequate expansion of their plasma volume.42 Folate Deficiency Anemia: Folate deficiency is one of a number of causes of megaloblastic anemia, a condition characterized by abnormal DNA synthesis and ineffective RBC production. The incidence of folate deficiency in pregnancy is low in developed countries but remains higher in other populations. The risk for development of folate deficiency is increased in patients with multiple gestations, short interpregnancy intervals, preexisting malnutrition, hyperemesis gravidarum, malabsorption syndromes, alcoholism, and diets lacking green leafy vegetables and animal protein.36,43 Use of certain antiepileptic medications also places women at increased risk for deficiency. As is the case for iron deficiency, effects on the fetus depend on the degree of anemia; the most significant complications are neural tube defects (NTDs). Folate supplementation reduces the risk of NTDs,44,45 and oral folate supplementation with 0.4 mg daily is routinely recommended for all women during pregnancy and before conception as the requirement for this micronutrient increases during gestation.36 The American College of Obstetricians and Gynecologists recommends 1.0 mg for those women who have a known pregnancy-related deficiency of folate.36 Women at higher risk for NTDs (e.g., NTDs in prior pregnancy) are advised to take much higher doses of folate at 4 mg daily under the close supervision of their obstetrician.46 Sickle Cell Anemia: Sickle cell disease (SCD) is one of the major sources of maternal and fetal complications in the United States. The details of the pathophysiologic mechanism and genetics of SCD are discussed in Chapter 121, but it is useful to review the most common phenotypes that affect pregnancy. The sickle gene can be homozygous (hemoglobin SS or SCD), and this form of the disease is responsible for most pregnancy complications. The sickle gene can also be heterozygous with normal hemoglobin A (sickle cell trait or hemoglobin SA), in which case symptoms are rare except under extreme environmental conditions. The hemoglobin S can also be heterozygous with a large number of abnormal hemoglobins, such as hemoglobin C, several variants of thalassemia, and other rare hemoglobin variants, and each variant has its own complication profile. Of these, the most relevant in terms of pregnancy complications is hemoglobin SC. Patients with SCD are subject to many chronic medical problems secondary to a variety of pathophysiologic mechanisms, including sickling of RBCs, anemia, immunosuppression caused by autosplenectomy, and repeated transfusion. Median life expectancy is in the fifth decade for both sexes affected by SCD, and female fertility is generally unaffected, so it is likely that the emergency physician will encounter pregnant patients with the disease. Maternal complications are common in patients with SCD and include preterm labor, eclampsia, premature rupture of membranes, maternal infections, more frequent pain crises, thrombosis, and increased need for cesarean delivery.47–52 Despite these complications, the maternal mortality rate is less than 1% with current treatment.48,49,51,52 SCD also results in adverse effects on the fetus (see Table 179-1).47 Placental infarction and insufficiency are common, and the incidence of small-for-gestational-age and low-birth-weight infants is significantly increased in SCD pregnancies compared with normal controls.48–51,53 The reported perinatal mortality rate varies but is low in the setting of appropriate maternal and neonatal care.49,50,52 Management of SCD during pregnancy is similar to that of the nonpregnant patient (see Table 179-1). Folate supplementation is standard even in the nonpregnant state because of the increased turnover of RBCs, and the recommended daily dose of folate increases to 4 mg daily during pregnancy.47 The use of supplemental iron and transfusion is controversial because of the potential for iron overload. The need for therapy is best determined by the appropriate specialists after a complete analysis of relevant hematologic parameters. Transfusion or exchange transfusion is generally reserved for patients with symptomatic anemia, cardiopulmonary instability, acute chest syndrome, intrapartum hemorrhage, and preeclampsia and possibly for patients with increasingly frequent pain crises. It is also used preoperatively for anticipated blood loss in patients undergoing cesarean section.49 In general, the goal with transfusion or exchange transfusion is to lower the percentage of hemoglobin S to 40% and to achieve hemoglobin values of approximately 10 g/dL (110 g/L).47 Hydroxyurea is not recommended for use in pregnancy because of potential teratogenicity.47 The effect of pregnancy on epilepsy is variable. Most (50-76%) epileptic patients experience no change in their seizure frequency, whereas approximately 15% experience more frequent seizures.54–56 A decrease in plasma drug concentrations is expected with certain AEMs, such as phenytoin, lamotrigine, oxcarbazepine, and levetiracetam.54 This results from a number of potential pregnancy-related physiologic changes, including increased plasma volume, decreased protein binding, and increased renal clearance. In addition, some patients engage in voluntary noncompliance with medications to avoid teratogenic effects on the fetus. Although gravid patients with epilepsy may be at increased risk for cesarean section, postpartum hemorrhage, and other adverse outcomes (see Table 179-1),57 the primary complication in these pregnancies is congenital malformations.56 Of primary concern is the risk for NTDs, facial clefts, and cardiac anomalies with the older generation agents: valproate, carbamazepine, and phenytoin. There is a twofold or threefold increase in the incidence of serious congenital malformations in offspring of epileptic mothers taking these agents. The risk is greatest with valproate and is also increased with AEM polypharmacy.55,56,58,59 Of all the older agents, carbamazepine appears to be the safest for use as monotherapy.55,56,58 Controversy exists as to whether infants of epileptic patients not taking AEMs have an increased incidence of congenital malformations compared with the general population. Studies comparing these infants with infants born to mothers without epilepsy noted a similar incidence of malformations.58 Data are limited, but preliminary results suggest that the rate of congenital malformations with the newer agents lamotrigine and levetiracetam is similar to that in the general population, and these agents are being used with increased frequency in gravid patients.59–62 New-Onset Seizure: Pregnant patients may seek treatment for idiopathic new-onset seizures; however, drug toxicity or withdrawal, head injury, meningitis, stroke, and eclampsia should be considered possible causes. The most important of these is eclampsia. Patients in the immediate postictal phase often have hypertension resulting from increased sympathetic neural activity, and even those with normal pregnancies may have mild edema of the lower extremities. Consequently, urinalysis is indicated to search for proteinuria, which may be the only differentiating factor in the initial assessment of these patients. After a period of observation, elevated blood pressure in the noneclamptic patient will likely revert to normal. If the patient remains hypertensive or has other signs of eclampsia, magnesium sulfate and other agents are indicated to prevent further seizures and to control blood pressure. In patients who do not have signs of eclampsia, investigation of the cause of the seizure should proceed as with the nonpregnant patient. Status Epilepticus: Any potential cause of seizure, including eclampsia, may result in status epilepticus. Despite this, status epilepticus in pregnancy is relatively rare, and limited data are available about its occurrence and therapy. Observations from the European Epilepsy Pregnancy Registry note that status epilepticus may occur at any time during gestation and even at delivery. It may also occur in patients who have been seizure free throughout their pregnancy, and no specific risk factors for its occurrence have been identified.54 Older reports noted a high fetal and maternal mortality, but recent data support a much lower complication rate.54 Pregnant Epileptic Patient: Patients with epilepsy coming to the emergency department for unrelated reasons may be found to be pregnant. Although no immediate change in their therapeutic regimen needs to be made, these patients should be advised of the potential risk of AEMs in pregnancy and be referred to appropriate specialists. Unintentional pregnancy is seen even in patients taking oral contraceptives because AEMs can cause increased clearance of these medications, thereby reducing their efficacy. There are significant obstetric complications related to prolonged seizure activity, and long-term treatment with an AEM for most patients with seizures is warranted (see Table 179-1). Patients who have nonconvulsive seizure disorders or who are seizure free for a sufficient period before conception are candidates for nonpharmacologic observation, but this decision should be deferred to the patient’s primary physician or neurologist. Because phenytoin, carbamazepine, valproate, and possibly other AEMs interfere with folate metabolism, oral supplementation with at least 0.4 mg/day is recommended for all women of childbearing age taking these drugs as it may have some efficacy in preventing malformations associated with these agents.63 Enzyme-inducing AEMs such as carbamazepine, phenytoin, and phenobarbital have been reported to cause neonatal vitamin K deficiency and hemorrhagic complications. However, results from a prospective study of 667 neonates in 662 women taking enzyme-inducing AEMs (none of whom received antenatal vitamin K) indicate that the actual risk of hemorrhage is low and without significant relationship to AEM use.64 The American Academy of Neurology and the American Epilepsy Society note that there is inadequate evidence to determine a definitive relationship between AEM use and neonatal hemorrhage.63 The impact of pregnancy on the course of MS has been closely studied in various cohorts of women, and a pattern has emerged. As in other autoimmune diseases, the frequency and severity of exacerbations of MS improve because of the immunosuppressant effects of pregnancy. This effect is most pronounced in the third trimester. During the 3 months after delivery, the rate of relapse increases and then returns to the pre-pregnancy baseline.65 The risk of postpartum relapse is increased in those women with relapses during the pre-pregnancy year and during pregnancy. Relapses are also more likely in MS patients with higher disability at the time of pregnancy onset. On the other hand, it does not seem that postpartum relapses are related to the duration of disease or the total number of relapses before conception.65 In addition, pregnancy does not appear to have any significant long-term adverse effects on disease progression.65 In fact, pregnancies occurring after onset of MS may confer a protective effect in regard to disease course.66 MS patients with disease exacerbation are often treated with immunomodulators such as intravenous immune globulin (IVIG), corticosteroids, and interferon beta. Although concerns exist about the use of interferon during pregnancy, small studies in gravid patients have shown that use of IVIG during pregnancy and the postpartum period is safe and may decrease the relapse rate.67–69 Likewise, the use of intermittent steroids in the postpartum period may decrease the likelihood of disease relapse.70 Maternal relapse rate is unaffected by epidural anesthesia,65 and decisions about anesthesia should be based solely on obstetric considerations. Labor may be complicated by fatigue and uncoordinated voluntary motor activity in pushing, and MS patients may be more likely to require assisted vaginal delivery.71 These pregnancies may also be at increased risk for preterm delivery and small-for-gestational-age infants.72 In general, however, pregnancies in the setting of MS have outcomes similar to those in unaffected patients.71 The increased coagulability of pregnancy combined with chronic immobilization results in an increased incidence of thromboembolic disease.73 The incidence of urinary tract infection is also markedly increased as a result of neurogenic changes and the need for catheterization.73 Infections are even more likely during pregnancy74 and may progress to pyelonephritis, with the subsequent increased risk of fetal loss, prematurity, and maternal sepsis. A unique problem in the patient with SCI is the detection of the onset of labor, which may be painless and precipitous. Patients with spinal cord lesions below T10 to T12 have an intact uterine nerve supply and will experience labor pains; however, with lesions above T10, labor may be imperceptible or experienced as only mild abdominal discomfort.73 In addition, up to 85% of patients with high lesions (above T5 to T6) experience potentially life-threatening autonomic dysreflexia.75 This is manifested as severe paroxysmal hypertension, headache, tachycardia, diaphoresis, piloerection, mydriasis, and nasal congestion. Because the response is not specific to labor and may be precipitated by distention of bowel or bladder, other causes may need to be pursued as well. Pregnant patients with SCI who have these symptoms should be assessed for cervical dilation and have uterine contractions monitored. Emergency department treatment is directed at restoration of normal blood pressure with standard agents. Definitive therapy is with regional anesthesia. Both spinal anesthesia and epidural anesthesia obliterate and prevent this response and should be used as soon as possible during labor for all women with SCI.75 Because of the difficulty in detecting labor, pregnant patients with SCI are sometimes admitted for observation near term. The effect of pregnancy and the postpartum state on myasthenia gravis is unpredictable in the individual patient, but overall approximately 25 to 40% of patients experience exacerbation of disease, with the remainder having improvement or no change in disease severity.76–78 Several important pregnancy complications are associated with myasthenia gravis. Because of weight gain, anemia, and other physiologic adjustments of pregnancy that may result in fatigue, the distinction between normal pregnancy symptoms and myasthenia may be difficult. Most deliveries are accomplished vaginally without complication in adequately treated patients; assisted and surgical delivery in these women is indicated mainly for obstetric reasons rather than for specific myasthenia-related care.76,77,79 Up to 30% of neonates born to mothers with myasthenia gravis have a transient neonatal myasthenic syndrome through placental transport of acetylcholine receptor antibodies.77 The risk of neonatal myasthenia gravis is decreased in those infants born to mothers who have undergone thymectomy.77,80 Onset of neonatal myasthenia is typically within the first hours of life but may be delayed by a period of days. Manifestations include poor feeding and suck, diminished reflexes, hypotonia, and respiratory failure. As in adults, the symptoms respond to cholinesterase inhibitors, but treatment should be done in an intensive care unit setting. The duration of the syndrome depends on its severity; severely affected infants sometimes require therapy for several months.77 Fortunately, myasthenic crises during pregnancy are rare.77,78 When exacerbations do occur, treatment is no different from treatment of nonpregnant patients (see Table 179-1). Assessment of pulse oximetry, forced vital capacity, and arterial blood gas parameters will guide respiratory therapy. For patients presenting with weakness, an edrophonium (Tensilon) challenge test to distinguish myasthenic from cholinergic crisis is appropriate after initiation of appropriate ventilatory support. Standard medical treatment is continued during labor and delivery to maximize motor strength. Epidural anesthesia is also recommended to reduce pain and fatigue. Sedatives and other agents that increase fatigue are best avoided during this time. The physician should be aware that 30% of patients experience an exacerbation during the postpartum period as the protective immunosuppressant effect of pregnancy dissipates.77 In addition, puerperal infections place the patient at risk for disease exacerbation and warrant aggressive therapy.77
Chronic Medical Illness during Pregnancy
Specific Disorders
Hypertension
Pulmonary Hypertension
Cardiac Disorders
Valvular Heart Disease
Hematologic Disorders
Neurologic Disorders
Multiple Sclerosis
Spinal Cord Injuries
Myasthenia Gravis

Full access? Get Clinical Tree


Chronic Medical Illness during Pregnancy
Only gold members can continue reading. Log In or Register to continue




