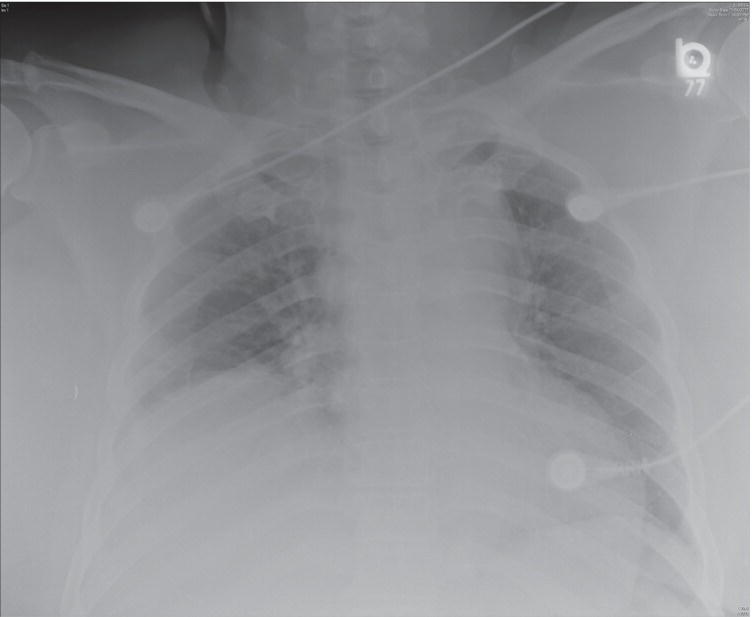
Ali S. Raja1 and Jesse M. Pines2,3 1 Department of Emergency Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA 2 US Acute Care Solutions, Canton, OH, USA 3 Department of Emergency Medicine, Drexel University, Philadelphia, PA, USA Patients with blunt chest trauma in the emergency department (ED) often require diagnostic testing to exclude potential injuries such as cardiac or pulmonary contusion, pneumothorax, hemothorax, diaphragmatic injury, rib fracture, and injury to the thoracic aorta. For patients with severe thoracic trauma, criterion standard imaging (i.e., computed tomography [CT] angiography) is often performed because, in 70–90% of cases, multiple injuries are present. There is a clinical divide between multitrauma patients and ambulatory patients with histories of blunt chest trauma and chest pain. While both groups typically receive screening chest radiography (Figure 13.1), the probabilities of clinically significant injuries in each are considerably different. When a patient is ambulatory or not severely injured, he or she can receive upright posterior–anterior and lateral chest X‐rays (CXRs). In contrast, multitrauma patients typically receive an initial supine anterior–posterior CXR because their presumed critical injuries preclude their receiving upright X‐rays safely. The initial screening supine X‐ray is less sensitive than an upright CXR for the detection of thoracic injuries, but both can be useful in guiding the initial management of patients with blunt chest trauma. Most patients in the United States with severe blunt chest trauma will receive CT scans. Which ED patients need diagnostic CXRs following blunt chest trauma? A 2006 study enrolled 507 patients with blunt chest trauma.1 The investigators’ objective was to derive a clinical decision rule able to identify blunt chest trauma patients at low risk for intrathoracic injury. The authors excluded patients <15‐years‐old and those with penetrating trauma, trauma that occurred greater than 72 hours before presentation, isolated head trauma, and Glasgow coma scale scores <14. Providers filled out surveys prior to viewing radiographic results and documented the mechanism of injury, vital signs (including oxygen saturation), patient symptoms, intoxication, distracting injuries, and the presence of visible chest wall injury, chest tenderness, pain on lateral chest compression, crepitus, and abnormal chest auscultation. Significant intrathoracic injuries were defined as pneumothoraces, hemothoraces, aortic injuries, two or more rib fractures, sternal fractures, or pulmonary contusions on blinded plain chest radiography. The prevalence of significant intrathoracic injury was 6% (31 of the 492 who had complete data). Tenderness to palpation and chest pain had the highest sensitivity (90%) as individual criterion to predict significant injuries, and hypoxia (defined as an O2 saturation <95% on room air) was the most specific (97%). The combination of tenderness to palpation and hypoxia identified all significant injuries: sensitivity 100% (confidence interval [CI] 91–100%), specificity 50% (CI 45–54%), positive predictive value 12% (CI 9–17%), and negative predictive value 100% (CI 99–100%). Figure 13.1 Chest X‐ray from a patient with a traumatic aortic injury demonstrating a wide mediastinum, blurring of the aortic arch, left apical cap, and deviation of the nasogastric tube. In a follow‐up study, the authors derived a decision rule to identify patients with blunt chest trauma with very low risk of significant intrathoracic injury who therefore do not require any chest imaging.2
Chapter 13
Chest Trauma
Background
Clinical question

Full access? Get Clinical Tree






