FIG. 47.1 Electromagnetic spectrum. (From Rothrock JC: Alexander’s care of the patient in surgery, ed 15, St. Louis, MO, 2015, Elsevier.)
Laser light differs from ordinary light in three distinct ways that make it both unique and effective in the surgical setting.1,3
1. Laser light is monochromatic, which means one color or wavelength. This pure color can determine how the laser beam reacts with certain tissues. Ordinary light, in comparison, is polychromatic, which means that it comprises a multiple array of colors or wavelengths.
2. Laser light is collimated. The light waves travel parallel to each other and do not diverge or spread. Collimation reduces the loss of power and allows for better focus and precision. Ordinary light spreads out in space as it travels away from its source.
3. Laser light is coherent. All the waves travel in an orderly manner in the same phase and direction, and all the peaks and troughs of the waves are synchronized. This coherence gives the laser beam its power. Ordinary light, in comparison, is incoherent as its waves travel out in random directions.
Tissue Interaction
Four different interactions can occur when laser energy comes into contact with human tissue (Fig. 47.2). These interactions include reflection, scattering, transmission, and absorption.3 The extent of this interaction is dependent on the wavelength of the laser, power settings, spot size, duration of exposure of the laser beam with the tissue, and the characteristics of the tissue. These interactions can have both positive and negative effects.1–3
• Reflection. Reflection occurs when the direction of the laser beam is changed after it comes into contact with a surface. This direction change can be intentional or accidental and thus can have both positive and negative effects. Mirrors can be used to intentionally reflect the laser beam to direct the beam to a hard-to-reach area. This action must be done carefully, however, to prevent an inadvertent strike and possible damage to a nontargeted area. Reflection can also occur if the laser beam hits an obstacle (e.g., a surgical instrument) and then is inadvertently reflected to another area, thus causing a tissue burn. Reflection can be either specular (direct reflection) or diffuse (scattered reflection).
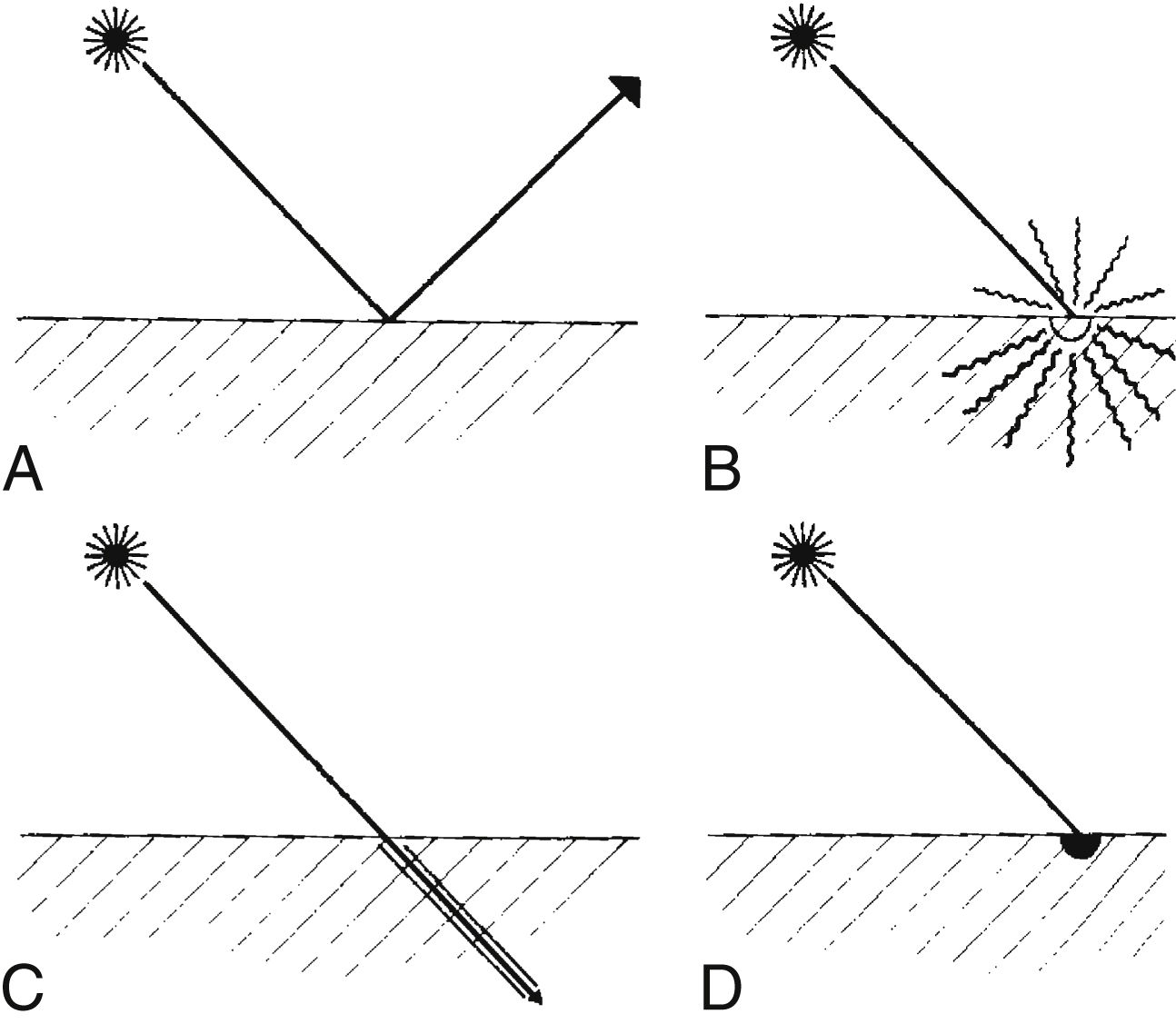
FIG. 47.2 Laser tissue interaction. A, Reflection. B, Scattering. C, Transmission. D, Absorption. (From Rothrock JC: Alexander’s care of the patient in surgery, ed 15, St. Louis, MO, 2015, Elsevier.)
• Scattering. The laser beam can also scatter as it enters certain tissues. This scattering causes the beam to disperse over a large area and weakens its strength. Backscattering can also occur as the beam scatters backward up the endoscope, thus causing damage to the operator’s eye, the endoscope optics, or the distal end of the scope.
• Transmission. Transmission occurs when the laser beam passes or is transmitted through fluids or tissue with little or no thermal effect. Transmission depends on the wavelength of the laser beam and the tissue with which it comes in contact. For example, an argon laser beam can be transmitted through the clear structures and solutions of the eye to coagulate a bleeding vessel on the retina. This action occurs because the argon energy is not absorbed by clear structures and solutions; therefore, no thermal effect is noted on these tissues.
• Absorption. Thermal effects and tissue response occur only when the tissue absorbs the energy of the laser. The amount of absorption and penetration depends on the beam’s wavelength and power, the characteristics of the contact tissue (color, consistency, and water content), the duration of the beam exposure, and the beam spot size. A thermal response can occur when tissue absorbs laser energy, thus heating the target cells. The degree of tissue change or thermal damage depends on the temperature to which the cells are heated. This temperature change is purposely regulated to affect the desired tissue response (Table 47.1).
Laser surgery can be categorized into three different types of tissue responses including thermal, mechanical, and chemical effects.3 The thermal effect, as discussed previously, is the most common laser effect as tissue is vaporized, coagulated, ablated, cut, and welded depending on the degree of thermal interaction. The mechanical (acoustic) effect from laser energy results when sound energy is created by the laser beam that disrupts tissue. The chemical effect is produced as the laser energy is used to activate a light-sensitive dye to disrupt and change tissue.
Types of Lasers
Lasers are classified by the four active mediums used to generate the laser energy: gas, solid, liquid, and semiconductor crystals. In a gas medium, electric energy is pumped through a gas, such as argon, to produce the laser energy. A solid medium uses a special rod doped with an element activated with exposure to flash lamps to create the laser energy. Liquid mediums are organic dyes that produce a wide range of wavelengths when activated with another laser beam. Semiconductor crystals are used in the medical field and in consumer products and fiberoptic communication systems. Experimental mediums that are currently being explored include free electron lasers. The actual laser name is usually derived from the active medium substance used to generate the laser energy.2,3 A summary of the various lasers currently in use can be found in Table 47.2.
Preoperative Care
Preoperative care, as with any procedure, focuses on adequate preoperative assessment and preparation of the patient. Although procedure-specific issues are addressed in other chapters, certain issues unique to laser surgery must be addressed in this discussion. One of those issues is appropriate patient selection. Procedure-specific requirements and contraindications must be evaluated.
For example, transmyocardial revascularization with the laser is generally limited to patients with advanced cardiovascular disease who have hemodynamically stable conditions and are not candidates for traditional bypass surgery. This innovative laser treatment may offer a method to revascularize the heart muscle for patients with intractable ischemic heart disease.4 Dermatologic procedures may require extensive skin preparation at home, preoperative administration of prophylactic antibiotics or antivirals, multiple treatments, and extensive postoperative skin care regimens that may last up to 1 month or more.2,5 Preoperative care must include education concerning these issues and must be used to determine whether the patient will be able to comply with the treatment regimen.
Table 47.1
Tissue Changes With Temperature Increases
| Temperature (°C) | Visual Change | BiologicAL Change |
| 37–60 | No visual change | Warming, welding |
| 60–65 | Blanching | Coagulation |
| 65–90 | White/gray | Protein denaturization |
| 90–100 | Puckering | Drying |
| >100 | Smoke plume | Vaporization, carbonization |
From Rothrock JC: Alexander’s care of the patient in surgery, ed 15, St. Louis, MO, 2015, Elsevier.)
The patient must also be prepared for expectations both during and after surgery. Many of these procedures are conducted without any anesthesia or with moderate sedation. The patient must be prepared for the sights, smells, and other sensations that will be experienced. Eye protection must be provided. Odors can include the smell of tissue vaporization. The patient may also have burning or stinging types of painful sensations with certain procedures.6
Intraoperative Issues
Intraoperative issues with laser procedures primarily concern safety. Lasers are considered a class III medical device and, as such, are subject to U.S. Food and Drug Administration jurisdiction.3 Many other regulatory, industry, and professional bodies also address the safe use of lasers. Regulations addressed include the registration of laser devices, training requirements, laser safety officer responsibilities, and safety rules.
Lasers must be further classified by the manufacturer according to their potential to cause biological harm and their inherent level of hazard. The classification system is based on the laser output power, wavelength, exposure duration, and emergent beam exposure. The classification system ranges from I to IV; the higher the class, the greater the potential hazard. Most lasers used in surgery are classified as a class IV and can damage eyes and skin and present a fire hazard.3 Because of the many provider and patient risks associated with laser use, a laser safety program should be in place in any facility in which laser procedures are conducted. This includes freestanding ambulatory facilities and physician’s offices. A laser safety committee complete with a laser safety officer should be established and responsible for guiding and overseeing all laser use in the facility. Issues that should be addressed include staff education, physician credentialing, and the monitoring of quality and safety issues. All staff involved in laser use must receive appropriate education before using or being involved in laser procedures. Topics included in these special training classes include laser biophysics, laser equipment, laser-tissue interaction, safety procedures, and clinical applications. Knowledge and skills should be verified through a competency-based credentialing program, and the skills should be reassessed and updated on a regular basis.2,3 The three most important areas of safe laser use include eye protection, smoke evacuation, and fire safety.
The eyes are susceptible to damage from laser radiation. The damage may occur acutely or may go unnoticed and develop gradually over time. The type of damage also varies with the type of laser being used. Anyone who enters an operating room or treatment area where a laser is in use (including the patient) is at risk for eye damage and, therefore, should wear protective eyewear specific to the laser in use. Filtering devices should also be placed on operative microscopes and endoscopes. The patient’s eyes should be protected with either the appropriate eyewear or moist gauze pads.2,3 The protective eyewear should have the laser wavelength that the lenses protect against inscribed on the side of the frame along with the optical density (i.e., the lenses’ filtering capabilities).2,3
Another major safety concern with the use of laser technology is the control of the smoke that the laser energy produces as it affects tissue. This surgical smoke is also called laser plume or surgical plume. Surgical smoke contains extremely small particles of vaporized tissues, toxins, and steam. If inhaled, this particulate can end up in the alveoli of surgical team members or can coat the inside lumen of unprotected suction lines if used to evacuate smoke. Even short exposure to smoke particulate and odor from toxic gases may be related to headaches, nausea, myalgia, rhinitis, conjunctivitis, and respiratory conditions and complications.2,3,7–9 In one study, perioperative nurses were shown to have twice the incidence of targeted respiratory problems, probably because of the repeated inhalation of surgical smoke.7–9 In addition, there is a high chance that surgical smoke can transmit viable pathogenic material within the plume.2,3,7
Patients are also exposed to hazards when surgical smoke is not evacuated appropriately. One classic study demonstrated that laparoscopic surgery patients can absorb the byproducts of laser tissue interaction (surgical smoke), thus increasing the level of the patient’s methemoglobin and carboxyhemoglobin. This, in turn, will decrease the oxygen-carrying capabilities of the red blood cells. The patient is absorbing the toxins produced within surgical smoke and then exhibits symptoms of headache, double vision, or nausea in the postanesthesia care area.10 When surgical smoke is properly evacuated during laparoscopy, vision of the surgical site is maintained, smoke is not absorbed by the patient, and these untoward symptoms are not routinely present in the recovering patient.
A smoke evacuation system with an ultralowpenetration air (ULPA) filter (to remove small particles) and charcoal filters (to absorb toxic gases) must be used whenever surgical smoke is generated. The smoke collection device should be positioned as close to the laser–tissue impact site as possible. All persons in the room should also wear high-filtration masks to protect against any residual plume that may have escaped capture. Surgical masks are never to be the first line of defense to protect against plume inhalation. There are smoke evacuators available today that sense surgical smoke is being generated during laparoscopy and automatically activate the system to gently evacuate the plume without destroying the pneumoperitoneum. There also are other different types of plume removal products that can be attached to the trocar sleeve to help clear the abdominal cavity of smoke without impacting the pneumoperitoneum. If any of these products requires a suction line, an in-line suction filter must be used so that plume particulate will not be drawn into the suction system. The in-line filter must be placed between the wall outlet and the suction canister to avoid pulling fluids through the filter, which would greatly alter its efficiency. Although smoke evacuation devices and supplies are available on the market today, compliance with smoke evacuation recommendations continues to be lacking.
Whenever a laser is in use, the risk of fire is also increased. A fire can be triggered any time a reflected laser beam or a direct beam comes in contact with a dry combustible item. The oxygen, anesthetic gases, and vapors from alcohol-based preparation solutions also contribute to the possible danger. All members of the laser team must be trained in fire safety and be able to respond quickly should a fire occur. All combustibles near the laser–tissue impact site should be kept wet to prevent ignition. Use of flammable draping materials and skin preparation solutions should be avoided. Sterile water or saline solution should be immediately available to douse any small fires that may occur.

Full access? Get Clinical Tree