CHAPTER 46
Celiac Plexus Block Using Fluoroscopic Guidance
INDICATIONS
The celiac (coeliac) plexus (CP) is a group of 1 to 5 ganglia of varying sizes that are interconnected by a dense mesh-like network of neural fibers, located in the upper abdomen, anterolateral to the aorta at the level of the first lumbar vertebrae. The CP carries afferent innervation of the upper abdominal viscera, from the distal esophagus and stomach to the mid-transverse colon, as well as the pancreas, kidneys, gall bladder, adrenals, and portions of the small bowel. CP blocks are indicated for the diagnosis and treatment of upper abdominal pain as it can be performed to help separate out visceral from somatic pains, and can be used as a treatment for chronic cancer–related pain as well as non-cancer-related pain. It is important to note that pain carried by somatic nerve fibers will not be affected when the CP is blocked.
Local anesthetic blocks, with or without steroids and alcohol neurolytic blocks are all performed. The literature is relatively clear that alcohol neurolysis is effective in reducing pain in patients with pancreatic and other upper abdominal cancers as well as retroperitoneal structures. CP blocks can be very effective when opiate therapy is causing significant side effects and can decrease the amount of opiates necessary to control pain, improves mood, and may improve life expectancy.1 The role of alcohol neurolysis in nonmalignant pancreatic pain is more controversial.
This is extremely successful in the treatment of upper abdominal cancer pain and should therefore be considered early on in the treatment algorithm.2
The indications for a celiac plexus block include:
• Treatment of visceral, poor localizing, abdominal pain, with or without malignancy
• Diagnostic block to differentiate somatic versus visceral complaints
• Pancreatic adenocarcinoma3
• Cholangiocarcinoma3
• Abdominal visceral pain syndrome
• Upper abdominal malignancies2
• Retroperitoneal malignancies
• Hepatobiliary disorders, including biliary sphincteric disorder
• Abdominal angina
• Pancreatitis, acute or chronic
RELEVANT ANATOMY
• The innervation of visceral abdominal structures largely comes from the sympathetic terminals of T5-T12.
• The preganglionic fibers leave the spine with the exiting nerve root and travel with the white communicating rami to the level of the celiac ganglion.
• The greater splanchnic nerves (T5-T9) lesser splanchnic nerves (T10-T11) and least splanchnic nerves (T11-T12) travel along the lateral border of the thoracic vertebral body and dive anterior to travel through crus of the diaphragm to become the celiac ganglion.
• The greater, lesser, and least splanchnic nerves travel together to become the celiac plexus. The celiac plexus lies anterior to the vertebral body at approximately T12 to L1, and usually lies near the takeoff of the celiac and superior mesenteric artery, which can be visualized on a preoperative computerized topography (CT) scan.
• The celiac plexus lies posterolaterally to the aorta at the level of the T12, L1 interspace on AP orientation.
• It is important to note that in a minority of patients, the artery of Adamkiewicz can leave the aorta in the low thoracic spine.
• The most important vertebrae to identify under fluoroscopic imaging are T12, L1, and L2.
Other relevant anatomy that should be taken into consideration when performing this injection is:
• Aorta
• Celiac and superior mesenteric arteries
• Anterior spinal artery (ie, the artery of Adamkiewicz)
• Adrenal glands and kidneys—located just lateral to the CP
• Diaphragm
• Renal arteries—inferiorly
• Exiting nerve roots of the lower thoracic and upper lumbar spinal cord
BASIC CONCERNS AND CONTRAINDICATIONS
The well-documented efficacy of this procedure for the treatment of pain caused by upper abdominal malignancy should direct the astute pain physician to consider this procedure early on. However, given the vast array of possible comorbidities likely suffered by a patient that could potentially benefit from a CP block, one must also consider added risk that would not typically be present in the average patient—as well as the basic risks inherent to the injection, itself.
• Immunocompromised patients are potentially at high risk of infection, this is of particular relevance in patients with malignancy.
• Patients with metastatic cancer pain may have local masses in the region.
• Patients may have thrombocytopenia secondary to chemotherapy.
• Prone position may be difficult if pain is too intense in the abdomen or if patient has abdominal distension.
• Skin breakdown from radiation treatment.
• Hypotension in a cancer patient who may already be dehydrated and hypovolemic.
Contraindications include:
• Infection, systemic or localized
• Coagulopathy
• Distorted or complicated anatomy
• Neoplasm or metastasis obstructing or potentially obstructing the intended path of the needle
• Patient refusal
PREOPERATIVE CONSIDERATIONS
• Informed consent listing the risks and proposed benefits of the procedure.
• Discontinuation of anticoagulation prior to procedure.
• Physical examination of the area of intended skin entry for infection, skin ulceration, or necrosis.
• Patient must be able to lie prone for the intended length of the procedure.
• The patient will need IV access. Pretreat with 500 to 1000 cc of lactated ringers to minimize the risk of symptomatic hypotension.
• Check for contrast allergies.
• Verify tumor anatomy.
• When alcohol is being considered for neurolysis and the patient is taking antabuse, it should be discontinued before performing an alcohol neurolysis.
• The aid of an anesthesiologist or the ability to administer sedation as it can be quite painful.
Fluoroscopic Views
• Start with an anterior-posterior (AP) image of the lumbar and lower thoracic vertebra with T12 in view and centered. The craniocaudal orientation of the C-arm should be adjusted to “square off” the vertebral bodies. The skin inferior to the T12 rib on the left side approximately 5 to 7 in lateral to the spinous process of L2 or even L3 is marked.
• Lateral view—when positioning the patient prone, the physician must take care to have the patient’s arms place toward the head so as to prevent view obstruction when obtaining lateral images. This view will allow for control of the depth and visualize the anterior advancement of the needle.
Equipment
• 22-gauge 7-in spinal needle—2 needles
• 25-gauge 1.5-in needle
• 3-cc syringe for local anesthetic
• 5-cc syringe for contrast
• 20-cc syringe for alcohol if neurolysis is to be performed
• Connector tubing (extension)
Medications
• Omnipaque 240
• 1% lidocaine with epinephrine
• 0.25% or 0.5% bupivacaine
• Occasionally steroids are added for pancreatitis
• For neurolysis—10 to 20 cc 50% to 100% alcohol
Technique
Different techniques have been advocated in the performance of the celiac plexus block. All techniques should use some type of advanced imaging in performance of the block. Fluoroscopic guidance, CT guidance, and ultrasound guidance have demonstrated to be effective. Advocates of fluoroscopic guidance point to dynamic imaging and the rapidity with which the procedure can be performed. CT guidance can be done in the prone or supine position and can demonstrate aberrant anatomy and flow of contrast more carefully. Ultrasound guidance is now being performed from a transesophageal approach, usually by the gastroenterologist, and can be done at the time of an endoscopy. The superiority of one approach over another has not been demonstrated.
We will describe here the classic retrocrural approach via fluoroscopy in the prone position using 2 needles.
Our Preferred Technique
• The patient is placed in the prone position.
• The arms are placed toward the head and out of view of lateral images.
• AP views of the lumbar and low thoracic spine are obtained.
• The skin inferior to the T12 rib on the left side approximately 5 in lateral to the spinous process of L2 or even L3 is marked. It is key that the needle is below the inferior rib of the T11 or T12 rib margin.
• The skin is then draped and prepared in a typical sterile fashion.
• The skin and deep structures are anesthetized with 1% lidocaine using the 25-gauge needle.
• A 7-in needle is advanced anterior to the aorta at the vertebral body and at the T12 L1 level taking an angled approach (Figures 46-1 and 46-2).
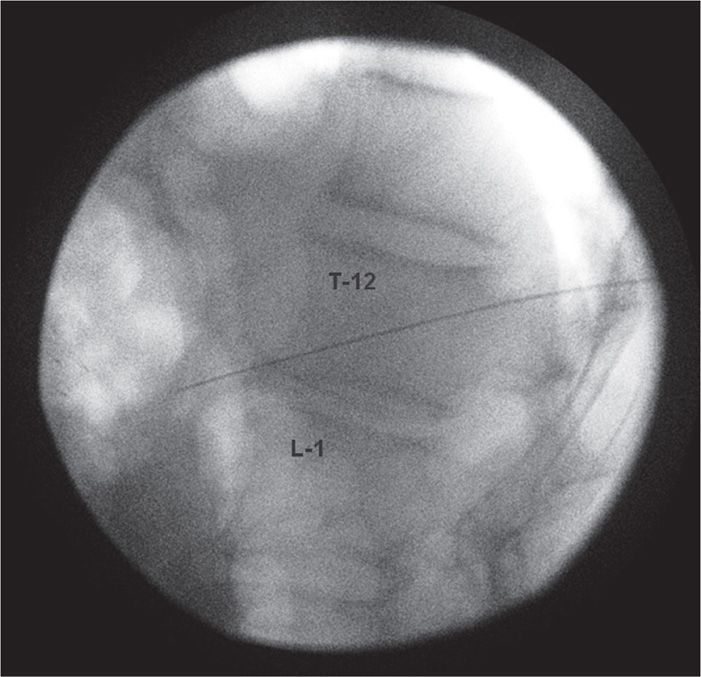
Figure 46-1. Lateral fluoroscopic image demonstrating left-sided needle advancing approximately 1 in anterior to the T12-L1 vertebral interspace for CPB. (Used with permission from Kenneth D. Candido, MD.)
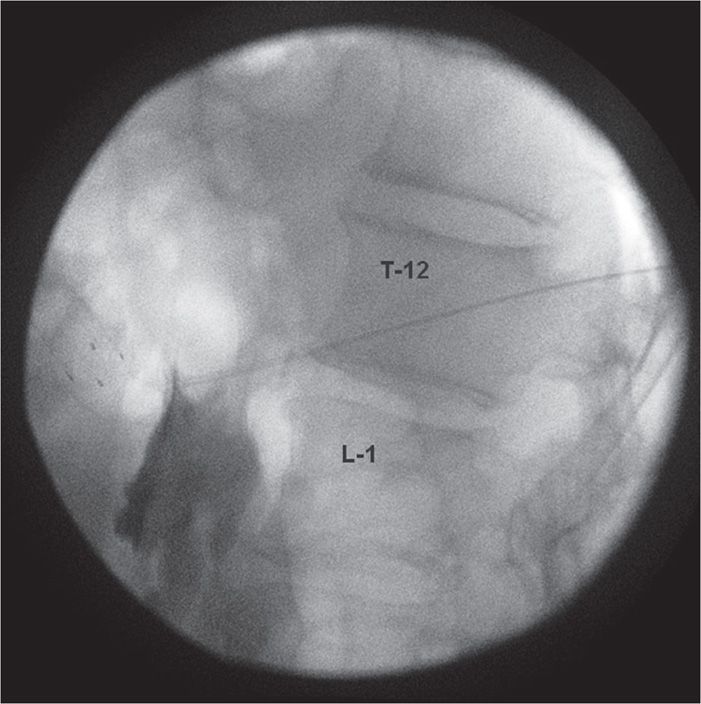
Figure 46-2. Lateral fluoroscopic image of CPB showing needle in place on the left side at T12-L1 with initiation of contrast injection demonstrating para-aortic spread. (Used with permission from Kenneth D. Candido, MD.)
• Initially the needle is placed from the left side and angled with intermittent fluoroscopic images to the region about 1 in anterior to the vertebral body at the inferior pole of the T12 level (Figure 46-3). Pulsations of the aorta can frequently be identified.
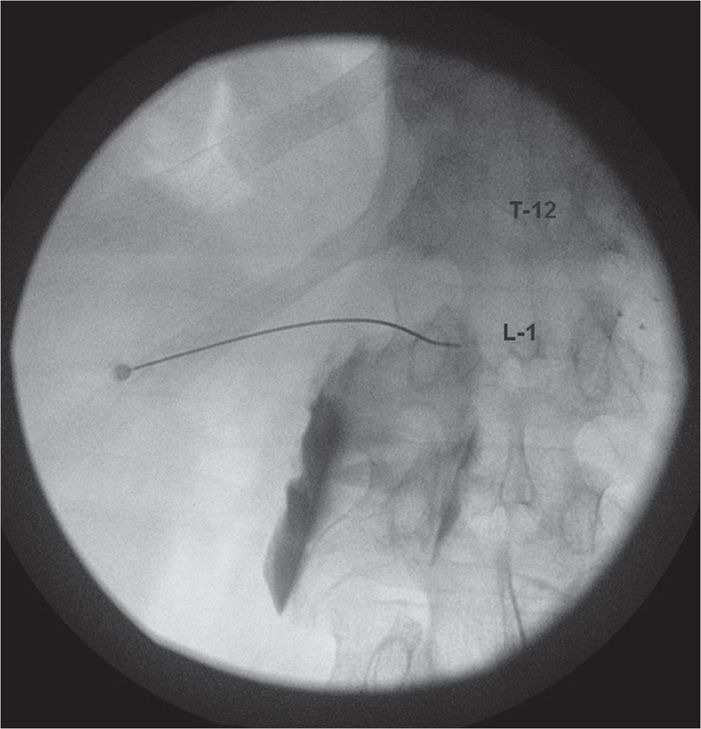
Figure 46-3. Anterior-posterior image of left-sided needle placed at T12-L1 for CPB. Initiation of contrast injection. No vascular uptake noted. Needle is curved intentionally to assist in negotiating lateral wall of the L1 vertebral body. (Used with permission from Kenneth D. Candido, MD.)
POSTPROCEDURE FOLLOW-UP
The patient should be followed into a postprocedural recovery area to ensure no immediate complications result as well as by telephone the next day (Table 46-1). The patient should be advised to call the pain service for any procedure-related complications and/or any unexpected neurological deficits or other changes. The patient should be monitored closely for the following:

Full access? Get Clinical Tree






