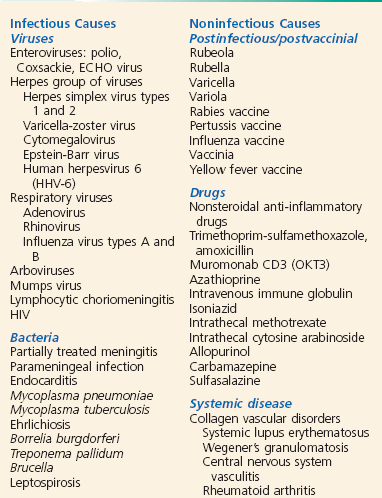
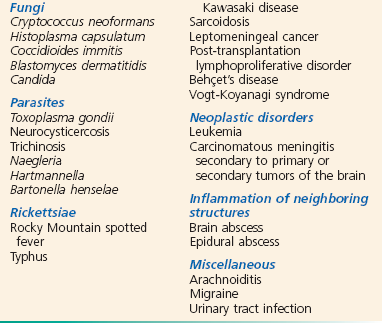
Chapter 109 Central nervous system (CNS) infections have always been among the most perplexing and devastating illnesses. “Epidemic cerebrospinal fever,” classically described by Vieusseux in 1805, was associated with almost universal mortality.1 The first American epidemic of meningococcal meningitis was recorded in 1806.2 Since that time, epidemiologic changes have occurred in concert with advances in understanding of disease processes and evolution of effective treatment strategies. Likewise, diagnostic tools have been developed that allow precise pathogen identification, most recently by molecular technologies such as polymerase chain reaction (PCR) tests for viral nucleic acids in cerebrospinal fluid (CSF). The initial treatment methods began by demonstrating the efficacy of antiserum treatment by Flexner in 1913 and of antibiotics by Colebrook and Kenny in 1936.3,4 Mortality rates in CNS infections were decreased further with the use of high-dose penicillin by Dowling and colleagues in the 1940s.5 Unfortunately, despite historical advances, the morbidity and mortality of these disorders remain considerable.6 The use of pneumococcal, Haemophilus influenzae type b, and meningococcal vaccines has led to dramatic reductions in the incidence of meningitis caused by these bacteria.7–10 This chapter focuses on the more common acute and subacute CNS infections. Infections of the nervous system with HIV or human T-lymphotropic virus, rabies virus, poliovirus, hepatitis viruses, Borrelia burgdorferi (Lyme disease), Treponema organisms (syphilis), parasites, or Rickettsia and the chronic and slow infections of the CNS (subacute sclerosing panencephalitis; progressive multifocal leukoencephalopathy; and the prion-mediated spongiform encephalopathies, such as Creutzfeldt-Jakob disease, bovine spongiform encephalopathy, and kuru) are not addressed in detail. Of note, the incidence of neurocysticercosis is on the rise in the United States.11 Bacterial meningitis is a common disease worldwide. Meningococcal meningitis is endemic in parts of Africa, and epidemics commonly occur in other countries, including the United States. A variety of other pathogens are also causative.12–16 The overall incidence of bacterial meningitis in the United States is 5 to 10 cases per 100,000 people per year.17 Men are affected more often than women are.17 Approximately 80% of cases in the United States are caused by either Streptococcus pneumoniae or Neisseria meningitidis.18 In regions where vaccination is common, the epidemiology of bacterial meningitis has substantially changed.7–10,19 The incidence of bacterial meningitis increases in late winter and early spring, but the disease may occur at any time of the year. Because most cases go unreported, the actual incidence of viral meningitis is unknown. It is estimated to affect between 11 and 27 individuals per 100,000 people.20 A prominent increase of cases is seen in summer months, which is concurrent with seasonal predominance of the enterovirus group of the picornaviruses. The same organisms responsible for viral meningitis may also be associated with encephalitis. Encephalitis is far less common, however, and the ratio of cases of meningitis to encephalitis varies according to the specific pathogen. Arbovirus infection is transmitted by an insect vector, although clinical disease develops in only a small percentage of the people bitten. Before 1999, there were approximately 19,000 hospitalizations in the United States annually for cases of encephalitis. Since then, there has been a rapid increase because of emergence of West Nile virus (WNV). In 2003, more than 8000 additional hospitalizations were required because of WNV alone.21,22 Approximately 2000 cases of brain abscess occur in the United States annually.23 Although CNS abscesses may occur at any age and any time of year, they are seen more commonly in men than in women.24 CNS abscesses are associated with local contiguous and remote systemic infections, injection drug use, neurologic surgery, and cranial trauma. Brain abscess secondary to otitis media most often occurs in pediatric or older adult populations. When brain abscess is associated with sinusitis, it most often arises among young adults. Increasingly, CNS abscesses are seen in immunocompromised patients, particularly those with HIV infection, and among bone marrow and solid organ transplant recipients. However, antimicrobial prophylaxis of immunosuppressed patients and more aggressive treatment of otitis and sinusitis have decreased the overall incidence to 0.9 per 100,000 person-years.23 Meningeal inflammation may be caused by a variety of disease processes, but the infectious causes predominate. Among the bacterial agents, Streptococcus pneumoniae remains the predominant pathogen in adult patients, followed by Neisseria meningitidis and Listeria monocytogenes.25 N. meningitidis is the predominant organism in adults younger than 45 years. Five major serogroups cause most meningococcal disease worldwide (A, B, C, Y, and W-135). Serogroup A accounts for the majority of cases of meningococcal meningitis in developing nations.26 A new vaccine for serogroup A may potentially reduce the impact of this disease in nearly half a billion individuals at risk.27 Serogroup distribution for invasive disease has changed markedly in the United States, with B, C, and Y now most commonly responsible.28 These pathogens account for the bulk of cases in nontraumatic meningitis, although virtually any organism can be encountered, particularly among patients who are elderly, alcoholic, or immunosuppressed and those who have cancer. Interestingly, higher case fatality has been observed in N. meningitidis outbreaks versus sporadic cases, probably because of increased virulence of outbreak-related strains.29 Causes of aseptic meningitis, simply defined as all cases with CSF cultures negative for bacteria, are listed in Box 109-1.30 Viral meningitis may likewise be caused by a variety of etiologic agents.31 Enteroviruses are statistically encountered most commonly.32 Unfortunately, precise identification of the etiologic agent is often impossible. Fungal and parasitic meningitides are additional concerns, particularly among immunocompromised patients.14,15 Viral meningitis secondary to herpes simplex virus (HSV) infection is actually relatively benign, especially in comparison with HSV encephalitis.33 Arboviruses and HSV, a human herpesvirus (HHV), are the most common causes of epidemic and sporadic cases of encephalitis, respectively. Children are the most vulnerable to infection with these viruses, although adults are also commonly affected. Epidemics of viral encephalitis have been attributed to a wide variety of viral agents. WNV, a flavivirus, first infected humans in the New York City area and rapidly spread to 47 states by 2003.15,34 Varicella, herpes zoster, HHV types 6 and 7, and Epstein-Barr virus have been increasingly reported to be the cause of encephalitis in immunocompetent hosts.35 Vaccinia encephalitis has been recognized in those receiving vaccination for smallpox.36 Postinfectious encephalomyelitis is also induced by a variety of viral pathogens, most commonly the measles virus.37 However, Mycoplasma pneumoniae and idiopathic causes are becoming more common in developed countries. The causes of CNS abscess are multiple and reflect the primary infective process and the immune state of the human host. A variety of mixed pathogens may be responsible for intracranial abscesses. Streptococci, particularly the Streptococcus milleri group, have been identified in nearly 50% of brain abscesses.38 Anaerobic bacteria, predominantly Bacteroides species, are commonly seen when the primary infectious process is chronic otitis media or pulmonary disease. S. aureus and Propionibacterium are often identified, particularly after cranial penetration from surgery or trauma.39 The Enterobacteriaceae are an additional common isolate. Opportunistic fungal and parasitic agents, including Nocardia species, are often seen in the immunosuppressed.40 Culture of epidural and subdural abscesses more often yields a single organism; streptococci are most commonly seen in association with contiguous spread, and S. aureus and gram-negative rods are most commonly encountered after neurologic trauma (Fig. 109-1).15 Etiologic agents in spinal abscess are similarly varied, with S. aureus being the most commonly encountered. The pathogenetic sequence in bacterial meningitis has been well characterized.14,15 The first step is nasopharyngeal colonization and mucosal invasion. Although colonization rates vary, virulent microbes use secretion of immunoglobulin A proteases and induce ciliostasis of mucosal cells. After penetration occurs by a variety of mechanisms, bacterial intravascular survival occurs because of evasion of the complement pathway. The varying capsular properties of each organism protect the bacteria. The third step occurs when the bacteria cross the blood-brain barrier to enter the CSF. The dural venous sinuses, cribriform plate area, and choroid plexus have all been implicated as potential sites of invasion. Although the mechanism of invasion is not completely understood, host defense mechanisms within the CSF are often ineffective; there are low levels of complement, immunoglobulin, and opsonic activity. Bacterial proliferation then occurs, which stimulates a convergence of leukocytes into the CSF. Meningeal and subarachnoid space inflammation is also associated with the release of cytokines into the CSF, most notably tumor necrosis factor and interleukins 1 and 6.41 This results in increased permeability of the blood-brain barrier, cerebral vasculitis, edema, and increased intracranial pressure. A subsequent decrease in cerebral blood flow leads to cerebral hypoxia. Glucose transport into the CSF is decreased concomitantly with an increased use of glucose by the brain, bacteria, and leukocytes, which depresses CSF glucose concentrations. The increased permeability leads to increased CSF proteins. Viruses enter the human host through the skin (i.e., insect vectors); through the respiratory, gastrointestinal, or urogenital tract; or by receipt of infected blood products or donor organs.42 Viral replication subsequently occurs outside the CNS, most often followed by hematogenous spread to the CNS. Additional routes into the CNS include retrograde transmission along neuronal axons and direct invasion of the subarachnoid space after infection of the olfactory submucosa.43,44 Fortunately, most systemic viral infections do not result in meningitis or encephalitis. The development and subsequent magnitude of viral infection depend on the virulence of the specific virus, the viral inoculum level, and the state of immunity of the human host. The tropism of the virus for specific CNS cell types also influences the focality of disease and its manifestations.43 Particular viruses may preferentially attack cortical, limbic, or spinal neurons, oligodendroglia, or ependymal cells. An example is the tropism of HSV for the temporal lobes and the development of temporal lobe seizures and behavioral changes in afflicted patients. Intraparenchymal brain abscesses, subdural empyema, and intracranial or spinal epidural abscesses form by inoculation of the CNS from contiguous spread of organisms from a sinus, middle ear, or dental infection or metastatic seeding from a distant site, usually from pulmonary infection, endocarditis, or osteomyelitis.45 The primary infection can be identified in 75 to 85% of cases. These conditions may also follow surgery or penetrating cranial trauma, particularly when bone fragments are retained in brain tissue. Otogenic abscesses occur most commonly in the temporal lobe in adults and the cerebellum in children, whereas sinogenic abscesses typically occur in frontal areas.38 Multiple brain abscesses suggest hematogenous spread of organisms, although solitary lesions may also occur. The pulmonary system is the most common source of hematogenous spread.15 Numerous host factors have been implicated in the acquisition of meningitis (Box 109-2).46 Although these factors alone and in combination increase the risk of meningitis, the disease often occurs in patients with none of these factors. Many patients with meningitis present with advanced disease; in these patients, the diagnosis of acute meningitis is strongly suspected. The constellation of symptoms that may classically occur in an acute CNS infection consists of fever, headache, photophobia, nuchal rigidity, lethargy, malaise, altered sensorium, seizures, vomiting, and chills.13,46 Unfortunately, more subtle presentations are also common. Immunosuppressed and geriatric patients present a diagnostic challenge because the classic signs and symptoms of meningitis may not be present. Although some degree of fever is present in most patients, as are a headache and neck stiffness, meningitis should be carefully considered in any immunosuppressed patient with symptoms or signs of infectious disease. Often, the only presenting sign of meningitis in elders is an alteration of mental status. However, a meta-analysis suggested that the absence of fever, stiff neck, and mental status change excludes meningitis in immunocompetent adults.47 A systematic review of prospective data in children found several clinical factors that were useful in influencing the likelihood of bacterial meningitis within suspected cases.48 There was no combination of factors that could rule in or rule out the disease, which is not surprising given the diversity of presentations in children. The presentation of fungal meningitis can be obscure even in the healthy adult population. Headache, low-grade fever, lassitude, and weight loss may be present but often to such a mild degree that the correct diagnosis is not initially considered.13 This is also true of tuberculous meningitis, which often has a protracted course and a vague nonspecific presentation consisting of fever, weight loss, night sweats, and malaise, with or without headache and meningismus.12 The physical findings in meningitis vary by the host, causative organism, and severity of the illness. Nuchal rigidity or discomfort on flexion of the neck is common. Kernig’s sign (the inability to straighten the leg to a position of full knee extension when the patient is lying supine with the hip flexed to a right angle) and Brudzinski’s sign (attempts to flex the neck passively are accompanied by flexion of the hips) are present in approximately 50% of adults.15 In the evaluation of patients with suspected meningitis, the sensitivity of Kernig’s sign, Brudzinski’s sign, and nuchal rigidity are 5%, 5%, and 30%, respectively, suggesting that these physical examination findings have little diagnostic value.49 Deep tendon reflexes may be increased, and ophthalmoplegia may be present, especially of the lateral rectus muscles. The systemic findings may include an obvious source of infection, such as sinusitis, otitis media, mastoiditis, pneumonia, or urinary tract infection. Various manifestations of endocarditis may be present. Arthritis may be seen with N. meningitidis and occasionally with other bacteria.46 Petechiae and cutaneous hemorrhages are widely reported with meningococcemia but also occur with H. influenzae type b, pneumococcal organisms, L. monocytogenes, and ECHO virus infections in addition to staphylococcal endocarditis.46 Endotoxic shock with vascular collapse often develops in severe meningococcal disease, but shock may be present in the advanced stages of any bacterial meningitis. Any determination of a serious systemic infection should encourage rather than dissuade the clinician from considering the possibility of a concomitant CNS infection. Patients with encephalitis may also have symptoms of meningeal irritation. An alteration of consciousness occurs in virtually all patients. Fever, headache, and a change of personality are also usually present.44 Hallucinations and bizarre behavior may precede motor, reflex, and other neurologic manifestations by several days, occasionally prompting an initial diagnosis of a psychiatric disorder. Because focal neurologic deficits and seizures occur much more commonly with encephalitis than with meningitis, there may also be diagnostic confusion with a brain abscess. It is difficult to distinguish the etiologic agent in encephalitis clinically, although HSV encephalitis results in a higher incidence of dysphasia and seizures.50 In some patients, WNV produces a myelitis that affects the anterior horn cells of the spinal column, resulting in a flaccid paralysis with a clear sensorium, similar to findings in poliomyelitis or Guillain-Barré syndrome.34 Patients with a subdural or epidural abscess most often have headache, fever, and focal signs, although more subtle presentations are common. Most of the patients with spinal abscess typically present with spinal pain and other symptoms and signs of cord compression but not necessarily with fever.51 The immediate complications of bacterial meningitis include coma (with loss of protective airway reflexes), seizures, cerebral edema, vasomotor collapse, disseminated intravascular coagulation, respiratory arrest, dehydration, syndrome of inappropriate secretion of antidiuretic hormone, pericardial effusion, and death (Box 109-3).16 Various delayed complications include multiple seizures, focal paralysis, subdural effusions, hydrocephalus, intellectual deficits, sensorineural hearing loss, ataxia, blindness, bilateral adrenal hemorrhage (Waterhouse-Friderichsen syndrome), peripheral gangrene, and death.46 The case fatality rate for pneumococcal meningitis averages 20 to 25%; higher fatality rates occur in patients with serious underlying or concomitant disease or advanced age.52 The prognosis is related to the degree of neurologic impairment on presentation. Overall, 20 to 30% of the survivors of pneumococcal meningitis have some residual neurologic deficit.46 The case fatality rate for Listeria meningitis may be as high as 40%.25 With the advent of antibiotic therapy, the mortality from meningococcal meningitis has markedly decreased to less than 20%, but it remains substantially higher in elders and those who have meningococcemia.52 Although most of the complications and sequelae are less common than with pneumococcal disease, the incidence of Waterhouse-Friderichsen syndrome is dramatically higher when meningococcemia is present.46 The overall mortality rate in community-acquired gram-negative meningitis has been less than 20% since the introduction of the third-generation cephalosporins.14 Hydrocephalus may develop in as many as 5% of patients with community-acquired meningitis; when this is present on admission, the proportion dead or with an unfavorable outcome approaches 50 to 70%.53 A delayed cerebral venous thrombosis was observed in several adults with an initially excellent recovery from pneumococcal meningitis, suggesting an immunologic vasculopathy.54 With rare exceptions, the overall prognosis for complete recovery from viral meningitis is excellent. Various complications related to the systemic effects of the particular virus include orchitis, parotitis, pancreatitis, and various dermatoses. Usually, all of these complications resolve without sequelae.31 Interestingly, HSV meningitis is often associated with the initial outbreak of genital herpes.33 The outcomes in viral encephalitis are dependent on the infecting agent. Encephalitis caused by Japanese encephalitis virus, Eastern equine virus, and St. Louis encephalitis virus is severe, with high mortality rates and virtually universal neurologic sequelae among survivors.55 WNV produces encephalitis in only 0.5% of those infected, yet it resulted in 120 deaths in 2003.22 Western equine virus and California encephalitis virus cause milder infections, and death is rare. The incidence of neurologic sequelae is highly variable and appears to depend on both the host and the infecting agent.56 Reports have emerged of influenza A H1N1 encephalitis that bears striking resemblance to “encephalitis lethargica,” reported as a complication of influenza-like illnesses in the 1920s.57 The mortality from HSV encephalitis before the use of acyclovir was 60 to 70%. Acyclovir treatment has reduced the mortality to approximately 30%.37 Common complications observed among survivors include seizure disorders, motor deficits, and changes in mentation. Death from tuberculous meningitis in the adult age group ranges from 10 to 50% of cases, with the incidence directly proportional to the patient’s age and the duration of symptoms before presentation. Focal ischemic stroke may result from the associated cerebral vasculitis. In advanced disease, up to 25% of patients may require some neurosurgical procedure for obstruction (ventriculoperitoneal shunt or drainage).58 Some neurologic deficit develops in most patients, but severe long-term sequelae among survivors are unusual.12 Common CNS complications with fungal meningitis include abscesses, papilledema, neurologic deficits, seizures, bone invasion, and fluid collections. Direct invasion of the optic nerve results in ocular abnormalities in up to 40% of patients with cryptococcal meningitis.13 The mortality rate is high but variable and is related to the timeliness of diagnosis, underlying illness, and therapeutic regimens. With the early diagnosis afforded by the use of cranial computed tomography (CT), appropriate antimicrobial therapy, and combined management approaches with surgery, aspiration, and medical therapy, the mortality rate from brain abscess has declined dramatically from approximately 50% to less than 20%.45,59 A seizure disorder is the most common complication of an intracranial abscess, occurring in 80% of patients.14 Other neurologic findings of intracranial abscesses, including focal motor or sensory deficits and changes in mentation, are common. Complications of spinal abscess primarily result from cord compression, including paralysis, motor and sensory deficits, and bowel and bladder dysfunction. Generalized spread of CNS infection and death may also occur.51 The possibility of the diagnosis of meningitis mandates lumbar puncture (LP) unless the procedure is contraindicated by the presence of infection in the skin or soft tissues at the puncture site or the likelihood of brain herniation.37 Adherence to this principle prevents a delay in diagnosis, which substantially increases the morbidity and mortality of the disease. Some patients have clinically obvious bacterial meningitis, and CSF examination serves primarily to help identify the organism, thereby facilitating the appropriate treatment. Most patients, however, present more of a diagnostic problem, and analysis of the CSF constitutes the critical step in confirming the presence of CNS infection. In most patients with bacterial meningitis, LP may be safely performed without antecedent neuroimaging studies. As this may not be the case in other brain diseases, in many circumstances it is advisable to obtain a CT scan of the head before LP is performed.60 An algorithm for diagnostic and therapeutic decision-making is presented in Figure 109-2.61 It has been conventionally asserted that LP in the presence of increased intracranial pressure may be harmful or fatal to the patient. Although data to address this concern are limited, the presence of focal neurologic signs does appear to be associated with a dramatic increase in complications associated with LP. These patients may deteriorate precipitously during or after the procedure.62–65 Patients with a markedly depressed sensorium that precludes careful neurologic examination or those with a focal neurologic deficit, papilledema, seizures, or evidence of head trauma must be considered to be at risk for a herniation syndrome that may be exacerbated by LP. If the presentation is an acute, fulminating, febrile illness and bacterial meningitis is the concerning diagnosis, early initiation of antimicrobial therapy is mandatory because of the association of prognosis and time to treatment.66 The algorithmic alternatives are therefore (1) immediate LP followed by initiation of antibiotic treatment before the results are obtained and (2) initiation of antibiotic treatment followed by a cranial CT scan and then LP. The latter choice of empirical treatment with antibiotics is now the routine in many institutions, although in some cases a third option could be considered: antibiotics and no LP despite an unremarkable CT scan.65 This reflects the efficacy of current methods of identification of causative organisms in CSF by means other than bacteriologic cultures that are less likely to be affected by antibiotic administration. The controversy emerging about not performing LP despite a lack of CT findings is based on some reviews and case reports. These describe a fulminant herniation syndrome temporally related to LP in patients with normal CT scans.63 Raised intracranial pressure may not be reliably detected by CT. Clinical signs of increased intracranial pressure, rapid change in consciousness, and recent seizures were identified as risk factors predicting deterioration despite a normal CT scan.65 The risks of ongoing empirical treatment with antibiotics without additional information from CSF analysis appears to be low as the yield from blood cultures and other diagnostic techniques such as PCR is relatively high. Therefore, this risk may be less than the risks of performing LP in certain very high-risk patients. In patients who have rapid neurologic deterioration, seizures, or signs of herniation, antibiotics should be given, a CT scan ordered, and the patient moved to intensive care. In this situation, LP may be deferred.
Central Nervous System Infections
Perspective
Definitions
Epidemiology
Principles of Disease
Meningitis
Encephalitis
Central Nervous System Abscess
Pathophysiology
Viral Meningitis and Encephalitis
Central Nervous System Abscess
Clinical Features
Complications
Viral Meningitis
Viral Encephalitis
Tuberculous Meningitis
Fungal Meningitis
Central Nervous System Abscess
Diagnostic Strategies
General Considerations
Increased Intracranial Pressure

Full access? Get Clinical Tree


Central Nervous System Infections
Only gold members can continue reading. Log In or Register to continue