- Around 10% of children have a mental disorder
- Over 5% of children are disabled
- One in 400 children is on the child protection register (or equivalent)
- Over 80% of all illnesses in childhood are managed by the family
- Around 25% of calls to NHS Direct and 10% of walk-in centre attendances involve children
- Up to 50% of infants aged <12 months and 25% of older children will attend an ED
- One in 11 children will attend a hospital outpatient clinic each year and around 1 in 12 will be admitted
Assessment of the Ill or Injured Child: the Differences Between Adults and Children
The principles of paediatric assessment are identical to those applicable to an adult. Problems arise because of the following.
The Size of Children
The variable age and hence size of children affects physiological measurements, drug doses and equipment sizes. An expected adult weight range might be 45–90 kg, i.e. a twofold difference. Children may easily vary from 3 kg to 60 kg: a 20-fold range. A factor of two is often disregarded – most adults are given a standard dose of drugs and assumed to have similar physiological parameters. A 20-fold difference is impossible to ignore; treatment must be tailored to the size of the child.
The age of a child is usually known but the weight is more difficult to ascertain. Because of this, it is important to be able to estimate a child’s weight from a knowledge of his or her age.
 Box 18.1 Estimating the Weight of a Child
Box 18.1 Estimating the Weight of a Child- Average birthweight of a full-term infant = 3.5 kg
- Weight at age 5 months = double the birthweight
- Weight at age 12 months = triple the birthweight
The Causes of Illness in Children
The conditions with which children present are different. They do not generally suffer from the degenerative diseases of adult life but have more problems with infective conditions.
The Causes of Cardiac Arrest in Children
Children usually die from hypoxia, secondary to respiratory distress or depression, or from hypovolaemia (fluid loss or maldistribution). These lead to cardiac asystole, which has a very poor prognosis. Therefore, it is vital to recognise and reverse these conditions before terminal bradycardia supervenes. Coronary artery disease, and thus ventricular fibrillation, is very uncommon in children.
The Anatomy and Physiology of Children
Children differ from adults in their body proportions. They also have a more elastic skeleton. This leads to a different pattern of injury and an airway that can be more difficult to manage. As a result of the elastic chest wall, children are far less likely to have rib fractures, although they may have severe underlying damage to the lung, liver or spleen (also → Chapter 6).
The fast metabolism and low reserves of children explain why they get ill, hypoxic, hypoglycaemic and hypothermic very quickly. However, their general health and high capacity for repair make for a speedy recovery.
The Psychology of Children
The interaction with the assessor is as variable as the age of the child. Only practice can teach the subtle parts of this relationship but those with children of their own have a distinct advantage.
IMMEDIATE ASSESSMENT AND MANAGEMENT
A – Airway
Checking for Responsiveness
The presence of a response is usually immediately obvious. If it is not then gentle shaking may establish verbal communication with an older child. The young child will respond by eye movement, cry or body posture – the mother will know.
The Child’s Airway
Children are particularly prone to airway obstruction because of the following:
- The airway has a small diameter. Its narrowest point is at the subglottis, rather than at the vocal folds as in an adult.
- The tongue and pharyngeal soft tissues are relatively bulky.
- The voice box (larynx) is more of a voice bag with a large, floppy epiglottis and pliable vocal folds. It lies more anteriorly than in an adult.
- In the submucosa of the airway there is a large amount of lymphoid tissue that can enlarge.
- The airway reflexes are particularly sensitive.
- Toddlers put things in their mouths.
- There is a high incidence of upper respiratory tract infection (URTI) in children, including several infections that target the airway.
- Children aged <6 months are compulsory nose breathers. Nasal obstruction is thus critical in this age group.
Maintenance and Protection of the Airway
The need for aids to maintain the airway is assessed on the same criteria in the child as in the adult. However, if a child’s airway is maintainable by simple manoeuvres, an oropharyngeal (Guedel) airway is best avoided. This is because retching is easily induced in children and may be followed by laryngospasm or aspiration.
 Box 18.2 Artificial Airway and Endotracheal Tube Sizes
Box 18.2 Artificial Airway and Endotracheal Tube SizesEndotracheal Intubation of Infants
The large, floppy epiglottis of the infant prevents a standard intubation technique whereby the tip of the laryngoscope is positioned in the vallecula – the angle between the base of the tongue and the anterior surface of the epiglottis. Instead, the epiglottis must be lifted forward by a laryngoscope, which is placed posterior to it.
For this reason, paediatric laryngoscopes have relatively straight blades (e.g. Seward, Soper, Robertshaw, Miller or Wisconsin blades). The Robertshaw laryngoscope, which has characteristics of both typical adult and paediatric designs, is probably the easiest to use. After the age of about 18 months, a standard adult technique can be adopted, although many anaesthetists prefer to use a straight blade for children up to the age of 5 years.
B – Breathing
Table 18.1 Normal respiratory rates and pulse rates in children
| Age (years) | Respiratory rate (breaths/min) | Heart rate (beats/min) |
| >1 | 30–40 | 110–160 |
| 1–5 | 25–30 | 95–140 |
| 5–12 | 20–25 | 80–120 |
| >12 | 15–20 | 60–100 |
Note that the heart rate is roughly four times the respiratory rate at all ages.
Very slow respiratory rates in children suggest imminent respiratory arrest or poisoning with narcotic drugs (e.g. methadone).
Oxygen Therapy
Almost all ill or injured children will benefit from high-concentration oxygen therapy. There is no need to assess risk as in adults with chronic lung disease. Only a small group of infants with duct-dependent congenital heart disease need controlled oxygen therapy.
Therapy with Brochodilators
All wheezy children should be given nebulised bronchodilators, whether or not they are known to be asthmatic. Ask the parents how much of this type of drug they have already had and look for agitation, tachycardia and tremor – the signs of overdosage. Remember, however, that these may also be signs of hypoxia.
Artificial Ventilation
Ventilation is indicated as an emergency procedure for respiratory insufficiency in a child in the same way as in an adult.
C – Circulation
Checking for a Central Pulse
The brachial or femoral pulses should be used in infants rather than the carotid pulse. The absence of a central pulse or a rate <60 beats/min in infants indicates the need to follow procedures for cardiorespiratory arrest (→ p. 151).
Cardiovascular Parameters
- Blood pressure varies with age. It can be difficult to measure in young, moving children. A useful formula is:
- Blood volume is approximately 80 mL/kg.
The ECG is rarely as helpful in making a diagnosis in children as in adults. The exception is, of course, dysrhythmias. A cardiac monitor does, however, provide constant information about the heart rate.
Important Signs of Circulatory Disturbance in Children
- Purpura (meningococcal disease).
- Dehydration – a dry non-elastic skin or sunken eyes. In infants a floppy anterior fontanelle is a useful, if late, sign of severe fluid loss. Diarrhoea and vomiting can quickly dehydrate a small child.
- Wet nappies confirm urine output in young children. As usual, the mother will know their normal state.
Access to the Circulation
The need for and site of this should be assessed carefully. There is nothing worse than looking for veins on a screaming child who is covered with bruises from previous attempts by someone else. Remember the possibility of intraosseous infusion and venous cut-down (→ Box 18.4).
 Box 18.4 Intraosseous Cannulation
Box 18.4 Intraosseous Cannulation- Mark the anteromedial tibia 2–3 cm below the tibial tuberosity or the anterolateral femur about 3 cm above the lateral femoral condyle
- Prepare the skin and insert local anaesthetic in a conscious child
- Make a small cut in the skin
- Insert the special intraosseous needle with the trochar at 90° to skin. A gentle twisting motion results in penetration of the cortex. The needle should then be fixed in the bone. A special intraosseous drill makes this procedure easier
- Remove the trochar and use a 5-mL syringe to aspirate and confirm the cannula’s position. Blood samples may be taken (although most hospital laboratories are reluctant to process them!)
- Connect an extension tube and three-way tap
- Fix the needle in position
- Give drugs or fluid in boluses from a syringe. A standard drip will not run adequately
Fluid Replacement
- Bolus fluid therapy = 20 mL/kg, repeated as necessary after further assessment. (This is reduced to 10 mL/kg for children with trauma in hospital and 5 mL/kg for children with trauma in the prehospital setting.)
- Maintenance fluid therapy:
- 4 mL/kg per h for the first 10 kg
- 2 mL/kg per h for the next 10 kg
- 1 mL/kg per h for subsequent weight.
For example, a 25-kg child needs:
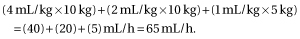
- 4 mL/kg per h for the first 10 kg
- The palm and adducted fingers of a child’s hand are approximately equal to 1% of their body surface area and can be used to make a quick estimate of the fluid replacement required for a burn (→ p. 137).
D – Disability
Level of Consciousness
AVPU scoring (→ p. 7) is as useful for children as for adults. The standard, adult Glasgow Coma Scale (GCS) is suitable for children of school age but special variants of the GCS are more appropriate in children aged <4 years (→ Box 18.5). Even sleepy children should be fairly easy to rouse.
 Box 18.5 The Children’s Coma Scale
Box 18.5 The Children’s Coma Scale| Response elicited | Score |
| Best eye response | |
| Open spontaneously | 4 |
| Open to speech | 3 |
| Open to pain | 2 |
| No response | 1 |
| Best motor response | |
| Moves normally and spontaneously or obeys commands | 6 |
| Localises pain | 5 |
| Withdraws in response to pain | 4 |
| Flexes abnormally to pain (decorticate movements) | 3 |
| Extends abnormally to pain (decerebrate movements) | 2 |
| No response | 1 |
| Best verbal response | |
| Smiles, follows sounds and objects, interacts | 5 |
| Cries consolably or interacts inappropriately | 4 |
| Cries with inconsistent relief or moans | 3 |
| Cries inconsolably or is irritable | 2 |
| No response | 1 |
Other Signs
- Agitation or an odd cry or affect may be the first signs of cerebral irritation.
- Children may be flaccid or show abnormal posturing.
- Limb movements may be unequal – sometimes this is congenital but it is best never to assume so.
E – Exposure and Environment
Comfort, warmth and the proximity of the mother or other carer are extremely important to children. Attention to these details early on can radically change the wellbeing and demeanour (and hence ease of assessment) of a child. Clothing may have to be removed to facilitate assessment. However, it must be remembered that children easily become cold and embarrassed.
F – Fits
In the apyrexic fitting child consider:
- hypoglycaemia
- meningitis
- poisoning
- cerebral oedema.
G – Glucose
Children are like fast-burning little engines and become short of oxygen and fuel very quickly. Their fuel is glucose and they have relatively low glycogen reserves.
All diabetic children will be on insulin; oral hypoglycaemic drugs are generally used only in adults. This does not mean, of course, that a child cannot take someone else’s drugs and become hypoglycaemic.
Hypoglycaemia should be corrected with 2–5 mL/kg of 10% dextrose solution (0.2–0.5 g/kg of glucose) through a large vein. Intramuscular (IM) glucagon (20 mcg/kg) is an alternative if venous access is delayed.
H – History
The initial AMPLE history (→ p. 12) should be obtained from the child or from the carers.
I – Immediate Needs of the Child
Some immediate needs will have been assessed as part of the ‘environment’. These include the provision of warmth, the removal of wet clothing and the need to ensure psychological support from the mother or other carer. A position of comfort is also mandatory; it may be life saving in conditions such as epiglottitis. As usual the relief of suffering is of paramount importance.
Assess
- The need for analgesia: exact localisation of pain is difficult in very young children but careful observation and discussion with the mother often help considerably. Analgesia can turn an unmanageable situation into a calm one. It also reassures the carers. It is far better to give analgesia freely to children who may be in pain than to withhold it on the spurious grounds that it alters conscious level or masks pupillary or abdominal signs.
- The need for limb splintage: simple limb support with troughs and pillows can be very helpful in children with limb injuries. Distal circulation should be assessed before and after positioning limbs in the same way in children as in adults.
- The tolerance of cervical and other spinal splintage: conscious children often do not tolerate this sort of restraint very well. If a collar is distressing a child significantly, it is better to remove it. The mother’s hands and pillows can be more acceptable substitutes. A child who is struggling to remove a collar is actually moving his or her neck more than a child with no splint who is lying still. The indications for spinal immobilisation are the same in children as in adults, although young children are less accurate in localising the pain of spinal injury.
Ask Yourself
Does this child need:
- drugs to relieve pain? (→ Boxes 18.6 and 18.7)
- splintage?
- freedom from splintage?
 Box 18.6 Opiate Analgesics for Children
Box 18.6 Opiate Analgesics for Children| Children aged >12 months | |
| Morphine injection | 0.1–0.2 mg/kg |
| Fentanyl injection | increments of 0.5 mcg/kg |
| Pethidine injection | 1–2 mg/kg |
| Diamorphine intranasal spray | 0.1 mg/kg |
| Morphine elixir | 0.2–0.4 mg/kg |
| Codeine elixir | 1–1.5 mg/kg |
 Box 18.7 Antipyretic Analgesics for Children
Box 18.7 Antipyretic Analgesics for ChildrenFURTHER ASSESSMENT OF THE CHILD
This will be greatly facilitated by a gentle approach and a child-friendly environment.
Additional Features in a Paediatric History
Maternal Health and Pregnancy
The health of the mother may affect the development of the fetus. Maternal infections (e.g. rubella) may lead to a damaged baby.
Birth Problems
A difficult birth (caesarean section or forceps delivery) may later manifest itself as developmental problems or fits. Was the child on the special care baby unit? If so, then the perinatal period was not as smooth as it might have been.
Siblings
The health of brothers and sisters may give useful information about a child’s illness.
Development
The continuing rapid development of a child distinguishes him or her from the adult. Questions should be asked about relationships, behaviour, play, school, sports and activities.
Immunisations
Children in the UK benefit from the existence of a planned programme of immunisations (→ Table 18.6 on p. 352). The immunisations actually received should always be ascertained.
Communication with a Child
Children vary widely in their ability to communicate. A neonate may make signals that are understood only by his or her mother whereas teenagers use the same system of communication as adults. The type and level of language used are also influenced by the child’s intelligence and environment. Consequently, communicating with a child is a difficult art, which comes more naturally to some than to others.
Questions must be pitched at the right level and the responses of the child constantly reassessed. It is obviously a mistake to phrase a question in language that a small child cannot understand. However, it is equally inappropriate to patronise an older child.
A child’s account of events can be extremely accurate. It should not be assumed that an adult’s story of events is any more credible than an older child’s.
Language Problems
Children from ethnic communities may be multilingual and revert to their domestic tongue in a crisis. Gentle rephrasing of questions may reassure them and encourage dialogue but sometimes the help of a translator is required.
The Needs of the Parents
Children usually have someone in close proximity to look after them. Sometimes the worries of these carers predominate over the symptoms of the child. Requirements vary from simple reassurance to medical interventions. The satisfactory treatment of the child often depends on the support of those closest to him or her; the child’s mental state may be inseparable from that of the mother. Parental anxiety or difficulty coping is a good reason for admitting a child to hospital.
Continuing Assessment
Assessment must continue during initial treatment and transportation. Children may change their physiological status very rapidly. It is particularly important to assess the effect of any interventions.
Monitoring must be appropriate to the child’s condition and should not replace careful observation. It needs to be considered in terms of: (1) usefulness of information obtained; and (2) acceptability to the child. In a conscious child, this probably means that:
- pulse oximetry is better than
- ECG monitoring, which is better than
- BP monitoring.
Consideration of Other Children in the Vicinity
In many situations, such as severe infections, fires, poisoning and abuse, other children may have been exposed to the same agents as the patient. In such cases, it is appropriate to assess the risk to these children also.
RESPIRATORY PROBLEMS
Respiratory disorders are responsible for around a third of all paediatric admissions to hospital in the UK.
Stridor
Stridor is a harsh respiratory noise, which is loudest in inspiration and usually indicates obstruction of the extrathoracic airways. It can be caused by:
- epiglottitis (supraglottitis)
- laryngotracheobronchitis (croup)
- bacterial tracheitis
- foreign body obstruction
- angio-oedema
- thermal, chemical or other damage to the airways
- other rarer causes of obstruction (e.g. diphtheria, quinsy, glandular fever).
Accompanying features, including the degree of respiratory distress, depend on the cause of the stridor. They may include:
- hoarseness or inability to speak
- coughing
- drooling
- sternal and subcostal recession (this is a good indicator of the degree of obstruction whereas the intensity of the stridor is not)
- tachypnoea and tachycardia
- indicators of hypoxia such as cyanosis, agitation or drowsiness.
Differences Between Epiglottitis and Croup
Despite its name, the swelling of epiglottitis usually involves more than just the bright-red, cherry-like epiglottis. It is, in fact, a complete ‘top of the larynx-itis’. This is different from the ‘bottom of the larynx-itis’ caused by croup. Spasmodic or recurrent croup is a variant form of the disease, which is more common in atopic children and is thought to have an allergic component.
Table 18.2 Differences between epiglottitis and croup
| Epiglottitis | Croup | |
| Age of child | 1–6 years | 6 months–5 years |
| Onset of symptoms | Hours | Days |
| Runny nose | No | Yes |
| Cough | Slight | Characteristic barking |
| Speech | Difficult | Hoarse |
| Stridor | Soft | Harsh |
| Able to drink | No | Yes |
| Drooling | Yes | No |
| Pyrexia | >38.5°C | <38.5°C |
| Appearance | Pale and toxic | Variable |
| Respiratory distress | Severe | Variable |
| Site affected | Supraglottis | Lower larynx and trachea |
| Causative organism | Haemophilus influenzae b | Parainfluenza and other viruses |
| Decreased incidence (since Hib vaccine) | Yes – now rare in the UK | No – still common |
| Need for observation | Yes | Yes |
| Need for intubation | Yes | Sometimes (5%) |
| Need for antibiotics | Yes | No |
| Helped by steroids | No | Yes |
XR
There is no place for radiographs in the management of stridor.
TX
- Leave the child in the position of comfort, usually sitting up and possibly on the mother’s knee.
- Avoid interventions that may precipitate crying; oxygen may sometimes be tolerated but attempts at IV access will not.
- Ask for paediatric help.
If respiratory distress accompanies the stridor, then:
- summon skilled senior help immediately, including an anaesthetist and an ENT surgeon (a consultant anaesthetist is the most appropriate grade)
- notify theatre of the situation.
Gaseous induction of anaesthesia, with a volatile agent such as sevoflurane or halothane in oxygen, followed by gentle laryngoscopy is the only appropriate treatment in the distressed child who is still breathing. Intubation should, of course, be attempted if respiratory arrest occurs.
As a holding measure, 5 mg nebulised adrenaline may be life saving (5 mL of 1 in 1000 adrenaline nebulised in oxygen) with ECG monitoring. For young children, 0.4 mL/kg of a 1 in 1000 solution of adrenaline is appropriate (up to a maximum of 5 mL). The benefit of the adrenaline only lasts for 30 min and so, in suspected croup, it should be followed immediately by nebulised or oral steroids → later.
Croup
A croup score is used in some hospitals to describe the clinical severity of the illness. It is calculated by scoring five features:
Two alternative steroid treatments have been shown to lead to marked clinical improvement in croup. Either of the following should be administered as soon as the diagnosis is suspected:
- Nebulised budesonide 2 mg (4 mL) stat or 1 mg (2 mL) repeated after 30 min
- Oral dexamethasone (0.15 mg/kg).
Oral prednisolone (1 mg/kg) is also used by some units.
Bacterial Tracheitis
Infection of the airway with staphylococci, streptococci or Haemophilus influenzae may cause bacterial tracheitis (pseudomembranous croup). The trachea contains copious purulent secretions with mucosal oedema and necrosis, features that can lead to severe airway obstruction. An affected child is unwell and toxic with a high pyrexia and stridulous breathing. Intensive care should be arranged immediately; three-quarters of such children require intubation. Antibiotic therapy should be a combination of cefotaxime and flucloxacillin.
Asthma in Children
An acute attack of asthma is one of the most common reasons for admission to a paediatric ward in the UK, although admissions for asthma have been declining rapidly over the last 5 years. Throughout western Europe, around 13% of children and over 8% of adults have asthma. These figures confirm that childhood asthma often remits in adult life. Persistence into adulthood is more likely with the following:
The first severe episode of asthma usually occurs at around 18 months of age. Attacks are often precipitated by a viral infection; in older children exercise and emotional upset may be the triggers. Asthma is an allergic bronchitis and is not primarily an infectious condition. The inflammatory process causes smooth muscle irritability, oedema and sputum retention, resulting in obstruction of the intrathoracic airways. The clinical signs of this obstructive process are:
Clinical signs correlate poorly with the severity of airway obstruction; some very ill children do not appear to be distressed.
Severe attacks
are characterised by the following:
- Child too breathless to talk or too breathless to feed (cannot complete sentences in one breath)
- Respiratory rate >50/min in children aged 2–5 years or >30/min in children aged >5 years (usually with marked recession and use of accessory muscles)
- Pulse rate >130/min in children aged 2–5 years or >120/min in children aged >5 years
- Arterial O2 saturation (SaO2) <92% on air, but any reduction in SaO2 from the normal of ≥97% must be given serious consideration.
Life-threatening features
include:
- fatigue or exhaustion
- agitation, drowsiness, confusion or a depressed level of consciousness
- cyanosis
- a silent chest
- poor respiratory efforts
- bradycardia or hypotension (bradycardia is often a preterminal sign)
- SaO2 <85% on air.
It is very useful to know what has happened during previous attacks:
- Oral steroids? How many times? For how long?
- Admission? How many times? For how long?
- Intensive care unit (ICU) admission? How many times? For how long?
Investigations:
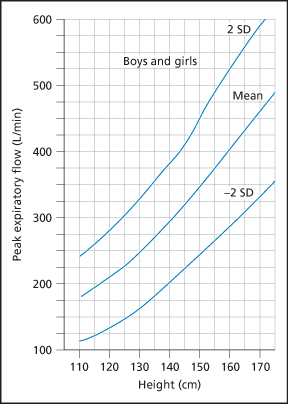
Measurement of peak expiratory flow rate (PEFR) can usually be performed on children aged >5 years provided that they are not too breathless or too distressed to cooperate. Predicted PEFRs in children → Figure 18.1. Investigations, including chest radiograph (CXR), are not generally indicated in recurrent attacks of asthma, unless there is a possible history of foreign body inhalation or severe systemic upset. Close observation and pulse oximetry are more important. The aim should be to keep the SaO2 >92%.
TX
- Nebulised salbutamol 5 mg or terbutaline 10 mg in 100% oxygen (salbutamol 2.5 mg or terbutaline 5 mg if the child is aged <5 years). The oxygen flow rate should be around 5 L/min to produce small particles without excess loss of drug from around the facemask. In children with mild-to-moderate asthma and an SaO2 >92% in air, there are some advantages in using a pressurised aerosol via a spacer device (± a facemask) to administer the β2 agonist. Ten puffs are given, one at a time, and inhaled sequentially.
- Soluble prednisolone 1 mg/kg orally (up to a maximum of 40 mg). Children who are already receiving maintenance steroid tablets should be given prednisolone 2 mg/kg (up to a maximum of 60 mg). If the child is unable to swallow liquids or is vomiting, give IV hydrocortisone 4 mg/kg. This should be repeated every 6 h or followed by a continuous infusion of hydrocortisone 1 mg/kg per h.
With life-threatening features or in a deteriorating situation get senior help, including an anaesthetist or paediatric ICU (PICU) consultant, so that intubation and ventilation can be performed if the child does not improve. (Induction of anaesthesia may be performed with bronchodilating agents such as ketamine or halothane.) Children whose SaO2 remains <92% on air after initial treatment should also be considered for PICU referral. Then consider adding:
- Nebulised ipratropium bromide 250 mcg (125 mcg if the child is aged <2 years). This may be repeated after every 20–30 min for children who are responding poorly to β2 agonists.
- Continuous nebulised β2 agonists.
- IV salbutamol 15 mcg/kg given over 10 min. This is an alternative to repeated salbutamol or terbutaline nebulisers for children aged >2 years. It is followed by a salbutamol infusion at a rate of 1–5 mcg/kg per min. ECG and electrolytes must be monitored to detect dysrhythmias and hypokalaemia.
- Magnesium sulphate 25–40 mg/kg given intravenously over 20 min (maximum dose 2 g; single dose only). Further information on magnesium → p. 250.
- Aminophylline 5 mg/kg given intravenously over 20 min under ECG control, followed by a maintenance infusion of 1 mg/kg per h in 5% dextrose. The infusion rate is reduced to 800 mcg/kg per h for children between the ages of 10 and 16 years and to 500–700 mcg/kg per h for adults. The initial loading dose should not be given to patients who are already receiving oral theophyllines.
Signs of clinical improvement include:

Full access? Get Clinical Tree